USMLE/COMLEX 3 - Supraventricular & Ventricular Arrhythmias
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 3 & COMLEX-USA Level 3 from the Supraventricular & Ventricular Arrhythmias tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
 Below is information not explicitly contained within the tutorial but important for USMLE Step 3.
Below is information not explicitly contained within the tutorial but important for USMLE Step 3.
- --
VITAL FOR USMLE/COMLEX 3
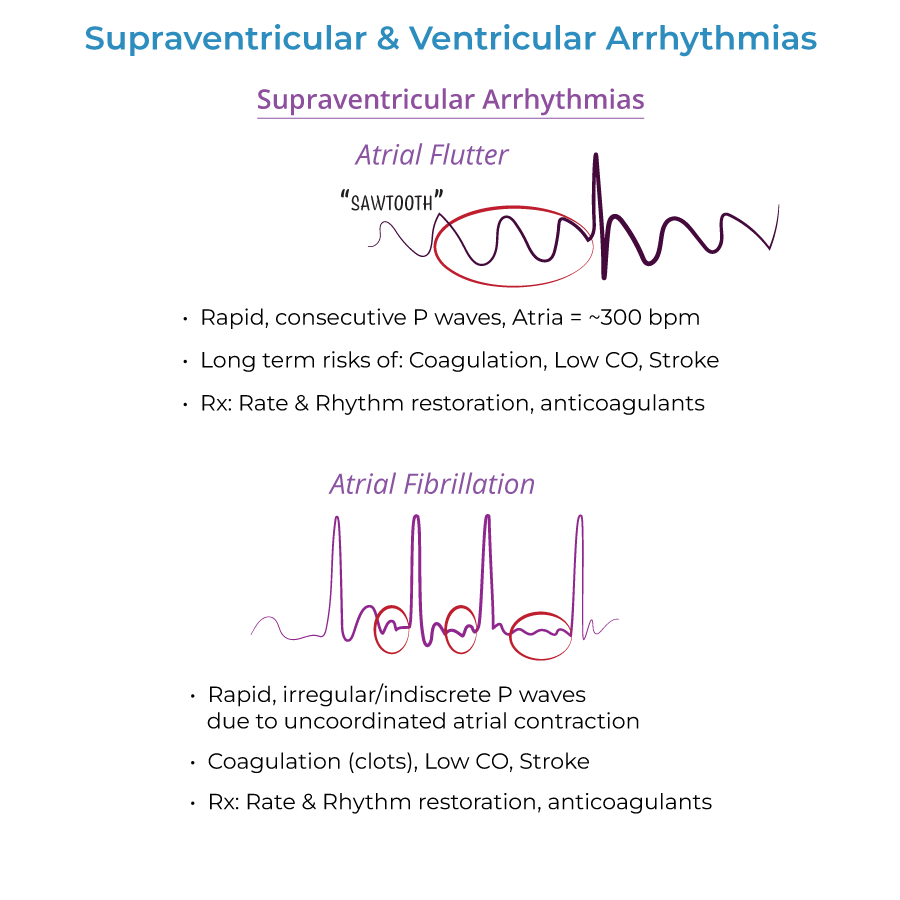
Atrial Arrhythmias Management
1. Atrial flutter treatment approach: Rate control with drugs: beta-blockers, calcium channel blockers (verapamil, diltiazem). Rhythm control with cardioversion, drugs (antiarrhythmics), possibly ablation. Anticoagulants (warfarin) are used to prevent thromboembolism.
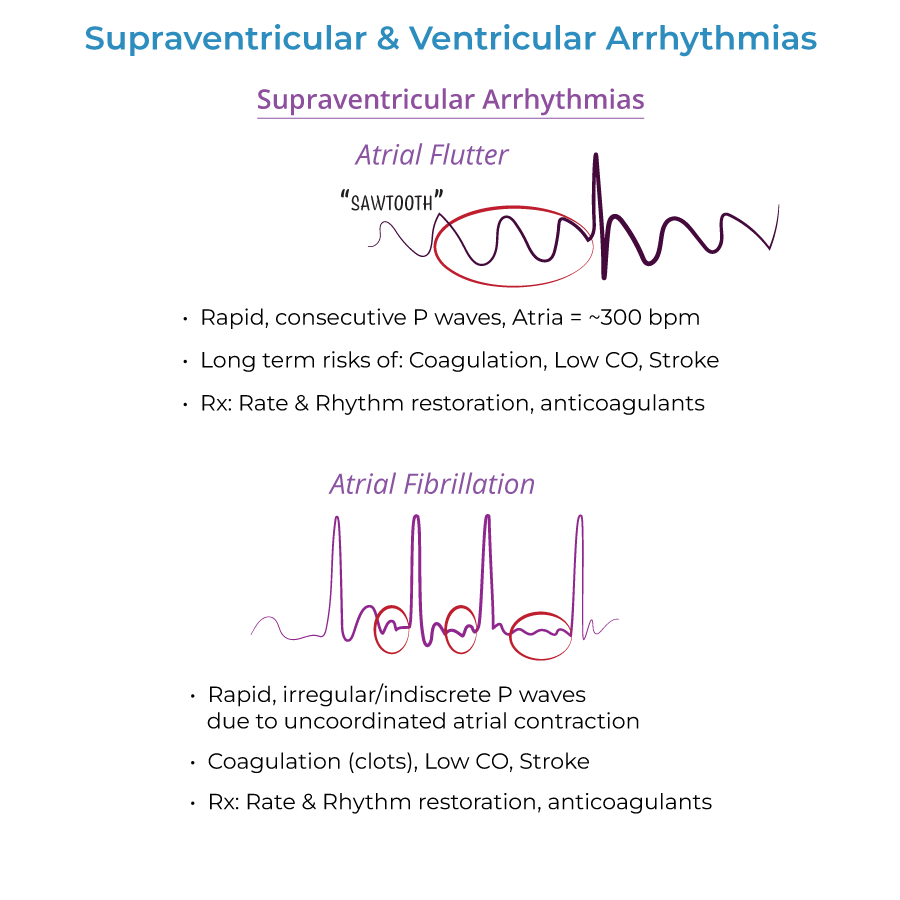
2. Atrial fibrillation management strategy: Rate control with beta blockers and nondihydropyridine calcium channel blockers. Anticoagulation before cardioversion therapy to prevent thromboembolism.
3. AV node blocker contraindication: Rule out Wolff-Parkinson-White Syndrome with accessory pathway; look for wide QRS. AV node blockers possible but beware Wolff-Parkinson-White Syndrome.
Ventricular Arrhythmias Management
1. Ventricular tachycardia therapy: Cardioversion, antiarrhythmic drugs, defibrillator implant.
2. Torsades de Pointes treatment: Magnesium.
3. Ventricular fibrillation emergency response: CPR & Defibrillation.
Critical Management Considerations
1. WPW treatment approach: Direct-current cardioversion therapy is preferred; long term treatment may require catheter ablation. Beware digoxin/nondihydropyridine calcium channel blockers to WPW patients, as they may trigger ventricular fibrillation (fatal).
2. Long QT management awareness: Prone to torsades de pointes, which can cause syncope, ventricular fibrillation, and sudden death.
3. Cardiac arrest management: Both asystole and pulseless electrical activity can lead to cardiac arrest.
- --
HIGH YIELD
Clinical Presentations
1. Atrial flutter symptoms: May be none. Or, may cause palpitations, and reduced CO, difficulty breathing, weakness, chest discomfort, syncope.
2. Atrial fibrillation presentation: May be asymptomatic. Or, may experience lack of energy, fast, irregular pulse, difficulty breathing, palpitations, chest discomfort, dizziness.
3. Ventricular tachycardia symptoms: May be asymptomatic if duration is short (aka, paroxysmal) or rate is not excessive; If sustained, palpitations, difficulty breathing, chest pain, dizziness, fainting, death.
4. Torsades de Pointes symptoms: Recurrent palpitations, dizziness, fainting, difficulty breathing.
Diagnostic Considerations
1. Atrial fibrillation workup: Echocardiography to check for structural defects, thyroid function tests.
2. WPW diagnostic findings: Short PR interval and positive delta wave at beginning of broad QRS complex; delta wave reflects early depolarization.
3. ECG in Torsades: Rapid, irregular QRS complexes "spiral" around baseline, as ventricular rate varies from cycle to cycle.
4. Pulseless electrical activity: Cardiac electrical activity is present, but no pulse is present due to inactivity of cardiac muscle.
Medication Considerations
1. Risk of specific medications: Medications that can trigger arrhythmias include antiarrhythmics, tricyclic antidepressants, anti-histamines when taken with erythromycin.
2. WPW medication caution: Beware digoxin/nondihydropyridine calcium channel blockers to WPW patients, as they may trigger ventricular fibrillation (fatal).
3. Long QT medication risks: Antihistamines, decongestants, diuretics, antiarrhythmic drugs, antidepressants can cause or worsen long QT.
4. Electrolyte considerations: Hypocalcemia, hypokalemia can trigger Torsades de Pointes.
Clinical Complications
1. Atrial flutter complications: When coupled with other cardiac complications, can lead to stroke, makes heart work more difficult, ventricular weakening, and coagulation is more likely. Patients may have periods of atrial fibrillation.
2. Atrial fibrillation complications: Stroke, systemic emboli.
3. Ventricular tachycardia complications: Can lead to heart failure, unconsciousness, sudden death by cardiac arrest.
4. Long QT complications: Prone to torsades de pointes, which can cause syncope, ventricular fibrillation, and sudden death.
- --
Beyond the Tutorial
Advanced Management Considerations
1. Rate vs rhythm control trials: Evidence base for choosing between rate and rhythm control strategies in atrial fibrillation.
2. Novel oral anticoagulants: Role of DOACs vs warfarin for stroke prevention in atrial fibrillation.
3. Catheter ablation evidence: Success rates and patient selection for ablation of various arrhythmias.
4. ICD therapy trials: Primary and secondary prevention indications based on clinical trial evidence.
Special Populations Management
1. Geriatric considerations: Adjustments to therapy due to comorbidities, polypharmacy, and fall risk.
2. Heart failure with arrhythmias: Specific management considerations when arrhythmias occur in the setting of heart failure.
3. Post-MI arrhythmias: Approach to various arrhythmias following myocardial infarction.
4. Perioperative management: Approach to patients with arrhythmias or devices undergoing surgery.
Quality Metrics and Systems-Based Practice
1. Anticoagulation quality metrics: Meeting standards for appropriate anticoagulation in atrial fibrillation.
2. Sudden cardiac death prevention: Community-based AED programs and education.
3. Remote monitoring: Implementation and interpretation of data from implantable cardiac devices.
4. Transition of care: Managing patients with arrhythmias across inpatient and outpatient settings.
Cost-Effectiveness Considerations
1. Medication selection: Cost-effectiveness of various antiarrhythmic and anticoagulant strategies.
2. Device therapy: Appropriate use criteria for expensive device therapies.
3. Ablation vs medical therapy: Long-term cost comparisons for various arrhythmia management strategies.
4. Screening programs: Evidence for cost-effectiveness of screening for specific arrhythmias or conditions.
