Allergy & Hypersensitivity for USMLE Step 3
Start your One-Week Free Trial
Already subscribed? Log in »
Allergy for the USMLE Step 3 Exam
Allergy Overview
- Definition:
- Allergies involve an immune overreaction to typically harmless substances (allergens) that leads to clinical symptoms, often IgE-mediated.
- Initial sensitization to an allergen triggers IgE antibody production, which binds to mast cells and basophils. Upon re-exposure, cross-linking of IgE causes degranulation and release of histamine and other mediators.
- Common Allergens:
- Environmental: Pollens, animal dander, dust mites, and molds.
- Food: Common allergens include peanuts, shellfish, tree nuts, milk, and eggs.
- Medications: Commonly antibiotics (penicillin), NSAIDs, and vaccines.
- Insect Stings: Hymenoptera (e.g., bees, wasps).
- Occupational: Latex and certain workplace chemicals.
Mechanisms of Hypersensitivity
- Type I (IgE-Mediated) Hypersensitivity:
- Mechanism: IgE antibodies generated on initial allergen exposure sensitize mast cells and basophils. Re-exposure leads to cross-linking and release of histamine, prostaglandins, and leukotrienes.
- Examples: Allergic rhinitis, asthma, anaphylaxis, and urticaria.
- Type II (Cytotoxic) Hypersensitivity:
- Mechanism: IgG or IgM antibodies bind to cell-bound antigens, leading to complement activation and cell destruction.
- Examples: Hemolytic anemia, Goodpasture syndrome.
- Type III (Immune Complex) Hypersensitivity:
- Mechanism: Antigen-antibody complexes deposit in tissues, causing inflammation via complement activation.
- Examples: Serum sickness, systemic lupus erythematosus (SLE).
- Type IV (Delayed-Type) Hypersensitivity:
- Mechanism: T-cell mediated response occurring 24-72 hours post-exposure, with cytokine release and macrophage activation.
- Examples: Contact dermatitis, tuberculosis skin test reaction.
Clinical Presentations
- Allergic Rhinitis:
- Symptoms: Sneezing, nasal congestion, itchy eyes, and rhinorrhea; seasonal or perennial.
- Diagnosis: Based on history, supported by skin or IgE testing.
- Treatment: Intranasal corticosteroids, antihistamines, and allergen avoidance.
- Asthma:
- Symptoms: Cough, wheezing, dyspnea, and chest tightness, often allergen-triggered.
- Diagnosis: Pulmonary function tests showing reversible obstruction; IgE testing may help identify triggers.
- Treatment: Inhaled corticosteroids, bronchodilators, leukotriene modifiers, and avoidance of known allergens.
- Atopic Dermatitis:
- Symptoms: Pruritic, erythematous rash on flexural surfaces.
- Diagnosis: Clinical features and consideration of allergy testing for environmental or food triggers.
- Treatment: Emollients, topical corticosteroids, and avoidance of irritants.
- Food Allergy:
- Symptoms: Urticaria, angioedema, gastrointestinal symptoms, and in severe cases, anaphylaxis.
- Diagnosis: Skin prick or serum IgE testing, with oral food challenges if necessary.
- Treatment: Avoidance of allergens and carrying an epinephrine autoinjector.
- Drug Allergy:
- Symptoms: Varies from mild rash to severe anaphylaxis.
- Diagnosis: Based on history and, for certain drugs like penicillin, skin testing.
- Treatment: Avoidance of the drug, substitution, and desensitization when necessary.
- Anaphylaxis:
- Symptoms: Rapid onset of multisystem involvement including urticaria, bronchospasm, hypotension, and shock.
- Diagnosis: Clinical, based on acute presentation following exposure.
- Treatment: Immediate intramuscular epinephrine, followed by antihistamines and corticosteroids. Patients should carry an epinephrine autoinjector.
Diagnostic Tests
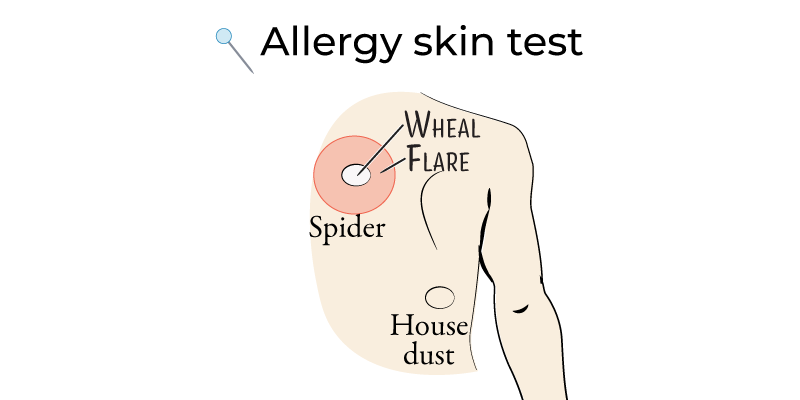
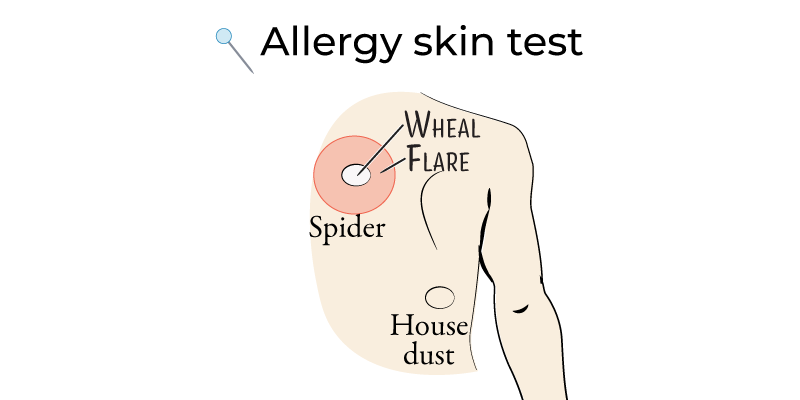
- Skin Prick Testing:
- Procedure: Small allergen amounts introduced into the skin; a positive response is a wheal-and-flare reaction.
- Indications: Allergic rhinitis, asthma, and food allergies.
- Serum IgE Testing:
- Procedure: Measures allergen-specific IgE antibodies in the blood.
- Indications: Useful in patients who cannot undergo skin testing.
- Oral Food Challenge:
- Procedure: Gradual exposure to the suspect allergen under medical supervision, especially when other tests are inconclusive.
Treatment Overview
- Avoidance: First-line management, particularly for food and environmental allergens.
- Pharmacologic Therapy:
- Antihistamines: Effective for allergic rhinitis and urticaria.
- Corticosteroids: Intranasal for rhinitis, inhaled for asthma, topical for dermatitis.
- Bronchodilators: Short-acting beta agonists for acute asthma symptoms.
- Immunotherapy:
- Subcutaneous and Sublingual Immunotherapy: Indicated for allergic rhinitis and asthma, promoting tolerance to specific allergens.
Key Points
- Allergies are often IgE-mediated hypersensitivity reactions that can range from mild (e.g., rhinitis) to severe (e.g., anaphylaxis).
- Common allergens include environmental triggers, foods, medications, and insect stings.
- Diagnosis relies on history, physical examination, and confirmatory testing (e.g., skin prick, serum IgE).
- Management includes allergen avoidance, pharmacologic therapy (antihistamines, corticosteroids), and immunotherapy.
- Anaphylaxis requires prompt epinephrine administration; patients at risk should carry an epinephrine autoinjector.
