Asthma for USMLE Step 3
Start your One-Week Free Trial
Already subscribed? Log in »
Asthma for the USMLE Step 3 Exam
Pathophysiology
- Chronic Inflammation:
- Asthma is a chronic inflammatory condition involving airway hyperreactivity and reversible bronchoconstriction. Key inflammatory cells include eosinophils, mast cells, and Th2 lymphocytes, which release mediators like histamine and leukotrienes, leading to bronchospasm and edema.
- Airway Hyperresponsiveness:
- Asthmatic airways are overly responsive to various stimuli (e.g., allergens, exercise, cold air), resulting in exaggerated bronchoconstriction.
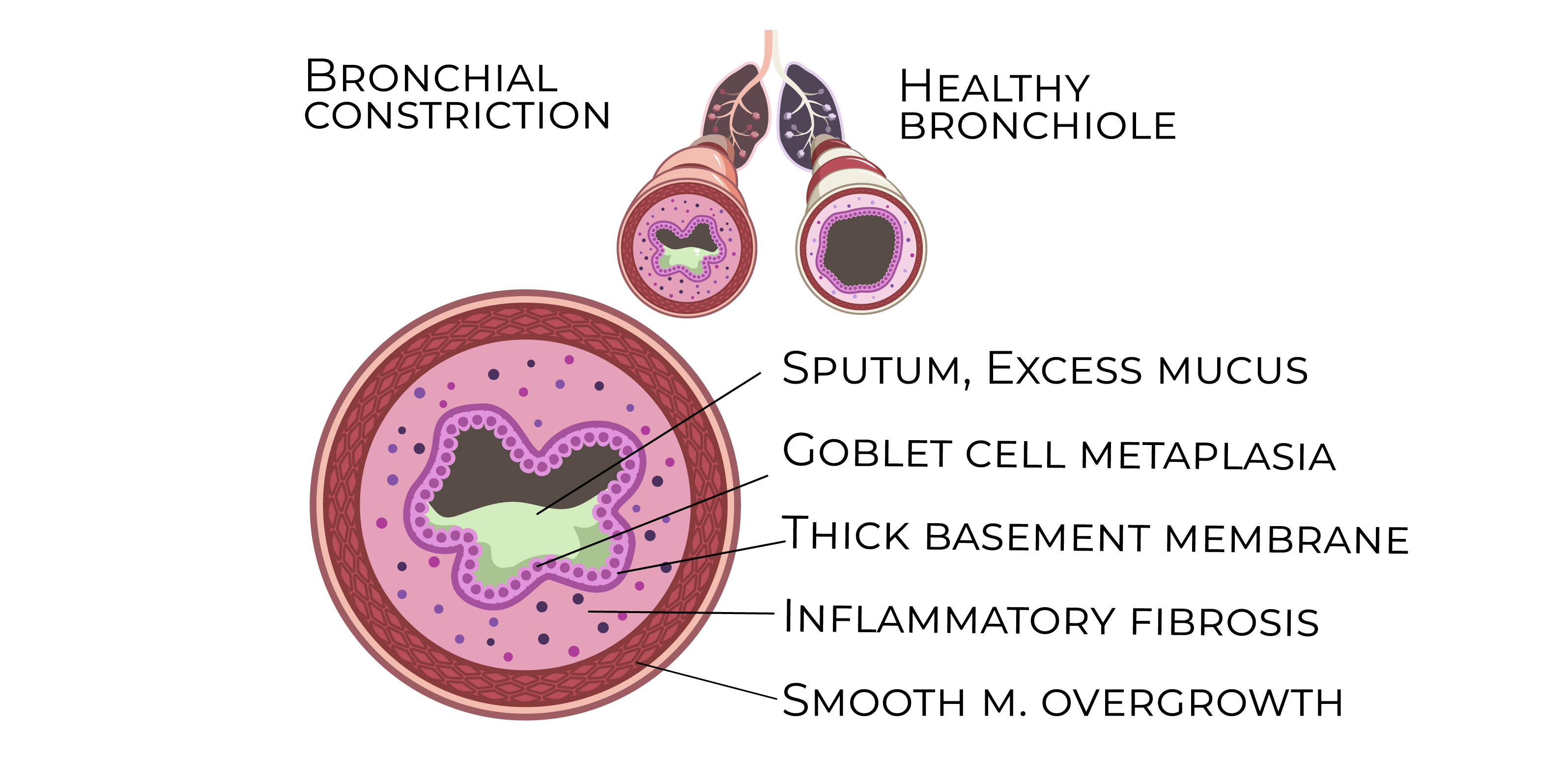
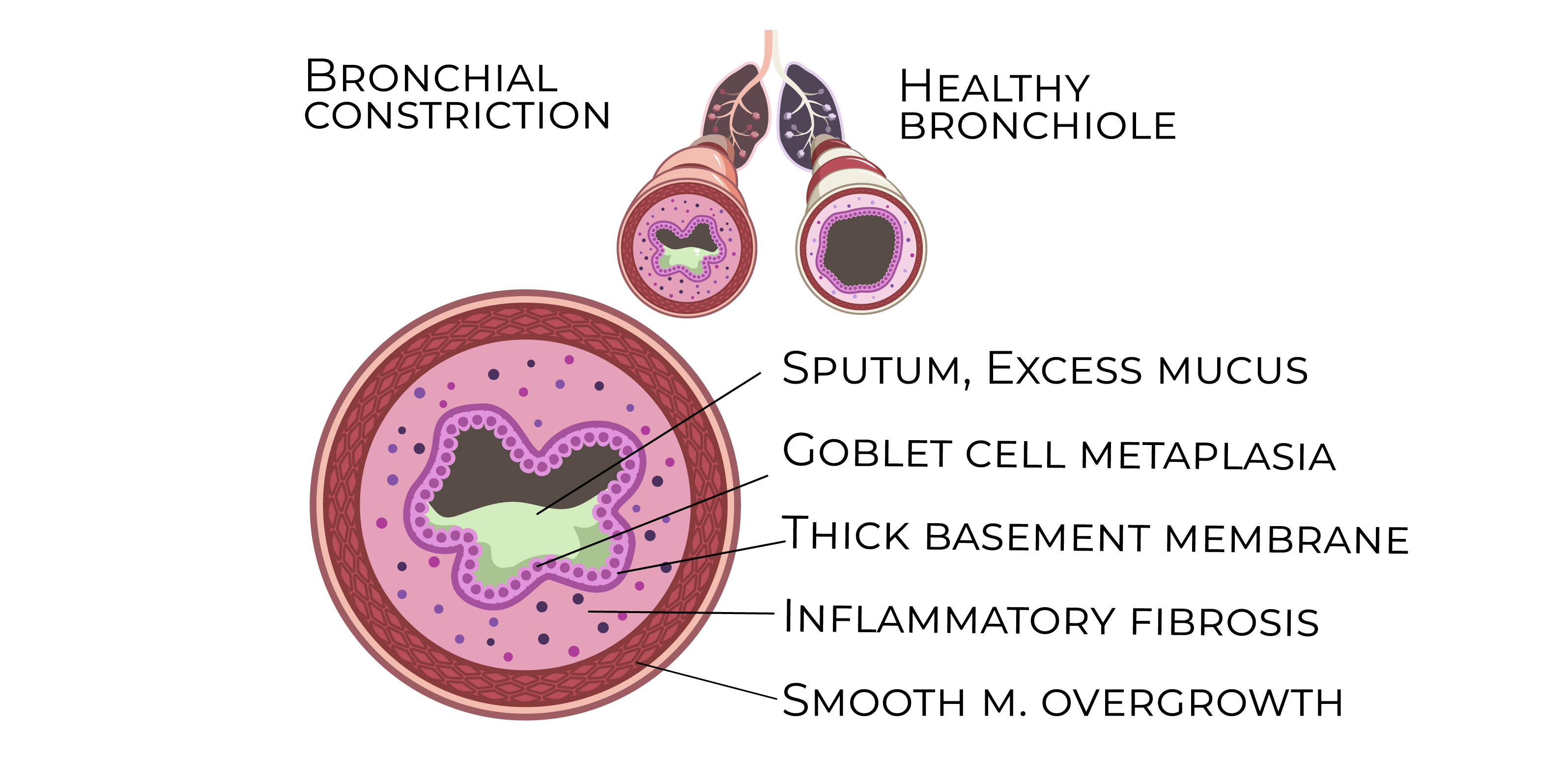
- Airway Remodeling:
- Recurrent inflammation can lead to structural changes, including thickening of the airway walls, smooth muscle hypertrophy, and subepithelial fibrosis. This can cause irreversible airway narrowing over time.
Risk Factors
- Atopy and Genetics:
- A family history of asthma, allergic rhinitis, or eczema increases the likelihood of developing asthma.
- Environmental Triggers:
- Common triggers include allergens (dust mites, pollen, animal dander), viral infections, air pollution, and tobacco smoke. Occupational exposure to chemicals and dust also plays a role.
- Exercise and Cold Air:
- Physical exertion, particularly in cold or dry conditions, can induce bronchoconstriction, known as exercise-induced asthma.
Clinical Features
- Wheezing:
- Expiratory wheezing is a classic sign of asthma, often triggered by environmental stimuli or exercise.
- Dyspnea:
- Shortness of breath, especially during physical activity or at night, is common and may fluctuate in severity.
- Cough:
- A persistent, nonproductive cough, especially nocturnal, may be the main symptom in some patients.
- Chest Tightness:
- Patients often report a feeling of tightness or pressure in the chest, which worsens during exacerbations.
Diagnosis
- Spirometry:
- The gold standard for diagnosis, demonstrating:
- Reduced FEV1 and FEV1/FVC ratio: Suggests obstructive lung disease.
- Reversibility: An increase in FEV1 by at least 12% and 200 mL after bronchodilator use confirms reversible obstruction.
- Methacholine Challenge Test:
- Used if spirometry is inconclusive. Inhalation of methacholine provokes bronchoconstriction, confirming airway hyperresponsiveness.
- Peak Expiratory Flow (PEF):
- Used to monitor asthma control and detect worsening symptoms.
Management
- Stepwise Approach:
- Intermittent Asthma (Step 1):
- Short-acting beta-agonists (SABAs) (e.g., albuterol) as needed for symptom relief.
- Mild Persistent Asthma (Step 2):
- Low-dose inhaled corticosteroids (ICS) for maintenance therapy.
- Moderate Persistent Asthma (Step 3):
- Low-dose ICS + long-acting beta-agonists (LABAs) or medium-dose ICS alone.
- Severe Persistent Asthma (Step 4 and above):
- High-dose ICS + LABA, with additional therapies like tiotropium (a long-acting muscarinic antagonist) or biologics (e.g., omalizumab for allergic asthma).
- Acute Exacerbation Management:
- SABAs: First-line treatment for quick relief during exacerbations.
- Systemic Corticosteroids: Oral or intravenous prednisone is used for moderate-to-severe exacerbations to reduce inflammation.
- Oxygen: Supplemental oxygen is administered to maintain SpO2 >90%.
Complications
- Status Asthmaticus:
- A life-threatening exacerbation unresponsive to initial treatment, requiring intensive care and possibly mechanical ventilation.
- Airway Remodeling:
- Chronic poorly controlled asthma can lead to permanent structural changes in the airways, causing fixed airflow limitation.
- Pneumothorax:
- Rare but can occur during severe exacerbations, particularly with excessive use of bronchodilators.
Key Points
- Asthma is a chronic inflammatory condition of the airways with episodic symptoms like wheezing, dyspnea, and chest tightness, often triggered by allergens, exercise, or infections.
- Diagnosis is confirmed through spirometry, demonstrating reversible airflow obstruction (FEV1/FVC improvement with bronchodilator use).
- Management follows a stepwise approach, from SABAs for intermittent asthma to ICS, LABAs, and biologics for more severe forms.
- Acute exacerbations are treated with SABAs, systemic corticosteroids, and oxygen in severe cases.
- Complications include status asthmaticus, airway remodeling, and pneumothorax, which emphasize the need for proper management and control of the disease.
