Hemophilia for the USMLE Step 3
Start your One-Week Free Trial
Already subscribed? Log in »
Hemophilia for the USMLE Step 3 Exam
- Definition:
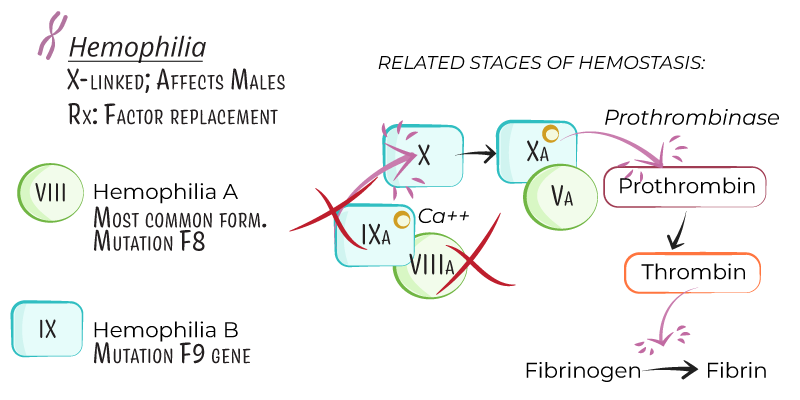
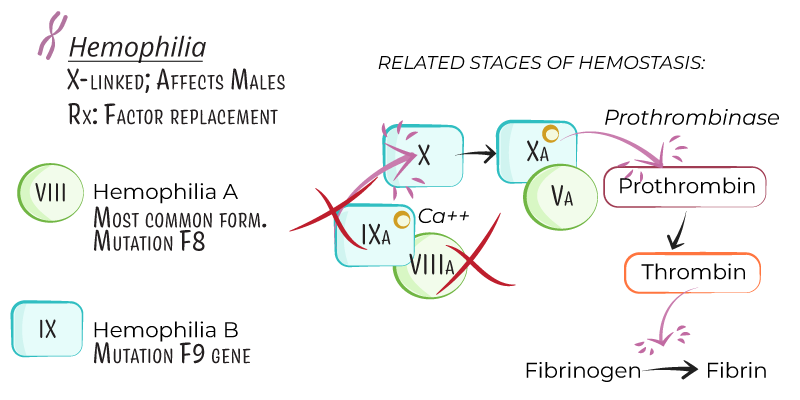
- Hemophilia is an X-linked recessive bleeding disorder due to deficiencies in specific clotting factors, leading to impaired blood coagulation.
- Hemophilia predominantly affects males, while females are typically carriers, though some may experience mild symptoms due to X-chromosome inactivation.
- Types:
- Hemophilia A: Caused by a deficiency in factor VIII, accounting for approximately 80% of cases.
- Hemophilia B (Christmas Disease): Caused by a deficiency in factor IX, representing around 20% of cases.
Genetics and Pathophysiology
- Inheritance:
- Hemophilia A and B are X-linked recessive, primarily affecting males. Carrier females have a 50% chance of passing the affected gene to sons (affected) or daughters (carriers).
- Pathogenesis:
- Factor VIII (Hemophilia A) and factor IX (Hemophilia B) are intrinsic coagulation factors essential for the activation of factor X, leading to thrombin generation and fibrin clot formation.
- Deficiency in these factors disrupts the clotting cascade, resulting in impaired clot stability and prolonged bleeding.
- Severity:
- Severe: Factor level <1% of normal, often associated with spontaneous bleeding episodes.
- Moderate: Factor level 1–5% of normal, with bleeding following mild trauma.
- Mild: Factor level 5–40% of normal, with bleeding typically only after significant trauma or surgery.
Clinical Presentation
- Bleeding Sites:
- Hemarthrosis: Repeated bleeding into joints (e.g., knees, elbows, ankles) is a hallmark of severe hemophilia and leads to joint deformity and hemophilic arthropathy if untreated.
- Muscle Bleeding: Deep muscle bleeds, especially in the thigh or iliopsoas, may lead to compartment syndrome if left untreated.
- Mucocutaneous Bleeding: Less common than in von Willebrand disease; may occur in dental procedures or minor nasal trauma.
- Intracranial Hemorrhage: Rare but life-threatening, often following head trauma.
- Postoperative or Post-Traumatic Bleeding:
- Prolonged bleeding after procedures or trauma is common, particularly in mild or moderate cases where hemophilia diagnosis may be delayed.
Diagnosis
- Laboratory Tests:
- Complete Blood Count (CBC): Usually normal but may show anemia if there is significant blood loss.
- Prothrombin Time (PT): Normal, as PT assesses the extrinsic pathway, which is unaffected by factor VIII or IX deficiencies.
- Activated Partial Thromboplastin Time (aPTT): Prolonged due to deficiency in the intrinsic pathway.
- Factor Assays: Measurement of factor VIII and IX levels confirms diagnosis and determines disease severity.
- Genetic Testing:
- Useful for carrier detection and prenatal diagnosis, especially in families with known hemophilia.
- Inhibitor Testing:
- Antibodies (inhibitors) against factor VIII or IX can develop in some patients, particularly those with severe hemophilia A, complicating treatment.
Treatment
- Factor Replacement Therapy:
- Factor VIII Concentrate (Hemophilia A) and Factor IX Concentrate (Hemophilia B):
- On-Demand Therapy: For active bleeding episodes.
- Prophylactic Therapy: Regular infusions to maintain target factor levels and prevent spontaneous bleeding, especially in severe hemophilia.
- Dosing: Based on factor deficiency, weight, and specific bleeding situation.
- Bypassing Agents for Inhibitors:
- Recombinant Factor VIIa (rFVIIa) and Activated Prothrombin Complex Concentrate (aPCC): Used in patients with high-titer inhibitors to factor VIII or IX.
- Emicizumab:
- Mechanism: A bispecific antibody that mimics factor VIII function by bridging factors IXa and X, used for prophylaxis in hemophilia A patients with or without inhibitors.
- Administration: Subcutaneous injection, generally given weekly or biweekly.
- Adjunct Therapies:
- Antifibrinolytics (e.g., tranexamic acid, aminocaproic acid): Useful for mucosal bleeding and dental procedures.
- Pain Management: Acetaminophen preferred over NSAIDs to avoid platelet inhibition.
Key Points
- Hemophilia is an X-linked recessive disorder caused by deficiencies in factor VIII (hemophilia A) or factor IX (hemophilia B), primarily affecting males.
- Disease severity (severe, moderate, mild) is based on factor levels, with severe cases often presenting with spontaneous joint and muscle bleeds.
- Diagnosis includes prolonged aPTT, specific factor assays, and genetic testing to identify carriers.
- Management includes on-demand and prophylactic factor replacement, bypassing agents for inhibitor patients, and emicizumab for prophylaxis in hemophilia A.
- Complications include joint deformities from recurrent hemarthrosis, inhibitor development, and increased bleeding risk with trauma or surgery.
