USMLE/COMLEX 3 - Ischemic Heart Disease Pathophysiology
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 3 & COMLEX-USA Level 3 from the Ischemic Heart Disease tutorial, as well as points of interest at the end that are not directly addressed in this tutorial but should help you prepare for the boards.
 2. Coronary microvascular dysfunction mechanisms:
2. Coronary microvascular dysfunction mechanisms:
 2. Clinical presentation patterns:
Below is additional information important for USMLE Step 3 not explicitly contained within the tutorial.
2. Clinical presentation patterns:
Below is additional information important for USMLE Step 3 not explicitly contained within the tutorial.
- --
VITAL FOR USMLE STEP 3
Comprehensive Patient Assessment
1. Risk stratification: Consider complex interactions of multiple factors:
- Traditional risk factors: Family history, age, smoking, hypertension, diabetes, hyperlipidemia
- Sex-specific considerations: Early menopause, gestational diabetes/hypertension
- Inflammatory conditions: Chronic inflammatory rheumatoid diseases
- Demographic variations: Risk factors may have stronger impacts in women
- Leading cause of death in both men and women requires vigilant assessment
- Sex and racial differences in presentation may delay diagnosis and treatment
- Consider ischemic heart disease in atypical presentations, especially in women
Diagnostic Algorithm for Suspected Ischemia
1. Critical interpretation of normal angiography:
- Up to 50% of patients with suspected ischemia have no significant obstruction
- Normal angiogram does not exclude ischemic heart disease
- Further investigation warranted with continued symptoms
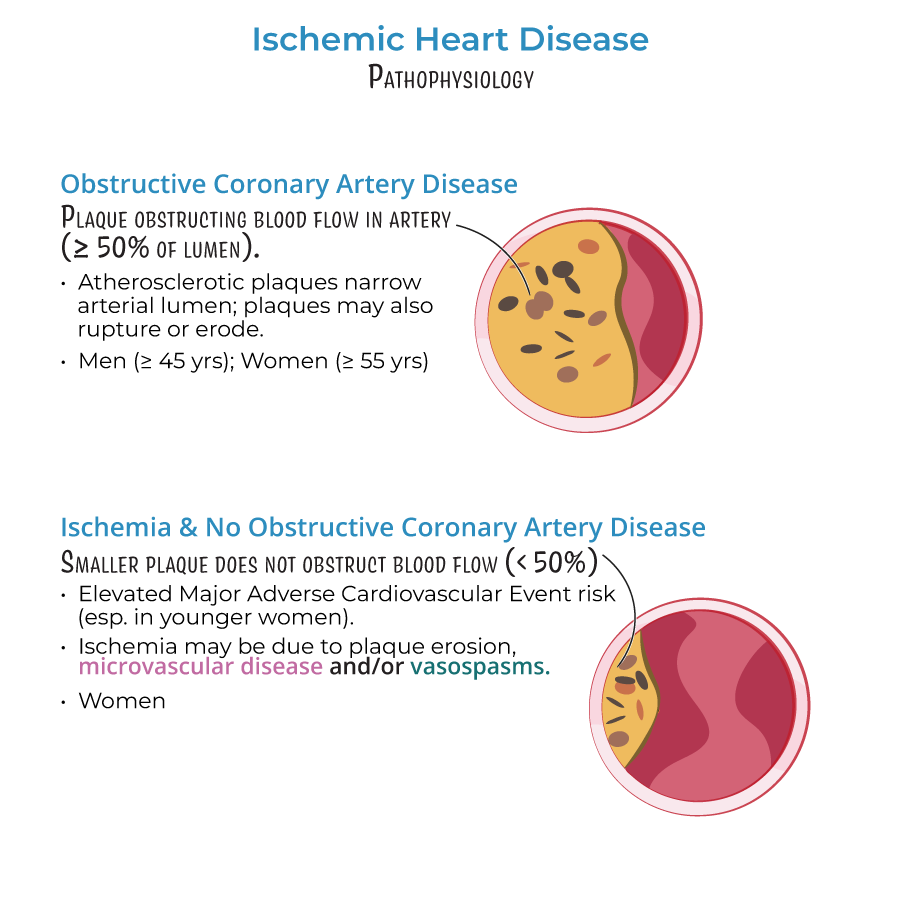
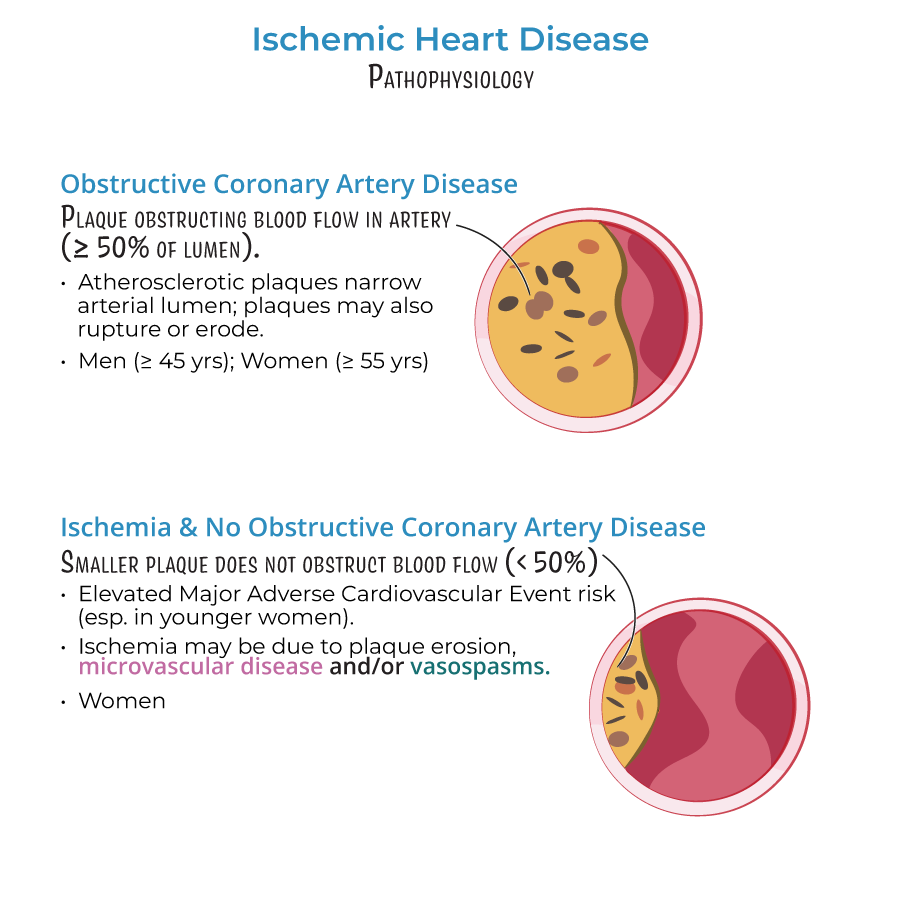
- Obstructive CAD (≥50% stenosis): More common in men >45, women >55
- INOCA (<50% stenosis): More common in women, ~30% of men
- Presence of MACE risk despite normal angiogram requires investigation of:
- Microvascular dysfunction
- Vasospasm
- Plaque erosion
Management Implications by Pathophysiology
1. Plaque stabilization strategies:
- Recognize limitations of statin therapy: Effective for rupture prevention but less impact on erosion
- Plaque erosion increasingly significant cause of ACS despite lipid-lowering therapy
- Consider endothelial dysfunction treatments in high-risk patients
- Recognize as significant cause of INOCA
- Can coexist with obstructive CAD requiring dual treatment approach
- Consider testing and treatment in both men and women (affects both sexes nearly equally)
- --
HIGH YIELD
Advanced Pathophysiologic Considerations
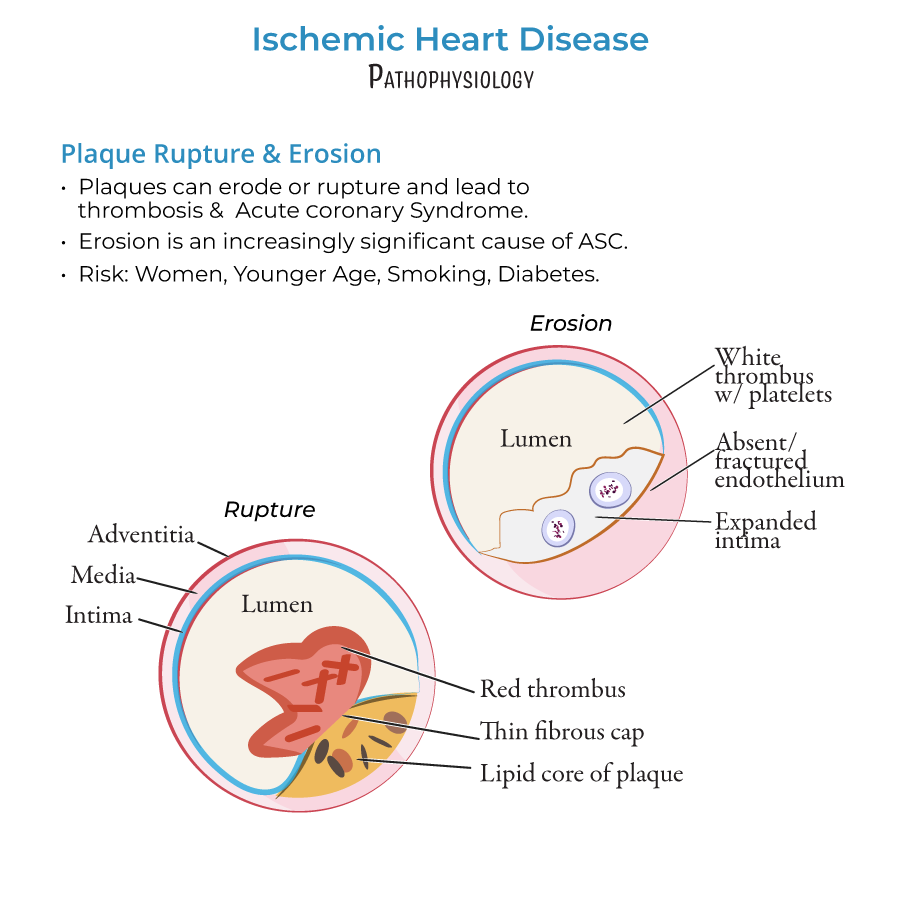
1. Plaque rupture vs. erosion:
- Plaque rupture:
- Tears in fibrous caps releasing thrombogenic contents
- Characterized by lipid cores, thin caps, fibrin-rich "red thrombi"
- Reduced frequency due to widespread statin use
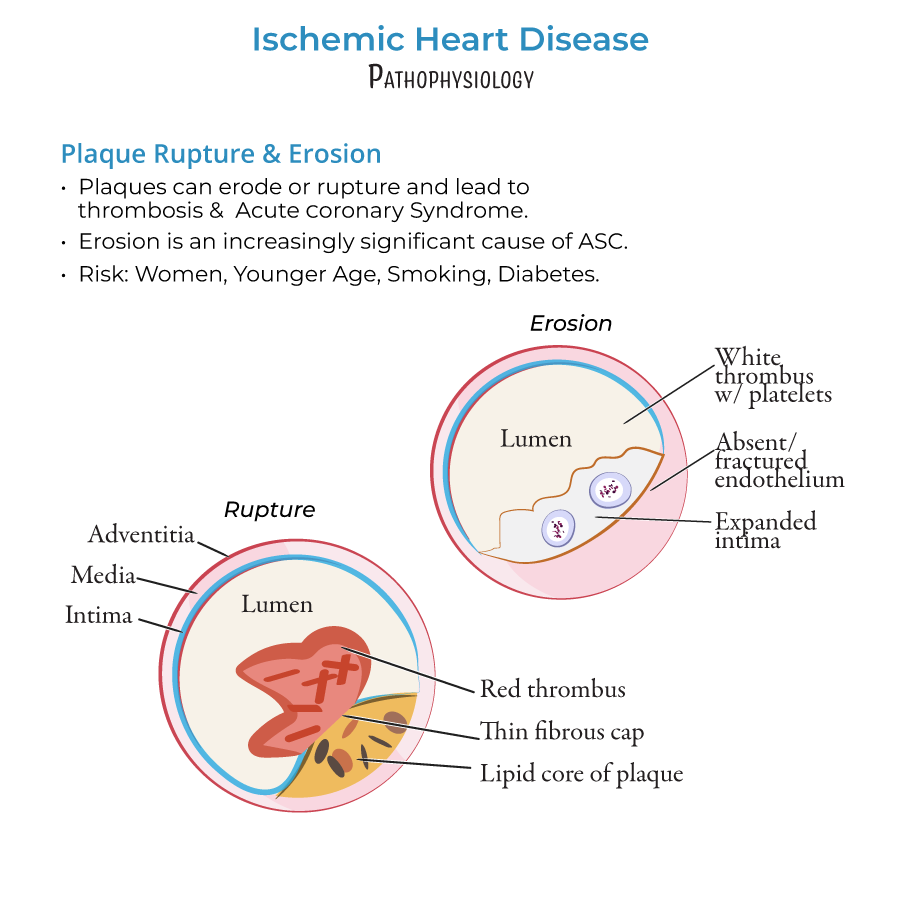
- Plaque erosion:
- More common in women, young patients, smokers, diabetics
- Thick cap plaques with endothelial dysfunction/absence
- Platelet-rich "white thrombi"
- Not prevented by lipid-lowering therapy
 2. Coronary microvascular dysfunction mechanisms:
2. Coronary microvascular dysfunction mechanisms:
- Structural: Arteriole remodeling affects wall:lumen ratio
- Functional: Impaired vasodilation, endothelial dysfunction
- Pattern: Diffuse, patchy ischemia vs. localized epicardial lesions
- Prevalence: Similar in both sexes
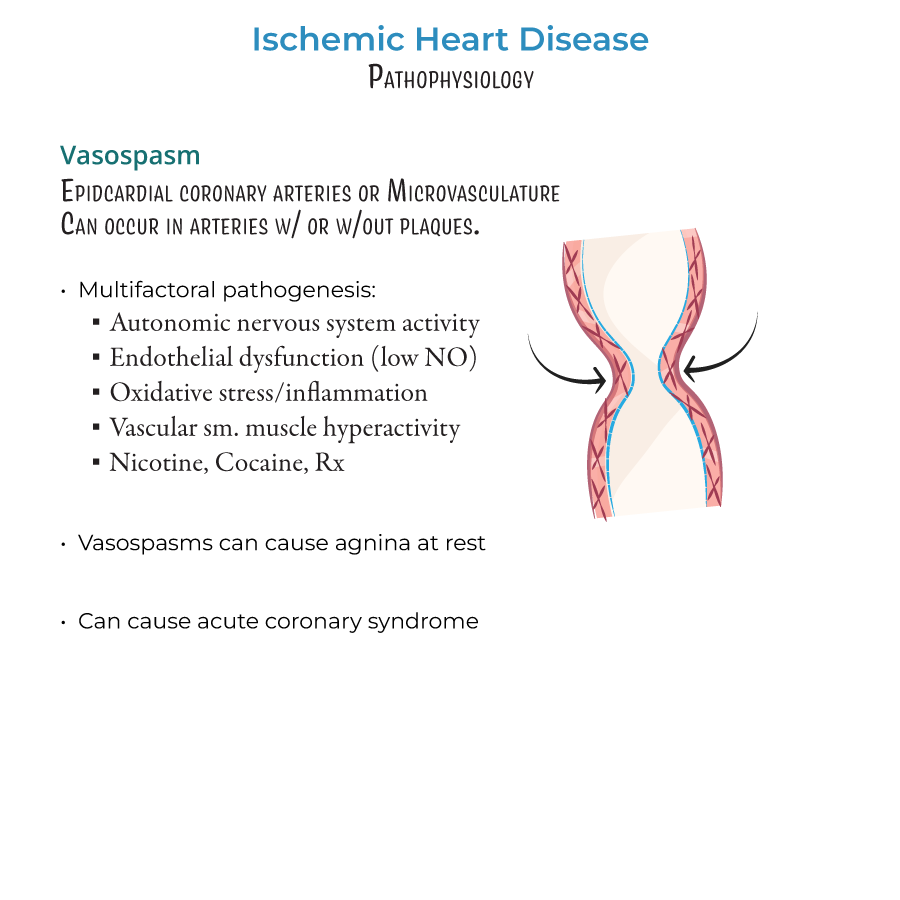
Vasospasm: Comprehensive Management
1. Potential triggers requiring clinical management:
- Enhanced autonomic nervous system activity
- Endothelial dysfunction (especially reduced nitric oxide)
- Oxidative stress and inflammation
- Vascular smooth muscle hyperactivity
- Modifiable factors: nicotine, cocaine, vasoconstricting medications
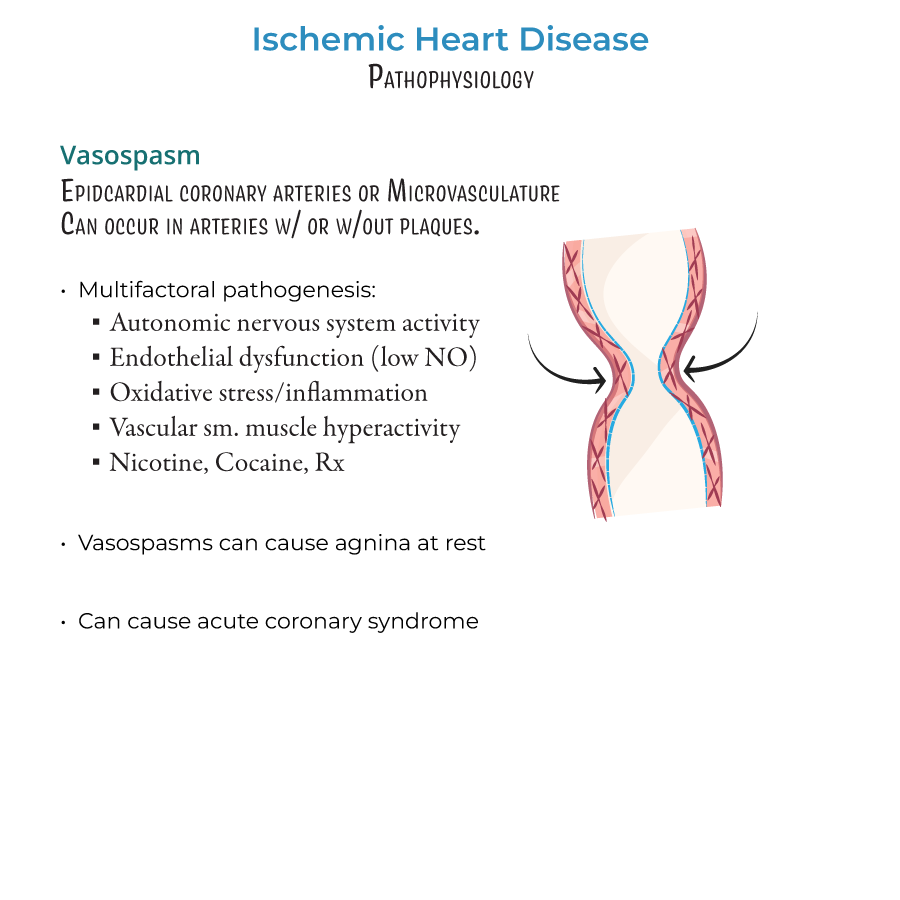 2. Clinical presentation patterns:
2. Clinical presentation patterns:
- Angina occurring at rest rather than with exertion
- Includes variant (Prinzmetal's) and microvascular angina
- Can occur with or without underlying stenosis
Integrated Approach to Complex Ischemic Syndromes
1. Four mechanisms requiring different management approaches:
- Obstructive coronary artery disease (≥50% stenosis)
- INOCA (<50% stenosis)
- Plaque rupture/erosion
- Coronary microvascular dysfunction
- Risk assessment must be sex-specific (women may have atypical presentations)
- Coronary angiography limitations must inform diagnostic algorithms
- Absence of obstruction requires consideration of alternative mechanisms
- Treatment must target specific underlying mechanism(s) for optimal outcomes
- --
Beyond the Tutorial
Acute Management Decisions
1. Early reperfusion strategies:
- Door-to-balloon time targets (<90 minutes)
- Fibrinolysis considerations when PCI unavailable or delayed
- Pharmacoinvasive approaches
- Complete vs. culprit-only revascularization in multivessel disease
- Aspirin loading and maintenance dosing
- P2Y12 inhibitor selection based on patient characteristics
- Clopidogrel: Lower bleeding risk, genetic variability
- Ticagrelor: Faster onset, reversible binding, mortality benefit
- Prasugrel: Potent inhibition, contraindications in high-risk groups
- Duration based on clinical scenario, stent type, bleeding risk
- De-escalation strategies for high bleeding risk patients
- Unfractionated heparin vs. LMWH vs. fondaparinux
- Bivalirudin considerations
- Triple therapy management (DAPT + anticoagulant) for AF patients
Long-term Management and Prevention
1. Comprehensive secondary prevention:
- Risk factor modification targets
- BP: <130/80 mmHg for most patients
- LDL-C: <70 mg/dL or ≥50% reduction from baseline
- HbA1c: Individualized targets, generally <7%
- Cardiac rehabilitation (Class I recommendation)
- Depression screening and management
- Sleep apnea evaluation
- Sexual dysfunction assessment and treatment
- High-intensity statins
- PCSK9 inhibitors for uncontrolled LDL despite statins
- ACE inhibitors/ARBs: Especially with LV dysfunction, diabetes, HTN
- Beta-blockers: Duration considerations based on LV function
- Aldosterone antagonists for selected patients
- SGLT2 inhibitors/GLP-1 RAs for diabetic patients (CV benefit)
- Women: Address sex-specific risk factors, recognize atypical presentations
- Elderly: Medication adjustments, fall risk, cognitive assessment
- Diabetics: Aggressive prevention, glycemic control strategy
- Chronic kidney disease: Medication adjustments, contrast minimization
- Prior CABG: Graft evaluation strategies, anti-anginal therapy
Emerging Management Approaches
1. Targeted therapies by pathophysiology:
- Microvascular dysfunction: Ranolazine, ACE inhibitors, statins
- Vasospastic angina: CCBs, nitrates, avoid beta-blockers
- Endothelial dysfunction: L-arginine, statins, ACE inhibitors
- Inflammation reduction: Colchicine, PCSK9 inhibitors
- Intravascular imaging (IVUS, OCT) guided PCI
- Physiologic assessment (FFR, iFR) for intermediate lesions
- Complete revascularization strategies
- Chronic total occlusion approaches
- High bleeding risk stent platforms
- STEMI networks and regional STEMI care
- Telemedicine for rural areas
- Quality metrics and performance improvement
- Cost-effective care strategies
- Shared decision-making tools
- Heart team approach to complex cases
