USMLE/COMLEX 3 - Large Vessel Vasculitis
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 3 & COMLEX-USA Level 3 from the Large Vessel Vasculitis tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
- --
VITAL FOR USMLE/COMLEX 3
Clinical Recognition and Immediate Management
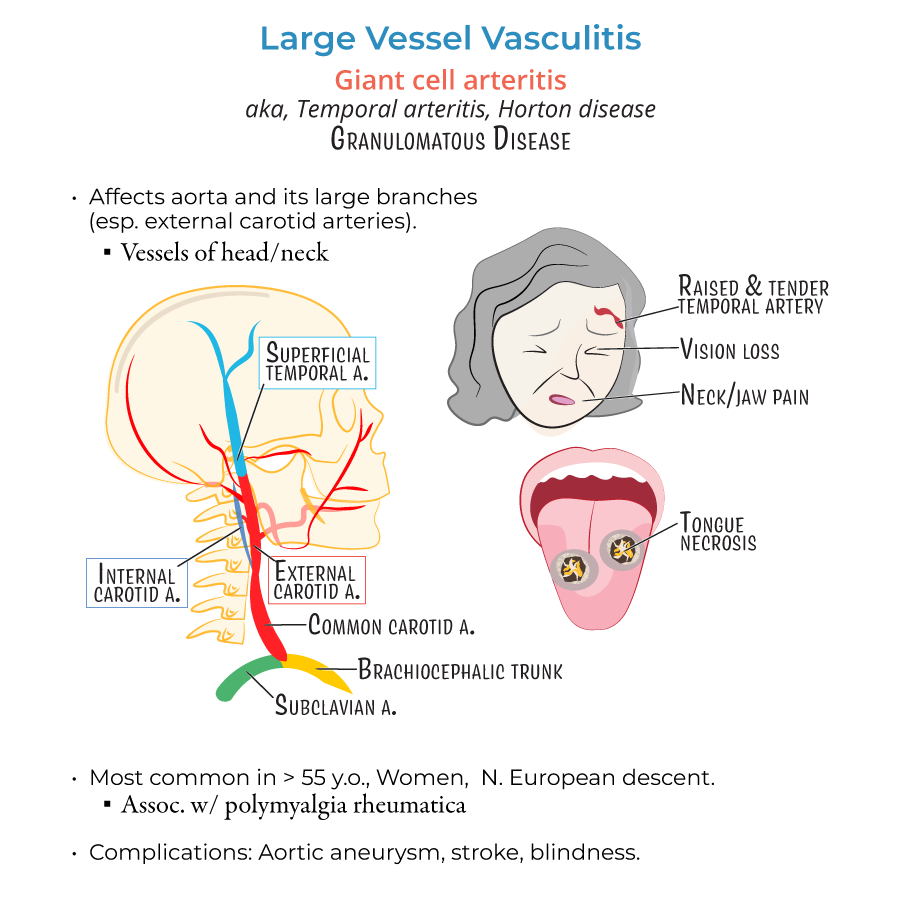
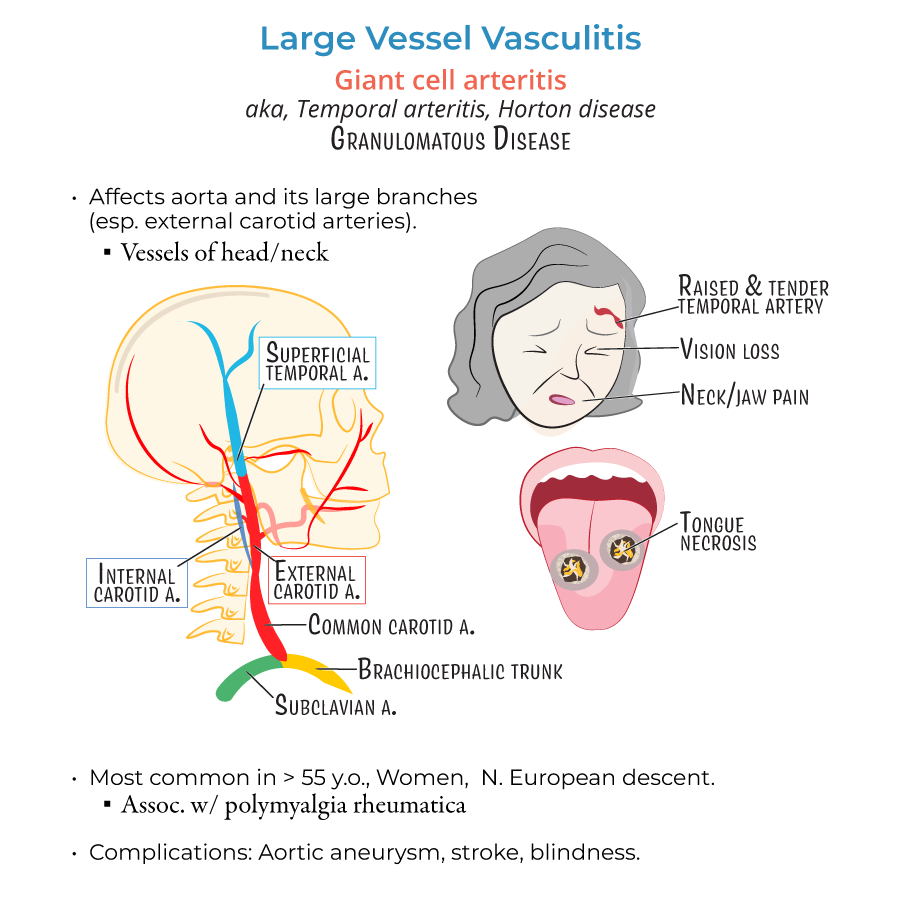
1. Giant Cell Arteritis (GCA) is a medical emergency due to the risk of permanent vision loss.
2. GCA typically affects women >50 years old, especially of Northern European descent.
3. Classic symptoms of GCA:
- New-onset headache (especially temporal)
- Jaw claudication
- Visual changes (amaurosis fugax, blurred vision)
- Scalp tenderness
- Absent pulses in upper extremities
- Asymmetric blood pressures (>10 mmHg difference between arms)
- Arm or leg claudication
- Carotid/subclavian bruits
- --
HIGH YIELD
Pathology and Disease Mechanism
1. Both GCA and Takayasu arteritis are granulomatous large vessel vasculitides.
2. Histologic features of GCA include:
- Multinucleated giant cells
- Chronic inflammatory infiltrates
- Destruction of internal elastic lamina
- Intimal thickening causing luminal narrowing
Clinical Management Nuances
5. Temporal artery biopsy has patchy involvement; a negative result does not completely exclude GCA.
6. For Takayasu, steroids are the first-line treatment, but refractory cases may require methotrexate or azathioprine.
7. Secondary hypertension in Takayasu is commonly due to renal artery stenosis.
8. Regular monitoring of ESR/CRP is important to gauge treatment response and detect relapses.
9. Chronic steroid therapy necessitates bone health management:
- Calcium and vitamin D supplementation
- Bisphosphonates for osteoporosis prevention
- --
Beyond the Tutorial
Advanced Management and Follow-Up
1. In GCA with visual involvement, hospital admission for IV steroids and urgent ophthalmology consultation is warranted.
2. After initial high-dose therapy, taper steroids gradually based on clinical improvement and normalization of ESR/CRP.
3. Tocilizumab (IL-6 receptor antagonist) is an option for GCA patients who cannot tolerate long-term steroids or have frequent relapses.
4. Annual surveillance imaging (CT/MRA) for Takayasu patients is recommended to monitor for progression or recurrence.
5. Watch for complications such as:
- Aortic aneurysm or aortic regurgitation (both diseases)
- Stroke (especially in GCA due to carotid involvement)
- Myocardial ischemia or limb ischemia (especially in Takayasu)
