Interstitial Lung Diseases for USMLE Step 3
Start your One-Week Free Trial
Already subscribed? Log in »
Interstitial Lung Diseases for the USMLE Step 3 Exam
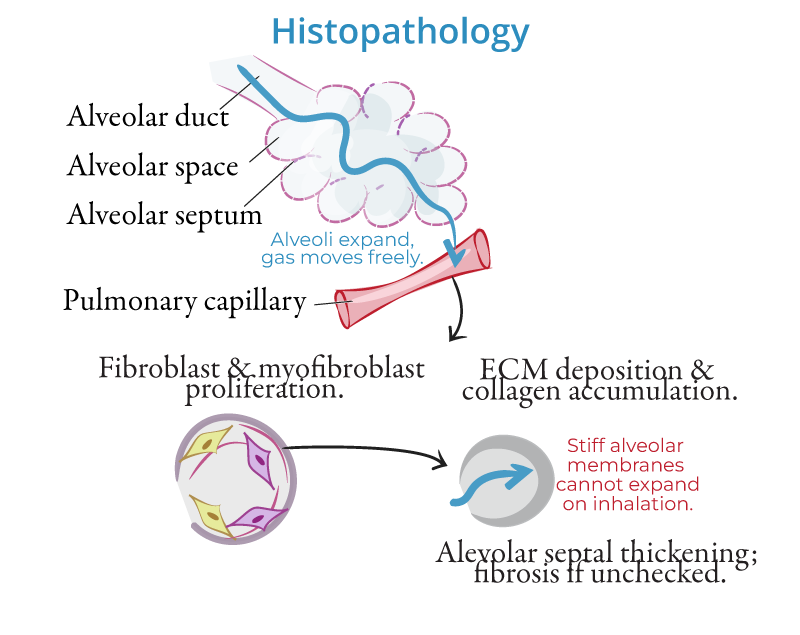
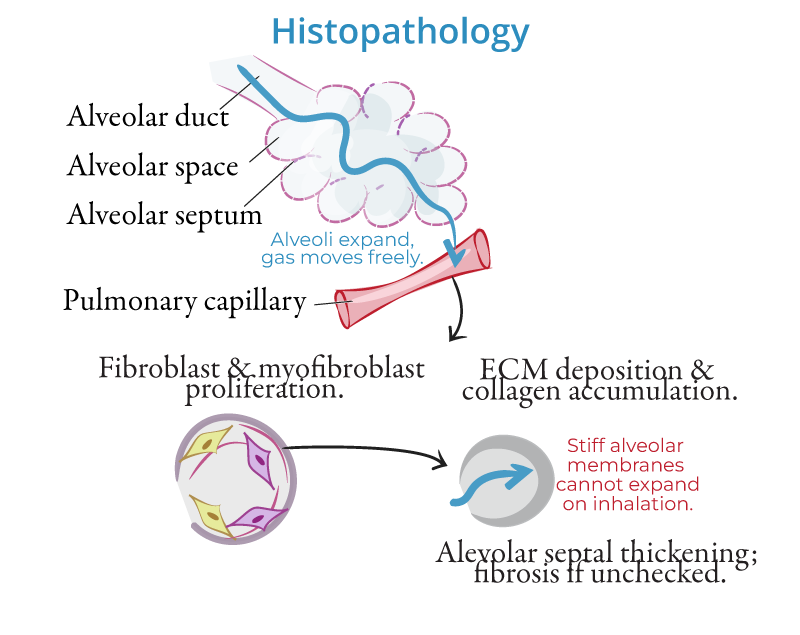
Pathophysiology
- Chronic Inflammation and Fibrosis:
- Interstitial lung diseases (ILDs) are a group of disorders characterized by chronic inflammation and fibrosis of the lung interstitium, leading to impaired gas exchange. The injury to the alveoli and surrounding tissue triggers an abnormal repair response, resulting in the deposition of excess collagen and extracellular matrix.
- Impaired Gas Exchange:
- As fibrosis progresses, the thickening of the alveolar walls restricts oxygen transfer, reducing lung compliance and causing restrictive lung disease.
- Mechanisms of Injury:
- Chronic exposure to environmental toxins, autoimmune reactions, or idiopathic processes can lead to repetitive lung injury and the activation of fibroblasts, promoting fibrosis. Inflammatory mediators like transforming growth factor-beta (TGF-β) are critical in the fibrotic process.
Etiologies
- Idiopathic Pulmonary Fibrosis (IPF):
- IPF is the most common form of ILD, particularly in older adults. It is characterized by progressive fibrosis and a poor prognosis. The hallmark histologic pattern seen in IPF is usual interstitial pneumonia (UIP).
- Pneumoconioses:
- Caused by the inhalation of inorganic dusts:
- Asbestosis: Seen in individuals exposed to asbestos, often in construction or shipyard workers.
- Silicosis: Results from inhaling silica dust, typically affecting miners and stone workers.
- Coal Workers' Pneumoconiosis: Known as black lung disease, caused by long-term inhalation of coal dust.
- Hypersensitivity Pneumonitis (HP):
- An immune-mediated reaction caused by inhalation of organic antigens (e.g., bird droppings, moldy hay). With chronic exposure, granulomatous inflammation can lead to fibrosis.
- Sarcoidosis:
- A multisystem granulomatous disorder affecting the lungs, characterized by noncaseating granulomas. It can cause fibrosis in chronic cases but has a variable course.
- Connective Tissue Diseases:
- ILD can occur in the context of autoimmune disorders, including:
- Rheumatoid arthritis (RA): Lung involvement occurs in a subset of RA patients.
- Systemic sclerosis (scleroderma): Causes diffuse pulmonary fibrosis.
Clinical Features
- Dyspnea:
- Gradual onset of progressive shortness of breath, worsened by exertion.
- Dry Cough:
- A persistent nonproductive cough is commonly seen alongside dyspnea.
- Crackles:
- Fine, inspiratory crackles are often heard on lung auscultation, particularly in the lung bases.
- Clubbing:
- Digital clubbing is seen in advanced stages, particularly in idiopathic pulmonary fibrosis (IPF).
- Systemic Symptoms:
- Extrapulmonary symptoms may include joint pain or skin changes in connective tissue disease-associated ILD.
Diagnosis
- High-Resolution CT (HRCT):
- The gold standard for ILD diagnosis. Findings vary by disease:
- Honeycombing: Seen in IPF, indicating advanced fibrosis.
- Ground-glass opacities: Seen in early inflammation (e.g., hypersensitivity pneumonitis).
- Pulmonary Function Tests (PFTs):
- Reveal a restrictive pattern with decreased total lung capacity (TLC) and forced vital capacity (FVC). The diffusion capacity for carbon monoxide (DLCO) is also reduced.
- Lung Biopsy:
- Sometimes required to confirm the diagnosis, especially when HRCT findings are inconclusive.
Management
General Approach
- Smoking Cessation:
- Smoking exacerbates lung injury and fibrosis, so cessation is critical in all patients.
- Avoidance of Triggers:
- In hypersensitivity pneumonitis, avoiding exposure to identified antigens (e.g., birds, mold) is essential for preventing further lung damage.
- Oxygen Therapy:
- Used in patients with hypoxemia to maintain oxygen saturation and improve quality of life.
Pharmacologic Therapy
- Idiopathic Pulmonary Fibrosis (IPF):
- Antifibrotic agents such as pirfenidone and nintedanib slow disease progression by inhibiting fibrotic pathways but do not reverse fibrosis.
- Corticosteroids and Immunosuppressants:
- Corticosteroids (e.g., prednisone) are used for inflammatory ILDs like hypersensitivity pneumonitis and sarcoidosis. In severe cases, immunosuppressive agents like methotrexate or azathioprine may be added.
- Pulmonary Rehabilitation:
- Structured exercise and education programs improve physical conditioning and quality of life.
Surgical Therapy
- Lung Transplantation:
- Considered in patients with end-stage ILD who have not responded to medical therapy. It significantly improves survival in carefully selected patients.
Key Points
- Interstitial lung diseases (ILDs) are characterized by chronic inflammation and fibrosis of the lung interstitium, leading to progressive dyspnea, impaired gas exchange, and restrictive lung disease.
- Major causes include idiopathic pulmonary fibrosis (IPF), pneumoconioses, hypersensitivity pneumonitis, sarcoidosis, and connective tissue diseases.
- High-resolution CT (HRCT) is the diagnostic gold standard, while pulmonary function tests show a restrictive pattern.
- Management includes antifibrotic agents for IPF, corticosteroids for inflammatory ILDs, and lung transplantation for advanced cases.
