USMLE/COMLEX 3 - Myocardial Infarctions
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 3 & COMLEX-USA Level 3 from the Myocardial Infarctions: Diagnosis & Treatment tutorial, focusing on advanced clinical management, complex decision-making, and systems-based practice concepts that are essential for these exams. See the tutorial notes for further details and relevant links.
 Below is information not explicitly contained within the tutorial but important for USMLE Step 3 & COMLEX Level 3.
Below is information not explicitly contained within the tutorial but important for USMLE Step 3 & COMLEX Level 3.
- --
VITAL FOR USMLE/COMLEX 3
Epidemiology & Risk Factors
1. Geographic distributions: Declining in high-income countries but rising in middle- and low-income countries.
2. Demographic patterns: Incidence after age 35, from highest to lowest: Black males > Black females > White males > White females.
3. Gender differences: MI occurs approximately 10 years earlier in men than women.
4. Mortality patterns: Higher mortality rates in women than their male peers, especially for young and/or minority women.
5. Modifiable risk factors: Dyslipidemia, diabetes mellitus, hypertension, smoking (including e-cigarettes), obesity, psychosocial stress, alcohol consumption, poor diet.
Diagnostic Decision-Making
1. Definition: Myocardial infarction is defined as myocardial injury with ischemia.
2. ECG interpretation: Should be administered as soon as possible when MI is suspected, and re-administered frequently to observe the evolution of the infarction.
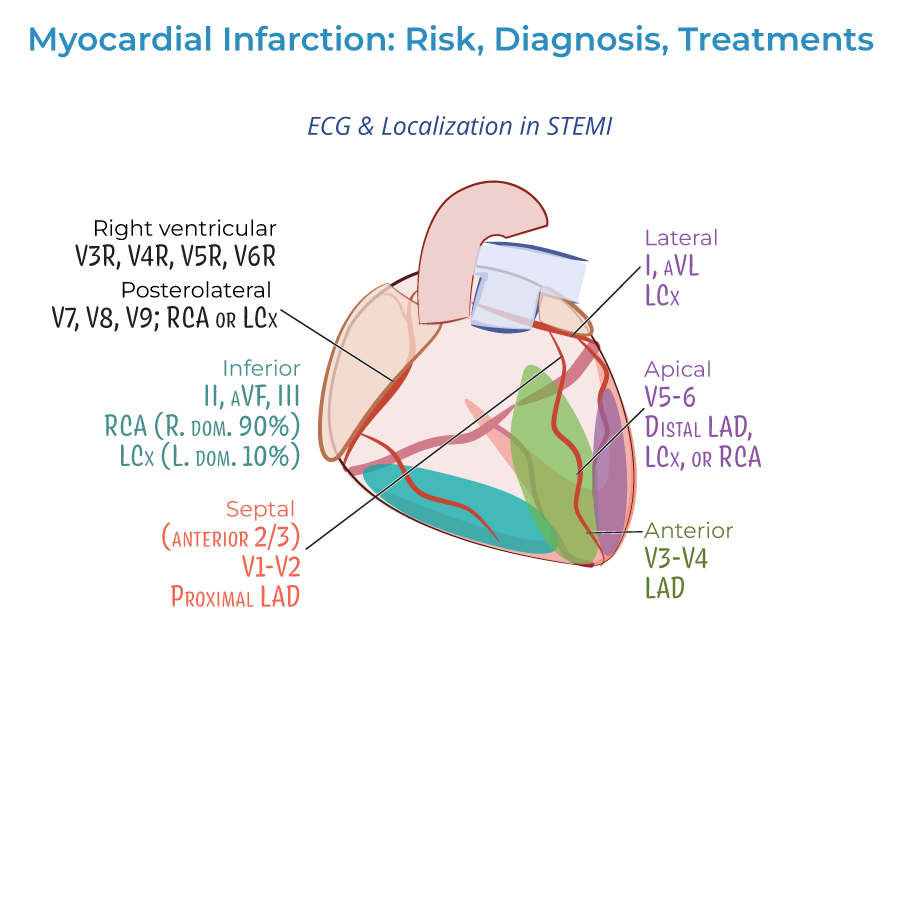
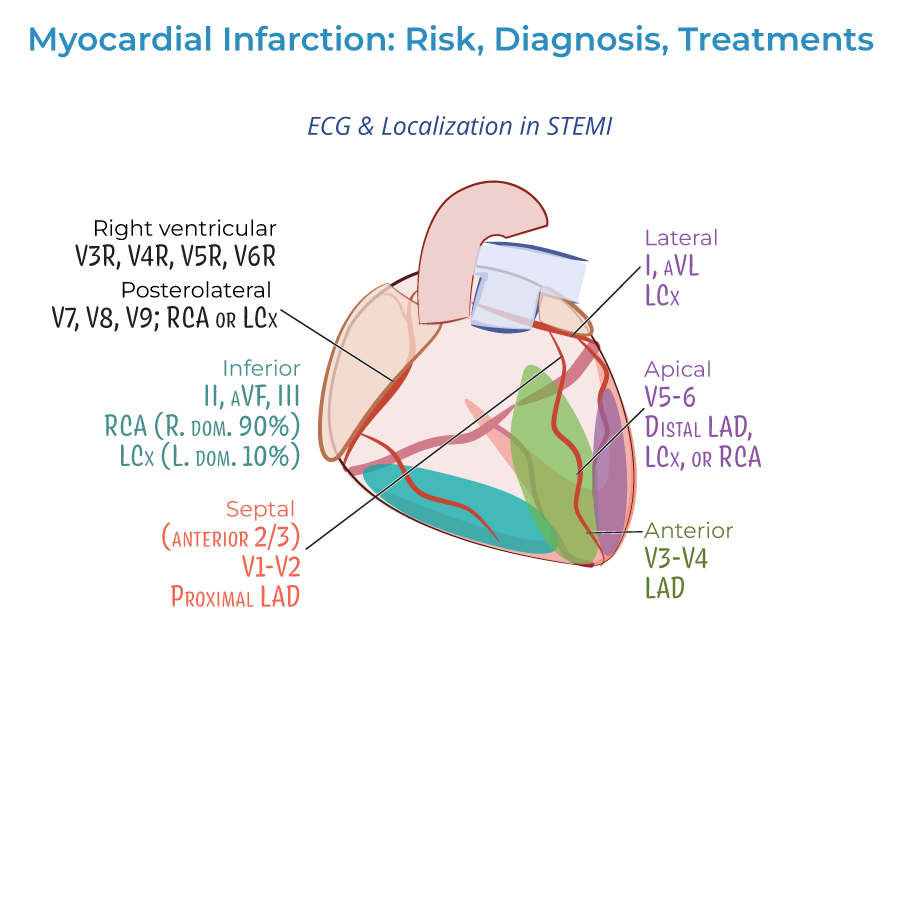
3. ECG localization: Identifying specific territories based on lead changes:
- Lateral infarction: Leads I and aVL; often left circumflex artery
- Apical infarctions: Leads V5 and V6; often left circumflex or right coronary arteries
- Anterior infarctions: Leads V3 and V4; left anterior descending artery
- Anterior septal infarctions: Leads V1 and V2; proximal left anterior descending artery
- Inferior infarctions: Leads II, aVF, and III; right coronary artery or left circumflex artery
- Right ventricular infarctions: Requires leads V3R-V6R
- Posterolateral infarctions: Requires leads V7-V9; right coronary or left circumflex artery
Treatment Decision Algorithms
1. Pre-hospital considerations: Early administration of oxygen (when saturation <90%), aspirin, and nitrates.
2. Reperfusion strategy selection: Based on severity of infarction:
- STEMI: Emergency PCI preferred; if unavailable, fibrinolytic drugs ASAP
- NSTEMI: Timing based on risk stratification (immediate for unstable patients, delayed for stable patients)
- Antiplatelets: Aspirin, clopidogrel, or other P2Y12 inhibitors
- Anticoagulation: Unfractionated or low molecular weight heparin
- Anti-ischemic: Beta-blockers or calcium-channel blockers
- Plaque stabilization: Statins, ACE-inhibitors
Recognition of Complications
1. Prodromal symptoms: May occur days, weeks, or months before the actual MI.
2. Silent MI: Recognition that some patients may have no noticeable symptoms.
3. Gastrointestinal manifestations: Nausea, vomiting, and indigestion may mask cardiac symptoms.
4. Psychogenic symptoms: Anxiety or sense of impending doom may be harbingers of MI.
5. Evolution of infarction: Understanding the dynamic nature of ECG changes over time.
- --
HIGH YIELD
Clinical Presentation Patterns
1. Chest pain variations: Dull, sharp, squeezing, pressure, or simply described as discomfort.
2. Radiation patterns: Pain may radiate to arms, neck, jaw, or back.
3. Non-pain symptoms: Extreme fatigue, exhaustion, sleep disturbances (particularly during prodromal period).
4. Neurological symptoms: Headaches, dizziness, lightheadedness common.
5. Respiratory symptoms: Shortness of breath (dyspnea) may be a prominent feature.
ECG Interpretation Pearls
1. Q-wave significance: May indicate size/location of current MI or evidence of prior MI.
2. ST-segment evaluation: Distinguishing between STEMI and NSTEMI guides treatment strategy.
3. Serial ECG importance: Re-administration to observe evolution of infarction patterns.
4. Lead selection: Standard 12-lead plus additional leads (V3R-V6R, V7-V9) when suspecting specific infarct locations.
5. Reciprocal changes: Understanding the significance of ST depression in reciprocal leads.
Biomarker Analysis
1. Troponin kinetics: Understanding the rise and fall pattern within 24 hours of MI.
2. CK-MB patterns: Complementary to troponin for timing and extent assessment.
3. Distinguishing features: Using biomarkers to differentiate between NSTEMI and unstable angina.
4. Timing considerations: Optimal sampling intervals for diagnosis and monitoring.
5. Interpretation in special populations: Renal dysfunction, elderly, or post-procedure elevation.
Reperfusion Decision-Making
1. Timing imperatives: Treatment should begin as soon as possible to reduce myocardial necrosis.
2. PCI considerations: Emergency PCI typically recommended for STEMI patients.
3. Fibrinolytic selection: When immediate PCI not available, administration timing is critical.
4. Revascularization indications: Unstable/complicated NSTEMI often requires immediate intervention.
5. Risk-benefit assessment: Understanding when conservative management may be appropriate.
Demographic Considerations
1. Gender differences: Women have higher mortality and often present atypically.
2. Racial/ethnic variations: Significant differences in MI incidence across populations.
3. Age-related considerations: Earlier occurrence in men vs. women by approximately 10 years.
4. Health literacy impact: Many patients, especially women, are unaware of risk factors and symptoms.
5. Socioeconomic factors: Impact on prevention, recognition, and treatment access.
- --
Beyond the Tutorial
Advanced Management Considerations
1. MINOCA (MI with Non-Obstructive Coronary Arteries): Diagnostic approach and management differences.
2. Type 2 MI: Supply-demand mismatch management distinct from Type 1 atherothrombotic MI.
3. Mechanical complications: Early recognition and management of papillary muscle rupture, ventricular septal rupture, and free wall rupture.
4. Cardiogenic shock algorithms: Mechanical support device selection and timing.
5. Post-MI arrhythmia management: Risk stratification for sudden cardiac death, antiarrhythmic selection.
Systems-Based Practice Concepts
1. STEMI systems of care: Regional networks, transfer protocols, door-to-balloon time optimization.
2. Quality metrics: Monitoring and improving key performance indicators in MI management.
3. Transitions of care: Post-discharge planning, medication reconciliation, cardiac rehabilitation referral.
4. Healthcare disparities: Recognition and addressing inequities in MI care and outcomes.
5. Resource utilization: Appropriate use of diagnostic testing and interventions in different clinical scenarios.
Advanced Pharmacotherapeutic Considerations
1. Antithrombotic therapy personalization: Risk-benefit assessment for duration and intensity.
2. Bleeding risk management: Strategies for patients on dual or triple antithrombotic therapy.
3. Medication adherence optimization: Strategies to improve long-term compliance with secondary prevention.
4. Polypharmacy management: Addressing drug interactions and side effects in complex post-MI regimens.
5. Novel therapeutic approaches: Emerging evidence for anti-inflammatory and metabolic interventions.
Long-Term Management Strategies
1. Secondary prevention optimization: Risk factor modification, guideline-directed medical therapy.
2. Functional capacity assessment: Return to work evaluation, exercise prescriptions.
3. Psychosocial aspects: Depression screening and management, social support assessment.
4. Recurrent event prevention: Intensified therapy for very high-risk patients.
5. Heart failure development: Early recognition and intervention for post-MI ventricular dysfunction.
