USMLE/COMLEX 3 - Jaundice
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 3 & COMLEX-USA Level 3 from the Jaundice tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
 Below is information not explicitly contained within the tutorial but important for USMLE & COMLEX 3.
Below is information not explicitly contained within the tutorial but important for USMLE & COMLEX 3.
USMLE Step 3 & COMLEX-USA Level 3: Jaundice
- --
VITAL FOR USMLE/COMLEX 3
Clinical Assessment & Management Framework
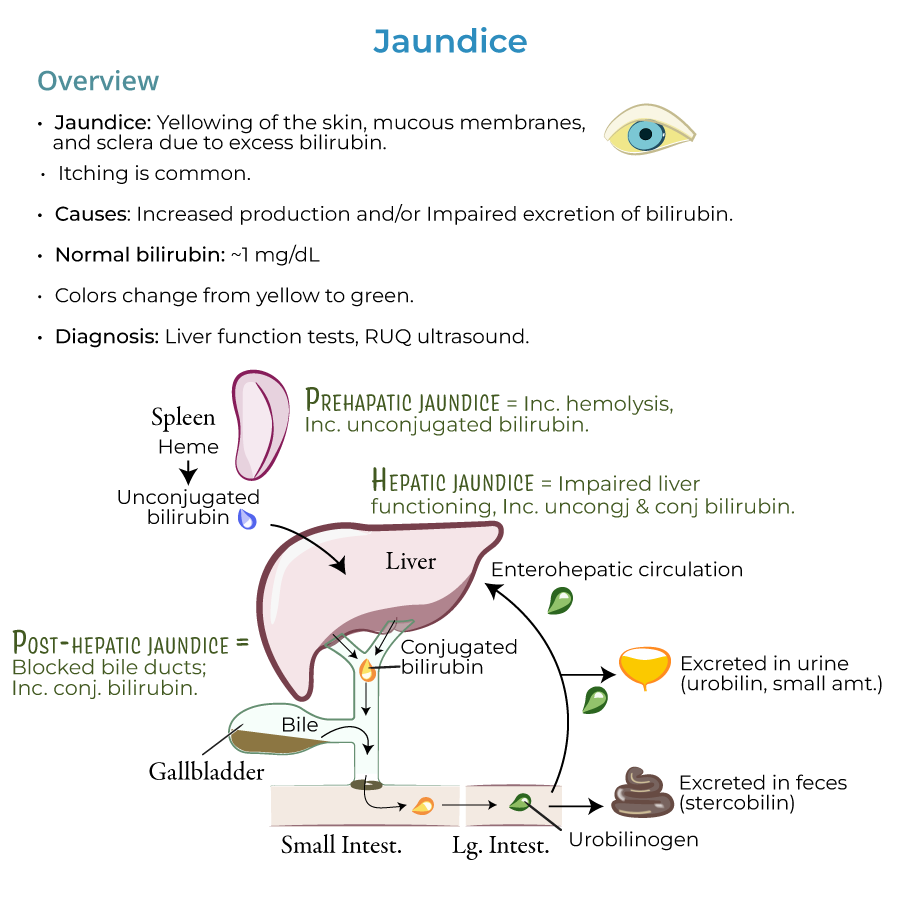
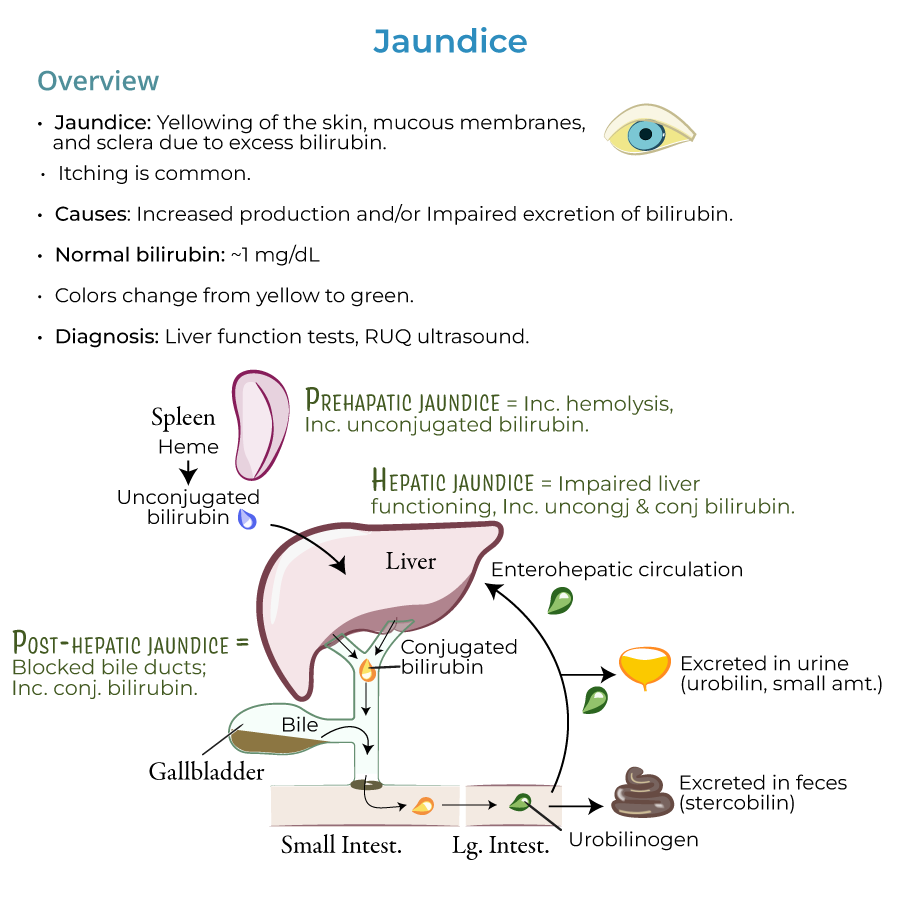
1. Diagnostic framework: Jaundice is a sign of an underlying disorder, so we need to investigate its causes to find the appropriate treatment.
2. Management approach: We use liver function tests and, when biliary obstruction is suspected, right upper quadrant ultrasound to discover and treat the origins of jaundice.
3. Pathophysiologic categorization: Understanding pre-hepatic, hepatic, and post-hepatic causes guides clinical decision-making.
4. HOT Liver mnemonic: Hemolysis, Obstruction, Tumors, and Liver diseases - provides framework for differential diagnosis.
5. Key clinical features: Dark urine indicates conjugated hyperbilirubinemia; pale stools indicate cholestasis.
Critical Management Considerations
1. Neonatal jaundice: Must monitor and treat bilirubin excess promptly because newborns are particularly susceptible to kernicterus, brain damage caused by bilirubin deposits.
2. Cholestasis identification: Cholestasis is a top cause of jaundice requiring prompt intervention.
3. Hepatocellular injury: Hepatocellular injury is a top cause of jaundice requiring careful investigation and management.
4. Hemolytic disorders: Elevated hemolysis is a top cause of jaundice requiring specific management approaches.
5. Emergency conditions: Certain causes like choledocholithiasis, acute viral hepatitis, and drug-induced liver injury require urgent intervention.
- --
HIGH YIELD
Diagnostic Approach & Decision-Making
1. Pre-hepatic causes: Increased hemolysis (sickle cell anemia, G6PD deficiency), inefficient erythropoiesis (thalassemia, pernicious anemia), and increased bilirubin production (massive blood transfusions, hematoma resorption).
2. Hepatic causes: Viral hepatitis, alcoholic hepatitis, autoimmune hepatitis, nonalcoholic steatohepatitis, cirrhosis, Wilson's disease, and drug effects (estrogen, acetaminophen, arsenic).
3. Post-hepatic causes: Gallstone obstruction (cholelithiasis, choledocholithiasis), biliary system inflammation, atresia, or strictures, and ductal compression from tumors or pancreatitis.
4. Special populations: Jaundice in pregnancy (intrahepatic cholestasis) and neonates requires specific management approaches.
5. Medication-related: Medications like protease inhibitors and Rifampin can reduce hepatic bilirubin uptake.
Management of Specific Etiologies
1. Obstructive jaundice: May require endoscopic, surgical, or interventional procedures to relieve obstruction.
2. Genetic disorders: Gilbert syndrome (mild, intermittent), Crigler-Najjar syndrome (risk of kernicterus), Dubin-Johnson syndrome (asymptomatic), and Rotor syndrome (benign) require different management approaches.
3. Hepatitis management: Different approaches for viral, alcoholic, autoimmune hepatitis based on specific etiology.
4. Neonatal jaundice types: Physiologic jaundice, breast milk jaundice, and breastfeeding jaundice require different management strategies.
5. Infiltrative disorders: Amyloidosis, lymphoma, sarcoidosis, and tuberculosis require specific treatment approaches.
Clinical Complications & Monitoring
1. Kernicterus risk: Newborns are particularly susceptible to bilirubin-induced brain damage requiring vigilant monitoring.
2. Cholestasis sequelae: Long-standing cholestasis can lead to fat-soluble vitamin deficiencies and pruritus requiring management.
3. Hepatic encephalopathy: Progressive liver dysfunction can lead to neurological complications requiring prompt intervention.
4. Coagulopathy: Liver dysfunction can disrupt clotting factor production requiring monitoring and potential prophylaxis.
5. Portal hypertension: Advanced liver disease can lead to varices and ascites requiring specific management strategies.
Special Clinical Scenarios
1. Pregnancy-associated jaundice: Intrahepatic cholestasis of pregnancy requires close monitoring of both mother and fetus.
2. Sepsis-induced jaundice: Recognition and management of sepsis-associated cholestasis is important in critically ill patients.
3. TPN-associated cholestasis: Total parenteral nutrition can cause intrahepatic cholestasis requiring adjustment of feeding strategies.
4. Mixed disorders: Patients can present with multiple causes of jaundice simultaneously, requiring comprehensive management.
5. Palliative approaches: Management of malignant biliary obstruction requires consideration of quality of life and overall prognosis.
- --
Beyond the Tutorial
Advanced Clinical Decision Making
1. Risk stratification: Tokyo criteria for severity grading of acute cholangitis and cholecystitis guide management intensity.
2. Early vs. delayed ERCP: Timing of intervention in gallstone pancreatitis with jaundice based on clinical markers of severity.
3. Antibiotic selection: Empiric coverage for suspected cholangitis should include gram-negative and anaerobic organisms.
4. Futility assessment: When to consider palliative biliary stenting vs. surgical bypass in malignant obstruction.
5. Transfer criteria: Indications for referring patients with acute liver failure to transplant centers (King's College criteria).
Therapeutic Interventions
1. ERCP techniques: Biliary sphincterotomy, stone extraction, stent placement, and post-procedure management.
2. Percutaneous approaches: When to choose PTBD (percutaneous transhepatic biliary drainage) over ERCP.
3. Surgical options: Timing of cholecystectomy after gallstone pancreatitis and approach for Mirizzi syndrome.
4. Liver transplantation: Indications, contraindications, and management of patients awaiting transplantation.
5. Novel therapies: Use of fibrates for primary biliary cholangitis not responding to UDCA; Y-90 for hepatocellular carcinoma.
Management of Complications
1. Post-ERCP pancreatitis: Risk factors, prevention strategies, and management approaches.
2. Recurrent pyogenic cholangitis: Long-term management strategy including surveillance and prophylaxis.
3. Refractory pruritus: Stepwise approach using cholestyramine, rifampin, naltrexone, and sertraline.
4. Resistant ascites: Role of TIPS, albumin infusion, and midodrine in managing hepatorenal syndrome.
5. Cholangiocarcinoma surveillance: Evidence-based screening protocols for patients with primary sclerosing cholangitis.
Population-Specific Considerations
1. Elderly patients: Drug dosing adjustments and procedural risk modifications in patients with jaundice.
2. Immunocompromised hosts: Differential diagnosis expansion and management modifications in HIV, post-transplant patients.
3. Pregnant patients: Safety profiles of diagnostic modalities and medications for managing jaundice during pregnancy.
4. Intensive care patients: Management of jaundice in the context of multiorgan failure and vasopressor dependence.
5. Outpatient follow-up: Evidence-based protocols for monitoring ambulatory patients after hospitalization for jaundice.
Systems-Based Practice Issues
1. Cost-effective approach: Step-wise use of diagnostic modalities to minimize unnecessary testing.
2. Readmission prevention: Discharge planning for patients with resolved jaundice to prevent recurrence.
3. Telehealth monitoring: Remote monitoring protocols for patients with chronic liver disease and intermittent jaundice.
4. Interdisciplinary care: Coordination between gastroenterology, surgery, interventional radiology, and primary care.
5. Quality metrics: Evidence-based quality indicators for management of jaundice in hospitals and outpatient settings.
