USMLE/COMLEX 3 - Ischemic Heart Disease Symptoms and Treatments
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 3 & COMLEX-USA Level 3 from the Ischemic Heart Disease Symptoms and Treatments tutorial, as well as points of interest at the end that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
 Below is information not explicitly contained within the tutorial but important for USMLE & COMLEX 3.
Below is information not explicitly contained within the tutorial but important for USMLE & COMLEX 3.
- --
VITAL FOR USMLE/COMLEX 3
Clinical Decision-Making in Ischemic Heart Disease
1. Differentiating angina types is critical for appropriate management: stable vs. unstable vs. vasospastic vs. microvascular angina.
2. Unstable angina requires immediate evaluation as an acute coronary syndrome with risk of progression to myocardial infarction.
3. Silent ischemia requires aggressive management despite lack of symptoms, as it's associated with increased morbidity and mortality.
4. Non-ischemic mimics must be ruled out: aortic stenosis, anemia, arrhythmias, and hypertrophic cardiomyopathy.
5. Diagnosis involves interpretation of ECG, echocardiogram, stress testing, angiograms, and CT scans in clinical context.
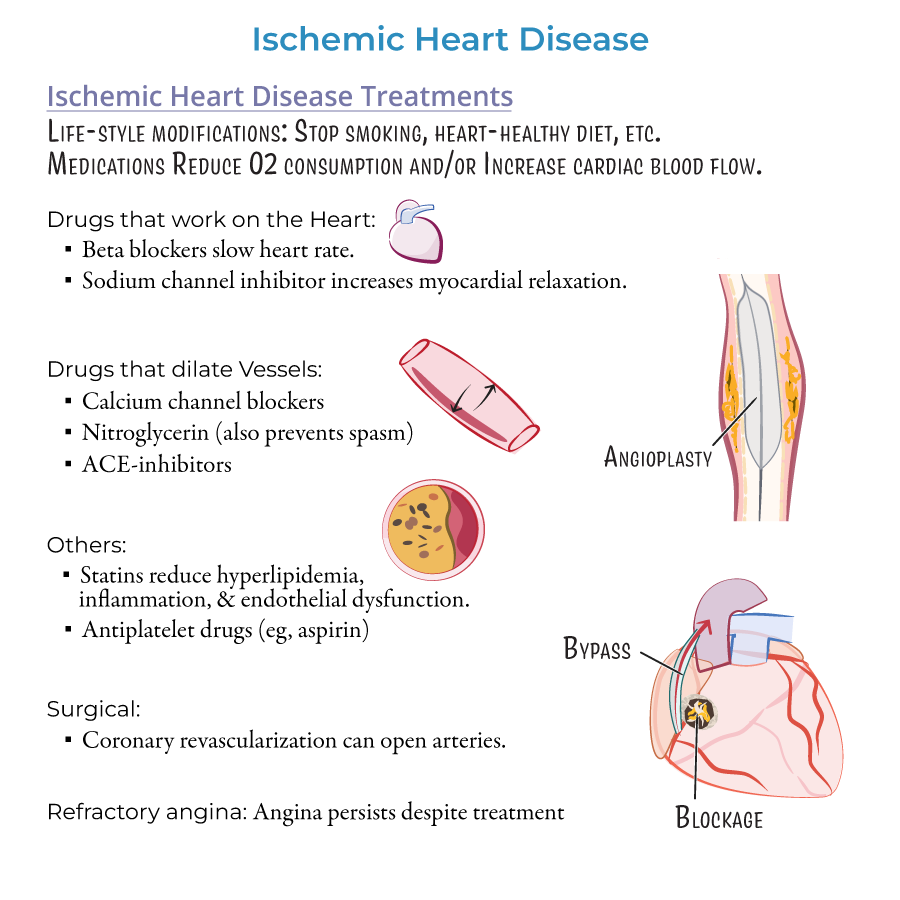
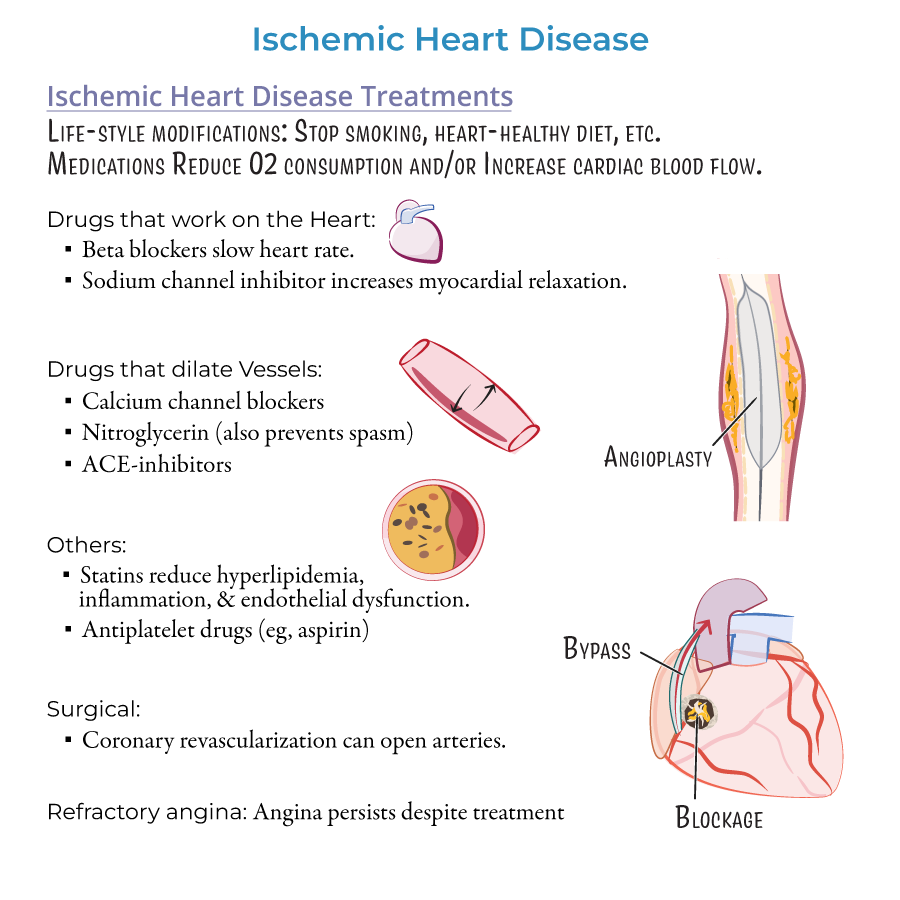
Evidence-Based Treatment Algorithms
1. Stable angina management includes stratified approach from lifestyle modifications to pharmacotherapy to revascularization.
2. Vasospastic angina responds to nitrates and calcium-channel blockers but not beta-blockers, which can worsen symptoms.
3. Microvascular angina requires specialized assessment with PET or cardiac MR to evaluate coronary microvascular blood flow.
4. Refractory angina represents a significant management challenge requiring innovative approaches for "no-option" patients.
5. Revascularization decisions between PCI vs. CABG depend on coronary anatomy, comorbidities, and patient preferences.
- --
HIGH YIELD
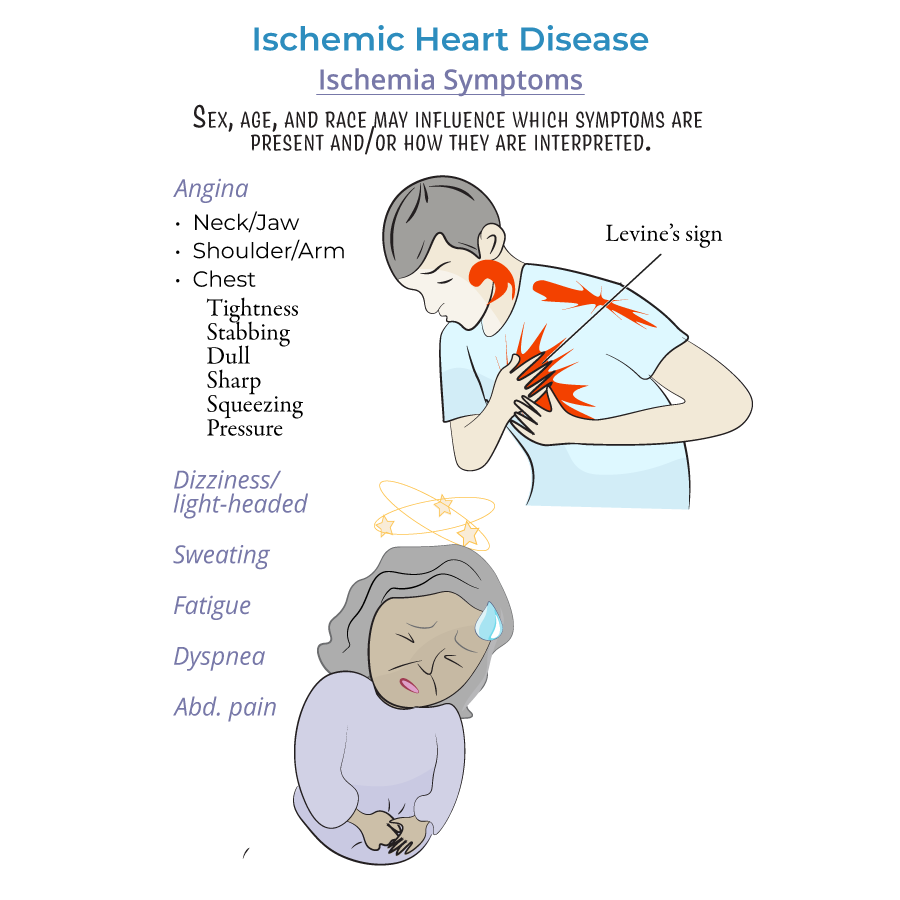
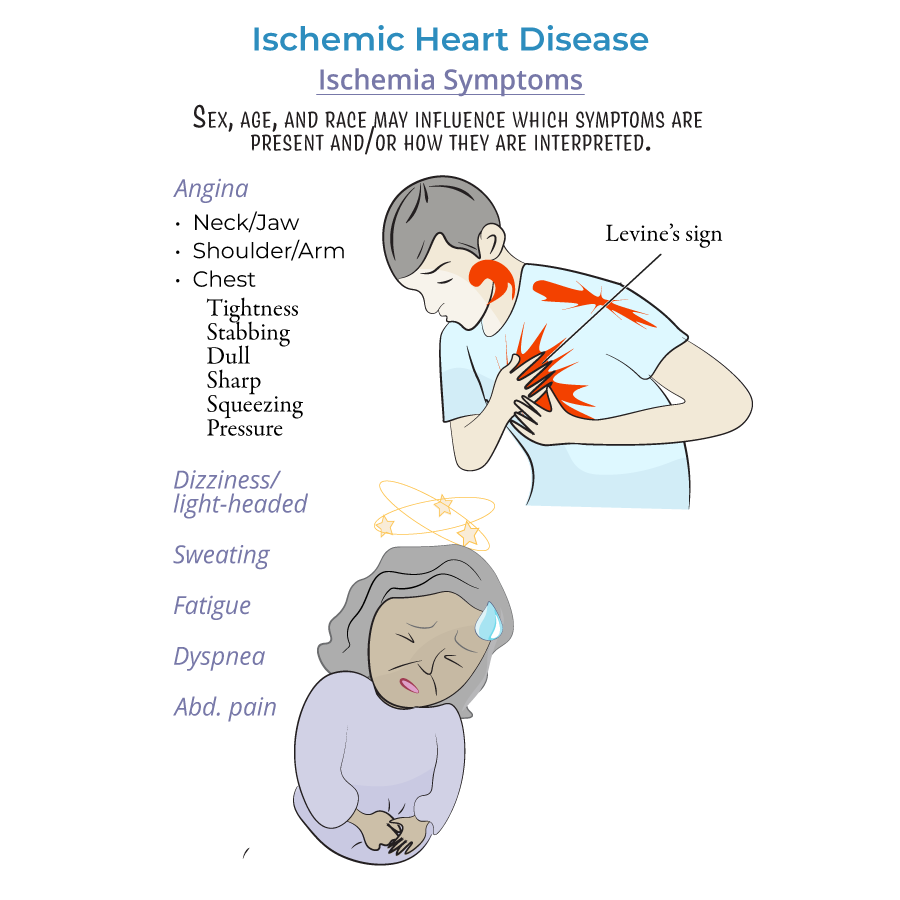
Nuanced Clinical Presentation
1. Demographic variations in presentation require high clinical suspicion: women, elderly, diabetics, and racial minorities often present atypically.
2. Levine's sign (clenched fist over sternum) should prompt immediate consideration of cardiac ischemia.
3. Gastrointestinal symptoms in patients of African descent may mask underlying cardiac ischemia.
4. Women with ischemic heart disease frequently present with light-headedness, dizziness, and persistent fatigue rather than classic angina.
5. Risk stratification tools should be applied to all patients with suspected ACS to guide management decisions.
Advanced Pharmacotherapy
1. Nitrate therapy requires careful dosing to prevent tolerance; nitrate-free intervals of 10-14 hours typically recommended.
2. Beta-blockers selection should consider cardioselectivity, intrinsic sympathomimetic activity, and lipophilicity based on patient factors.
3. Calcium channel blockers subtypes (dihydropyridine vs. non-dihydropyridine) have different effects on heart rate and contractility.
4. Ranolazine offers anti-anginal effects without significantly affecting hemodynamics; useful in patients with hypotension or bradycardia.
5. Statin intensity should match patient's cardiovascular risk; high-intensity statins preferred for secondary prevention.
6. Antiplatelet therapy duration depends on clinical context, stent type, bleeding risk, and recurrent ischemic risk.
7. Post-revascularization management includes dual antiplatelet therapy, statins, and optimization of all modifiable risk factors.
- --
Beyond the Tutorial
Complex Clinical Scenarios
1. MINOCA (Myocardial Infarction with Non-Obstructive Coronary Arteries) requires specialized evaluation including CMR and consideration of vasospasm, thromboembolism, or SCAD.
2. INOCA (Ischemia with Non-Obstructive Coronary Arteries) management focuses on microvascular and vasomotor dysfunction.
3. Post-CABG ischemia evaluation must differentiate between graft failure, progression of native disease, or incomplete revascularization.
4. Perioperative management of patients with coronary disease requires risk stratification and appropriate bridging strategies.
Emerging Therapeutic Approaches
1. SGLT2 inhibitors have shown cardiovascular benefit beyond glycemic control in patients with diabetes and established CVD.
2. PCSK9 inhibitors provide additional LDL reduction for high-risk patients not reaching goals on maximal statin therapy.
3. Coronary CTO (Chronic Total Occlusion) interventions have evolved with improved success rates and potential symptomatic benefit.
4. Cardiac rehabilitation participation significantly reduces morbidity and mortality but remains underutilized.
