USMLE/COMLEX 3 - Liver Disease Overview
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 3 & COMLEX-USA Level 3 from the Liver Pathophysiology Overview tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
 Below is information not explicitly contained within the tutorial but important for USMLE & COMLEX 3.
Below is information not explicitly contained within the tutorial but important for USMLE & COMLEX 3.
- --
VITAL FOR USMLE/COMLEX 3
Clinical Diagnosis and Management
1. Disease Recognition: Early diagnosis is key for proper treatment, and even reversal, of damage.
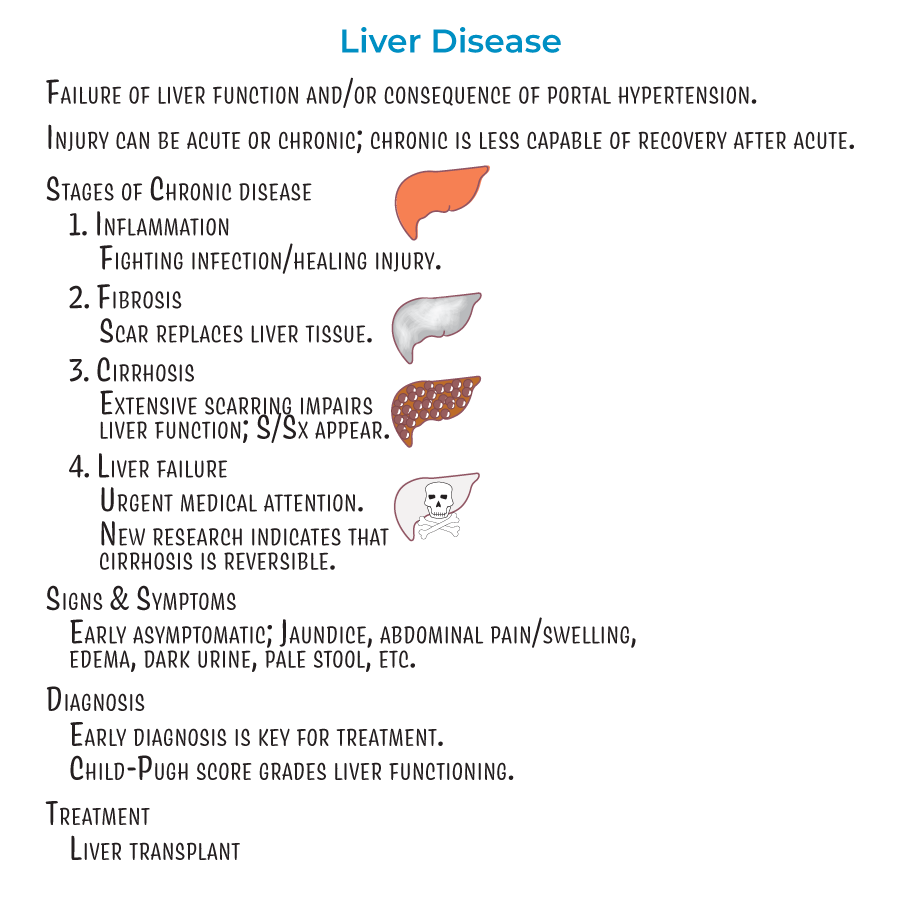
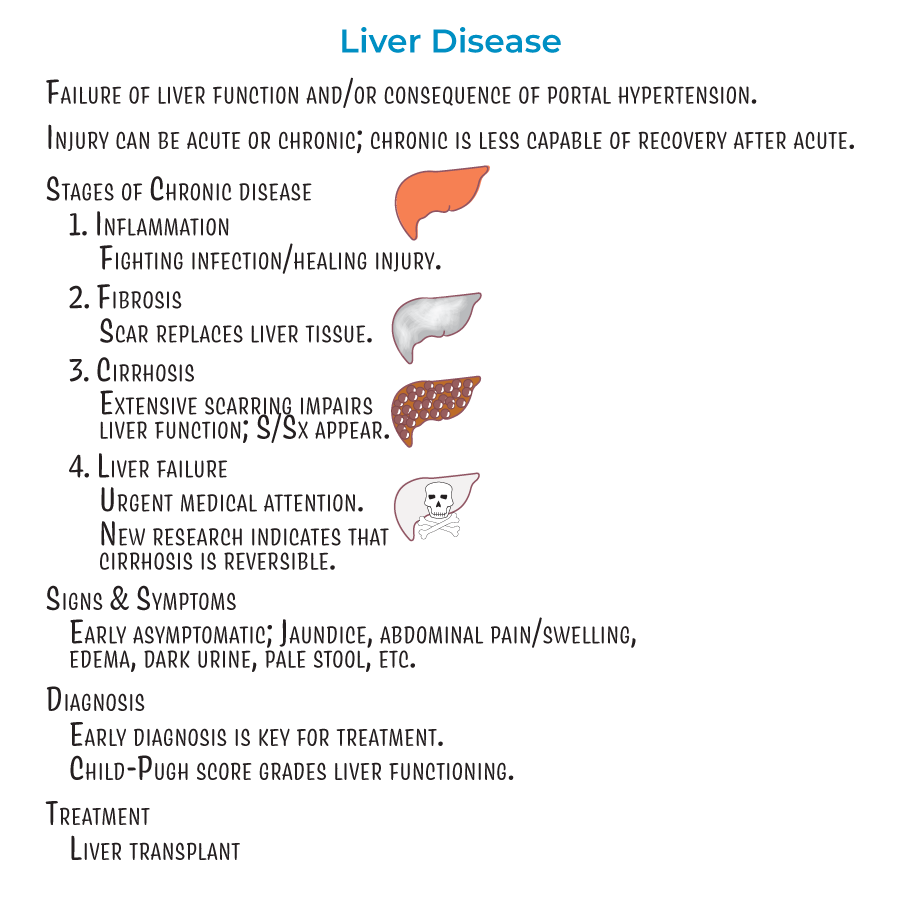
2. Staging Awareness: Liver disease progresses through inflammation, fibrosis, cirrhosis, and liver failure stages.
3. Reversibility Potential: Newer research indicates that cirrhosis (stage 3) is also reversible, not just stages 1 and 2.
4. Prognostic Assessment: The Child-Pugh score is used to grade liver functioning.
5. Definitive Treatment: In cases of cirrhosis or failure, transplants may be the best option.
Portal Hypertension Management
1. Variceal Bleeding Risk: Varices are collateral blood vessels that form to provide alternative blood flow routes; these pose a significant risk for hemorrhage, and are an important cause of GI bleeding.
2. Ascites Management: Ascites refers to the accumulation of fluid in the peritoneum caused by systemic dilation that allows fluid leakage. Ascites is a main complication of cirrhosis, and can lead to peritonitis.
3. Infection Prevention: Spontaneous Bacterial Peritonitis (SBP) is an acute infection resulting from bacteria and endotoxins leaking from the GI tract, and can lead to septic shock if not treated promptly.
Hepatic Encephalopathy Assessment
1. Pathophysiology Understanding: Hepatic encephalopathy is the result of toxin build-up in the blood; ammonia, specifically, is thought to be a key culprit.
2. Clinical Examination: Asterixis, aka, "flapping hand tremor" or "liver flap" is the inability for a patient to sustain a posture due to involuntary, brief, "shock-like" movements.
3. Bedside Testing: To test for asterixis, have a patient sit with closed eyes, outstretched arms, dorsiflexed wrists, and spread fingers – if they suddenly "flap" their hands, this is asterixis (which is indicative of metabolic encephalopathy, and not specific to hepatic dysfunction).
- --
HIGH YIELD
Multi-System Complications Management
1. Coagulopathy: Coagulopathy results from decreased storage of vitamin K and synthesis of clotting factors.
2. Endocrine Manifestations: Elevated estrogen levels can cause spider angiomas (spider-looking collections of blood vessels visible beneath the skin), palmar erythema (reddening of the palms and fingers), and gynecomastia (enlargement of breast tissue in males).
3. Nutritional Impact: Impaired bile flow can lead to hyperlipidemia, jaundice, and malabsorption of GI contents.
4. Glucose Regulation: Glucose metabolism is dynamically altered in liver damage so that patients can be hyper- or hypoglycemic.
Renal Complications Approach
1. Pathophysiology: Renal insufficiency and failure are the result of local vasoconstriction (in response to systemic hypotension) and inflammatory processes that reduce filtration.
2. Clinical Correlation: Spontaneous bacterial peritonitis is often a trigger for renal failure, as it induces the release of pro-inflammatory molecules that contribute to renal dysfunction.
Pulmonary Management
1. Ventilation Assessment: Hepatopulmonary syndrome, in which pulmonary vasodilation leads to a ventilation/perfusion mismatch, reduced oxygenation, and hypoxemia.
Oncologic Surveillance
1. Cancer Risk: Increased risk of liver cancer in progressive liver disease.
- --
Beyond the Tutorial
Advanced Management Strategies
1. Variceal Bleeding Protocol: Initial resuscitation, vasoactive agents (octreotide, terlipressin), antibiotic prophylaxis, and urgent endoscopic intervention with band ligation or sclerotherapy.
2. Refractory Ascites Approach: TIPS procedure, serial large volume paracentesis with albumin, consideration for liver transplant evaluation.
3. Hepatorenal Syndrome Treatment: Vasoconstrictors (norepinephrine, terlipressin) with albumin, avoidance of nephrotoxins, hemodialysis as bridge to transplantation.
4. Encephalopathy Management: Tiered approach with lactulose as first-line therapy, rifaximin for prevention of recurrence, addressing precipitating factors, ammonia-lowering strategies.
Critical Care Management
1. Acute-on-Chronic Liver Failure: Recognition, organ support strategies, and prognostic scoring (CLIF-SOFA, CLIF-C ACLF).
2. Variceal Hemorrhage Resuscitation: Restrictive transfusion strategy (Hgb target 7-8 g/dL), balanced fluid resuscitation, avoiding over-transfusion.
3. Hepatic Hydrothorax Management: Thoracentesis, TIPS evaluation, diuretics, and pleurodesis for refractory cases.
4. Infection Management: Early broad-spectrum antibiotics for suspected infections, diagnostic paracentesis for any deterioration, targeted de-escalation.
Transplant Considerations
1. Listing Criteria: MELD-Na score interpretation, exceptions for hepatocellular carcinoma and other conditions.
2. Contraindications Management: Addressing alcohol use disorder, psychosocial issues, and medical comorbidities.
3. Bridging Therapies: Locoregional therapy for HCC while awaiting transplant, TIPS for refractory ascites/hydrothorax.
4. Post-transplant Care: Immunosuppression management, rejection monitoring, infectious disease prophylaxis.
Quality of Life Considerations
1. Minimal Hepatic Encephalopathy: Recognition through psychometric testing, impact on driving and work performance.
2. Nutritional Support: Avoiding unnecessary protein restriction, managing sarcopenia, micronutrient supplementation.
3. Pruritus Management: Stepwise approach with cholestyramine, rifampicin, naltrexone, and sertraline.
4. Palliative Care Integration: Appropriate timing for goals of care discussions, symptom management in end-stage disease.
