USMLE/COMLEX 3 - Myocardial Infarction Symptoms, Diagnosis, & Treatments
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 3 & COMLEX-USA Level 3 from the Myocardial Infarctions: Diagnosis & Treatment tutorial, focusing on advanced clinical management, complex decision-making, and systems-based practice concepts that are essential for these exams. See the tutorial notes for further details and relevant links.
 Below is information not explicitly contained within the tutorial but important for USMLE Step 3 & COMLEX Level 3.
Below is information not explicitly contained within the tutorial but important for USMLE Step 3 & COMLEX Level 3.
- --
VITAL FOR USMLE/COMLEX 3
Epidemiology & Healthcare Disparities
1. Geographic variations: Incidence of myocardial infarctions is declining in high-income countries but rising in middle- and low-income countries.
2. Demographic patterns: Within the United States, MI incidence after age 35, from highest to lowest: Black males > Black females > White males > White females.
3. Gender disparities: First MI occurs approximately 10 years earlier in men than women, possibly related to risk factors such as smoking and hyperlipidemia.
4. Mortality disparities: Despite overall declining rates, mortality remains higher in women than male peers, especially for young and/or minority women.
5. Health literacy gap: Many patients, especially women, are unaware of risk factors and symptoms—a significant obstacle to prevention and treatment of myocardial infarction.
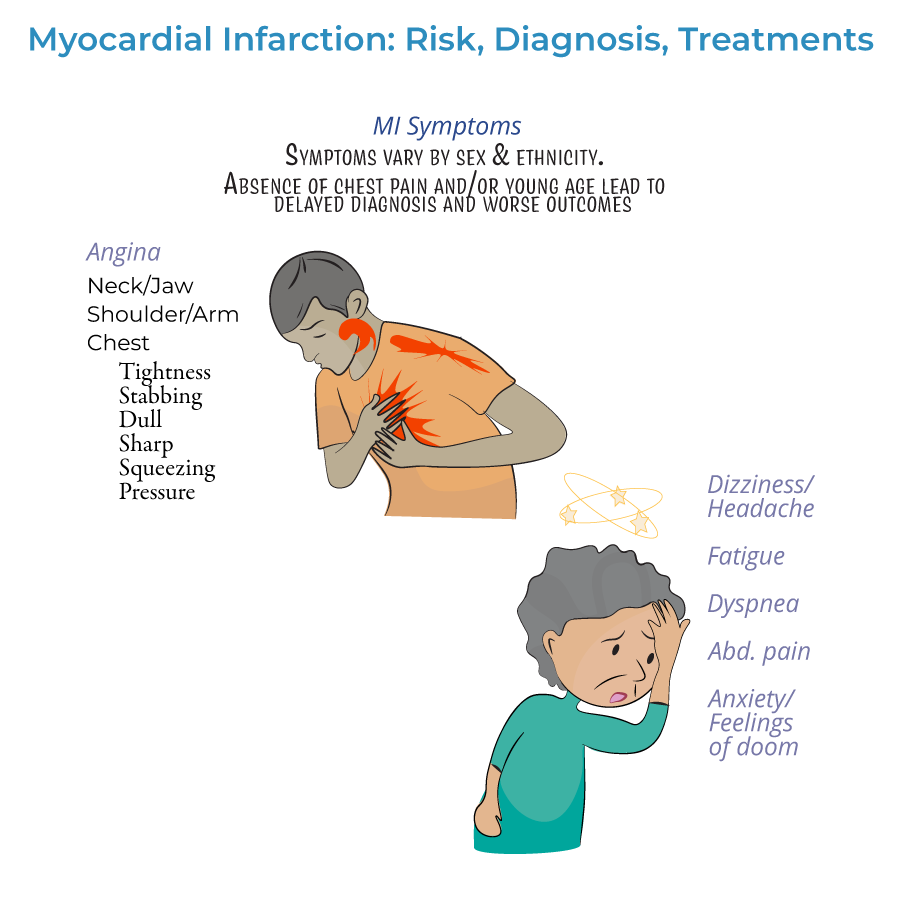
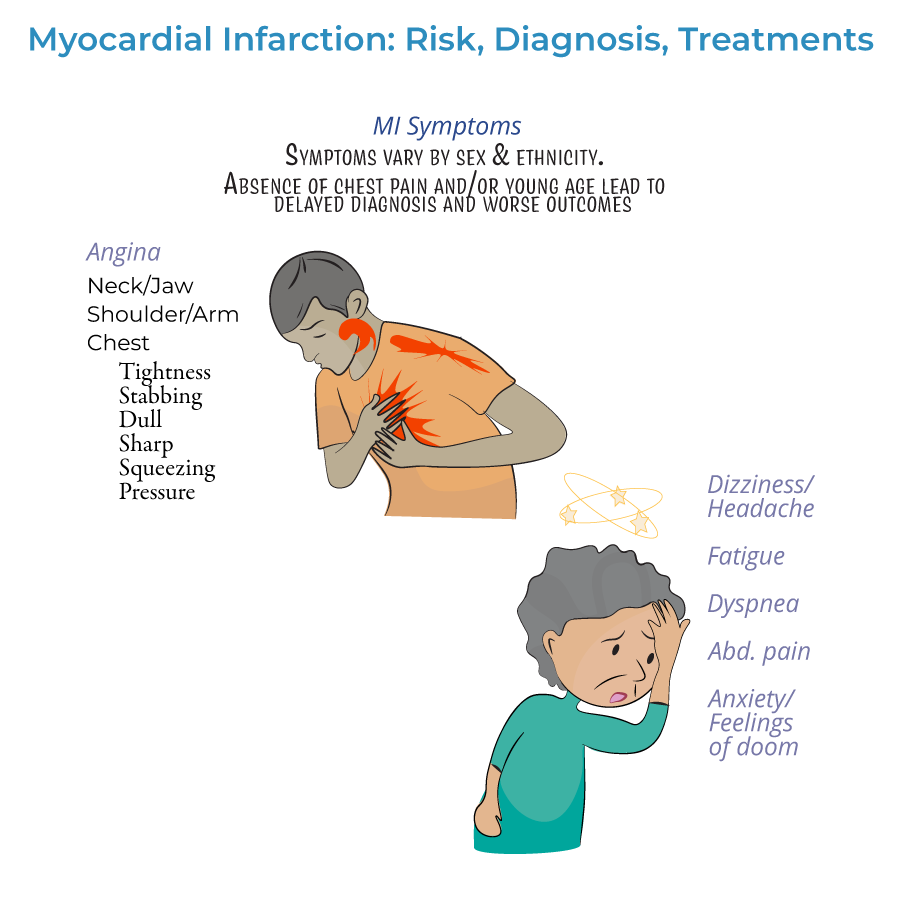
Clinical Recognition & Diagnostic Decision-Making
1. Syndrome definition: Myocardial infarction is defined as myocardial injury with ischemia.
2. Presentation patterns:
- Prodromal symptoms: Days, weeks, or months prior to the acute event
- Acute symptoms: Experienced at the time of the event
- Silent MI: No noticeable symptoms
Advanced ECG Interpretation
1. Timing importance: ECG should be administered as soon as possible when MI is suspected, and re-administered frequently to observe the evolution of the infarction.
2. STEMI vs. NSTEMI classification: Critical for determining reperfusion strategy and urgency.
3. Q-wave significance: May indicate size/location of current MI or evidence of prior MI.
4. Comprehensive localization:
- Lateral infarction: Leads I and aVL; left circumflex artery
- Apical infarction: Leads V5 and V6; left circumflex or right coronary arteries
- Anterior infarction: Leads V3 and V4; left anterior descending artery
- Anteroseptal infarction: Leads V1 and V2; proximal left anterior descending artery
- Inferior infarction: Leads II, aVF, and III; right coronary artery or left circumflex artery (in ~10% with left dominance)
- Right ventricular infarction: Requires additional leads V3R through V6R
- Posterolateral infarction: Requires additional leads V7-V9; right coronary or left circumflex artery
Biomarker Assessment
1. Diagnostic hierarchy: Cardiac troponin is the preferred biomarker for MI diagnosis.
2. Differential utility: Biomarker values help distinguish between NSTEMI and unstable angina—only NSTEMI is associated with rising/falling troponin levels.
3. Temporal patterns: Both cardiac troponin I and CK-MB peak within 24 hours of MI and gradually return to normal.
4. Serial measurements: More valuable than single determinations for diagnosis, estimating infarct size, and detecting reinfarction.
5. Integration with clinical context: Biomarkers must be interpreted within the overall clinical picture, including ECG changes and symptoms.
Advanced Treatment Decision Algorithms
1. Time-critical approach: Treatment should begin as soon as possible, ideally before hospital arrival, to reduce myocardial necrosis.
2. Pre-hospital protocols:
- Oxygen administration when oxygen saturation is less than 90%
- Aspirin for antiplatelet effects
- Nitrates for chest pain (morphine if nitrates ineffective)
- STEMI: Emergency PCI recommended; if unavailable, immediate fibrinolytic therapy
- NSTEMI: Risk stratification guides intervention timing—unstable/complicated cases require immediate PCI/CABG; uncomplicated cases may wait longer
- Fibrinolytics: Generally not recommended for NSTEMI due to unfavorable risk/benefit ratio
- Antiplatelets: Aspirin, clopidogrel, or others
- Anticoagulation: Unfractionated or low molecular weight heparin
- Anti-ischemic: Beta-blockers or calcium-channel blockers
- Plaque stabilization: Statins, ACE-inhibitors
- --
HIGH YIELD
Complex Clinical Scenario Management
1. Atypical presentation recognition: Absence of chest pain, especially in women, elderly, and diabetics, requires high clinical suspicion.
2. Multisystem symptom integration: Gastrointestinal symptoms, fatigue, dyspnea, or anxiety may be predominant presentations.
3. Prodromal symptom recognition: Extreme fatigue, sleep disturbances, and vague discomfort days to months before acute event may provide early intervention opportunity.
4. Silent MI detection: Incidental findings of MI on ECG or imaging require appropriate secondary prevention strategies.
5. Psychogenic symptom evaluation: Anxiety or sense of impending doom may be harbingers of MI rather than primary psychiatric symptoms.
Advanced ECG Interpretation Pearls
1. Evolution monitoring: Serial ECGs to track development and resolution of ischemic changes.
2. Localization accuracy: Different lead abnormalities correspond to specific coronary territories:
- Anterior/septal (V1-V4): Left anterior descending artery
- Lateral (I, aVL, V5-V6): Left circumflex artery
- Inferior (II, III, aVF): Right coronary artery (or left circumflex in left dominant patients)
Comprehensive Biomarker Approach
1. Troponin primacy: Cardiac troponin is key to diagnosis of myocardial infarction.
2. Temporal utilization: Both cardiac troponin I and CK-MB peak within 24 hours of MI.
3. NSTEMI vs. unstable angina differentiation: Only NSTEMI shows troponin elevation; critical for treatment pathway decisions.
4. Reinfarction detection: Serial measurements can identify new events after initial MI.
5. Integration with ECG findings: Combining biomarker trends with ECG evolution provides more complete assessment.
Treatment Strategy Optimization
1. Reperfusion timing: "Time is myocardium"—treatment should begin as soon as possible to minimize necrosis.
2. Therapeutic selection algorithm:
- STEMI: Emergency PCI preferred; fibrinolytics if PCI unavailable
- NSTEMI: Risk-based approach to intervention timing and modality
Special Population Management
1. Women: Higher mortality rates, more atypical presentations, first MI approximately 10 years later than men.
2. Young patients: Often experience missed/delayed diagnosis due to low clinical suspicion despite presentation.
3. Racial/ethnic disparities: Black males and females have higher incidence than white counterparts; minority women have particularly high mortality.
4. Patient education imperatives: Awareness of risk factors and symptoms significantly impacts outcomes; education initiatives should target high-risk populations.
5. Geographic considerations: Rising incidence in middle- and low-income countries requires tailored prevention and treatment strategies.
- --
Beyond the Tutorial
Advanced Management Considerations
1. MINOCA (MI with Non-Obstructive Coronary Arteries): Diagnostic approach and management differences.
2. Type 2 MI: Supply-demand mismatch management distinct from Type 1 atherothrombotic MI.
3. Cardiogenic shock management: Mechanical support devices, vasopressors, and timing of revascularization.
4. Post-MI arrhythmia management: Acute vs. chronic approaches, device therapy indications.
5. Mechanical complications: Early recognition and management of papillary muscle rupture, ventricular septal rupture, and free wall rupture.
Systems-Based Practice
1. STEMI systems of care: Regional networks, transfer protocols, door-to-balloon time optimization.
2. Quality metrics: Core measures for AMI care, public reporting implications.
3. Transitions of care: Post-discharge planning, medication reconciliation, follow-up arrangements.
4. Healthcare disparities: Addressing inequities in MI prevention, recognition, and treatment.
5. Resource utilization: Appropriate use of diagnostic testing and interventions in various clinical contexts.
Complex Pharmacotherapeutic Decisions
1. P2Y12 inhibitor selection: Individualized approach based on patient factors and comorbidities.
2. Anticoagulation strategy: Agent selection and duration based on clinical scenario and comorbidities.
3. Beta-blocker optimization: Timing, dosing, and contraindications in various clinical scenarios.
4. Statin intensity decisions: Risk-based approach to lipid management after MI.
5. Antithrombotic combinations: Managing patients with indications for both DAPT and anticoagulation.
Advanced Imaging and Diagnostic Modalities
1. Cardiac MRI: Role in diagnosis of borderline cases and assessment of complications.
2. Coronary CT angiography: Utility in selected patients with intermediate pre-test probability.
3. Echocardiography: Timing, mode, and interpretation for post-MI assessment.
4. Nuclear imaging: Role in viability assessment and risk stratification.
5. Invasive assessment: FFR, iFR, and IVUS applications in complex coronary disease.
Long-Term Management Strategies
1. Cardiac rehabilitation: Components, benefits, and implementation strategies.
2. Secondary prevention optimization: Evidence-based targets for risk factor control.
3. Psychosocial assessment: Depression screening and management after MI.
4. Return to activities guidance: Evidence-based recommendations for driving, work, exercise, and sexual activity.
5. Recurrent event prevention: Intensified therapy for very high-risk patients.
