USMLE/COMLEX 3 - Inflammatory Bowel Disease
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 3 & COMLEX-USA Level 3 from the Inflammatory Bowel Disease tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
- --
VITAL FOR USMLE/COMLEX 3
Inflammatory Bowel Disease (IBD)
1. Diagnosis relies on endoscopy.
2. Associated with neoplasia, influenced by duration and severity of disease.
3. Extraintestinal manifestations: Most common are skin lesions (in up to 40% of patients), uveitis, and arthritis.
4. Less common but potentially deadly complications: involvement of liver/gallbladder, lung, pancreas, and kidneys.
5. Most patients diagnosed in teens/early 20s; ulcerative colitis has a second "peak" in patients in their 60's or 70's.
Crohn's Disease
1. Clinical presentation: Abdominal cramping (often on the right side, where the ileum meets the large intestine), diarrhea (potentially bloody), fever and malaise, weight loss (due to malabsorption), perianal lesions (25% of patients).
2. Complications: Problems related to fistulas, fissures, and obstructive strictures; dysplasia and adenocarcinoma; and anemia from chronic blood loss.
3. Treatment: Patients advised to avoid cigarette smoking and nicotine (exacerbates inflammation), anti-inflammatories, immune suppressors, surgery to remove parts of the colon.
4. Can affect any segment of GI tract, but most commonly involves ileum and colon.
5. Rectum usually spared (unlike ulcerative colitis).
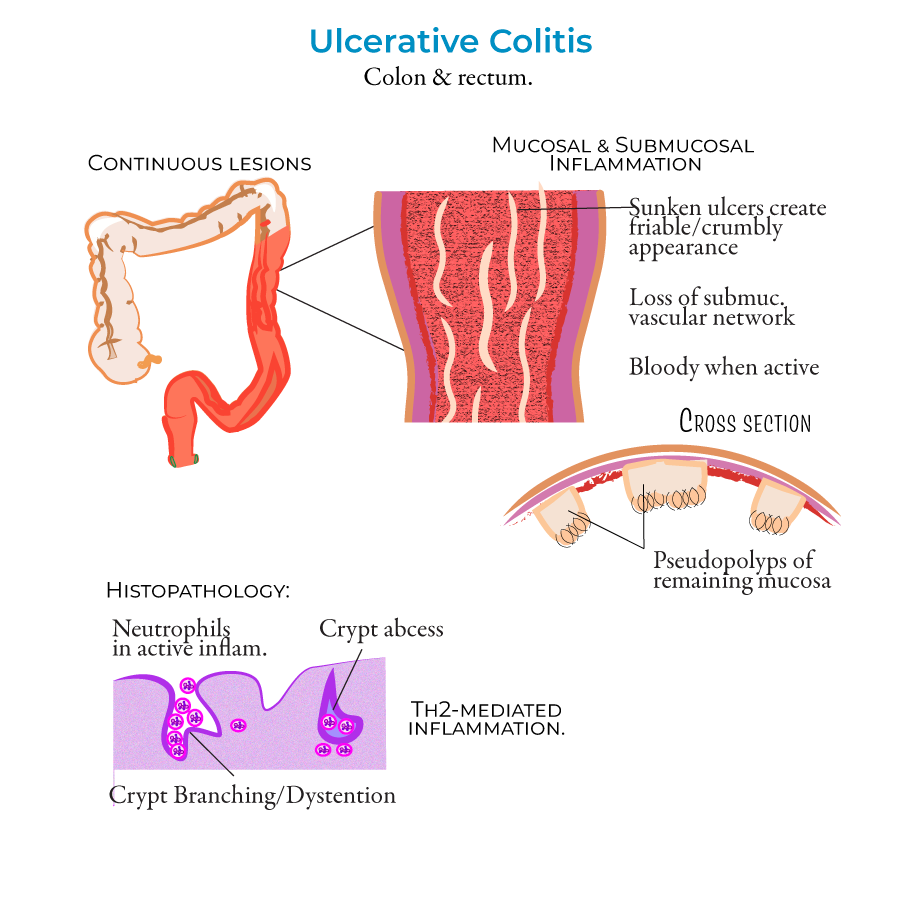
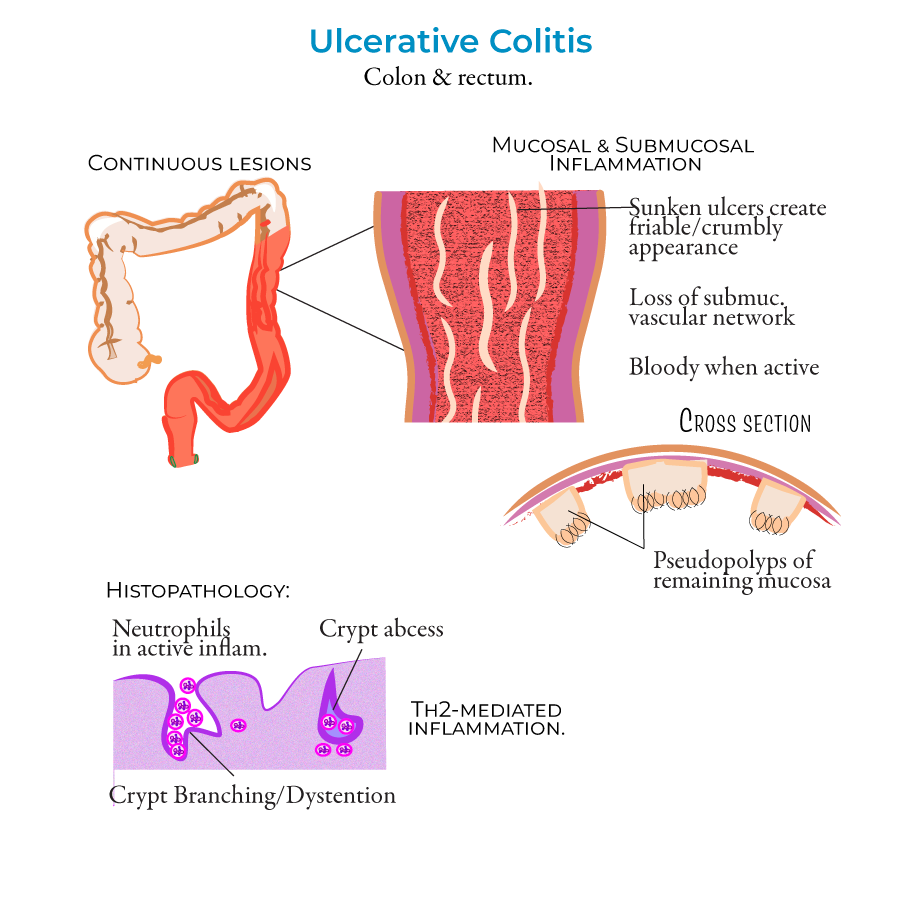
Ulcerative Colitis
1. Clinical presentation: Bloody diarrhea with rectal bleeding, abdominal pain, fever, and weight loss.
2. Complications: Toxic ulceritis, toxic megacolon, intestinal perforation. Dysplasia and adenocarcinoma more likely when entire colon is involved (pancolitis).
3. Treatment: Anti-inflammatories, immune suppressors, and colectomy. Patients who smoke cigarettes more likely to experience bouts upon quitting.
4. Restricted to the colon and rectum with continuous lesions.
5. Mucosa appears bloody with friable appearance during active inflammation.
- --
HIGH YIELD
Inflammatory Bowel Disease Management
1. Environmental factors are important in management (diet, cigarette smoking, medications).
2. Result of detrimental interactions between host immune response, intestinal microbiota, and intestinal barrier defects - relevant for therapeutic targeting.
3. About 5-15% of cases are considered "indeterminant" colitis - important for management decisions when diagnosis is unclear.
4. Genetic factors play a role (e.g., mutations in NOD2 associated with Crohn's disease) - may influence family counseling.
Crohn's Disease Management
1. Many studies suggest a female predominance - relevant for family planning discussions.
2. Lesion progression understanding guides treatment intensity:
- Aphthous erosions (early shallow whitish sores)
- Longitudinal "bear claw" ulcers (look like rake dragged down GI lining)
- Cobblestone appearance (as tissue becomes crowded with ulcers)
- Fissures form and progress to fistulas (connecting to abdominal/pelvic cavity or other organs)
Ulcerative Colitis Management
1. Inflammation destroys submucosal vascular network - contributes to bleeding.
2. Remaining mucosa creates "pseudopolyps" - important to distinguish from adenomatous polyps.
3. Histology: crypt abscesses with neutrophils - guides acute treatment decisions.
4. Inflammation is Th2 cell-mediated - relevant for targeted therapies.
5. Patients who smoke cigarettes more likely to experience bouts upon quitting - important for counseling and relapse prevention.
Treatment Decision Factors
1. Smoking cessation advised for Crohn's disease but may temporarily worsen ulcerative colitis - requires different counseling approaches.
2. Different inflammatory patterns (Th1/Th17 in CD vs Th2 in UC) guide targeted therapy selection.
3. Key anatomical differences influence surgical approaches:
- CD = transmural inflammation, skip lesions, any GI segment, rectum usually spared
- UC = mucosal/submucosal inflammation, continuous lesions, colon/rectum only
- --
Beyond the Tutorial
Acute Management
1. Acute severe ulcerative colitis:
- Initial assessment with Truelove and Witts criteria
- IV hydrocortisone 100mg q6h as first-line therapy
- Daily clinical reassessment with CRP, abdominal X-ray
- Rescue therapy (infliximab or cyclosporine) if no improvement by day 3-5
- Emergency colectomy indications and timing
- Distinguishing inflammatory vs. fibrotic obstruction
- Role of bowel rest, antibiotics, and corticosteroids
- Abscess management: antibiotics vs. percutaneous drainage vs. surgical drainage
- Thresholds for surgical intervention
- Recognition: >6cm transverse colon, systemic toxicity
- Management: NPO, NG suction, fluid resuscitation, antibiotics
- Monitoring parameters and colectomy indicators
- Post-recovery management strategies
Chronic Management Strategies
1. Treatment selection algorithm:
- Disease phenotype-based therapy (inflammatory, stricturing, penetrating)
- Location-based therapy (ileal, ileocolonic, colonic, upper GI)
- Risk stratification for aggressive disease
- Step-up vs. top-down approaches based on individual risk profile
- Proactive vs. reactive testing strategies
- Target trough levels for different biologics
- Anti-drug antibody interpretation and management
- Dose optimization protocols
- Benefits vs. risks of combined immunosuppression
- Duration of combination therapy
- Withdrawal strategies for different agents
- Infection risk mitigation during combination therapy
- Primary non-response vs. secondary loss of response
- Objective assessment of disease activity
- Within-class vs. out-of-class switching
- Surgery timing in medically refractory disease
Special Populations Management
1. Pregnancy and IBD:
- Pre-conception counseling and optimization
- Medication safety profiles by trimester
- Disease activity monitoring during pregnancy
- Delivery mode considerations
- Postpartum flare prevention
- Differential diagnosis considerations
- Comorbidity impact on treatment selection
- Drug interaction and polypharmacy management
- Infection risk mitigation strategies
- Vaccination guidelines
- Structured transition programs
- Self-management skill development
- Medication adherence strategies
- Psychosocial support during transition
Complication Management
1. Fistulizing Crohn's disease:
- Classification systems: simple vs. complex
- Combined medical-surgical approach
- Post-operative prophylaxis strategies
- Monitoring and recurrence prevention
- Inflammatory vs. fibrotic differentiation
- Endoscopic dilation techniques and protocols
- Strictureplasty vs. resection decision-making
- Post-dilation monitoring and recurrence prevention
- Risk stratification models
- Surveillance intervals based on risk factors
- Chromoendoscopy techniques
- Dysplasia management algorithms
- Joint manifestations: axial vs. peripheral
- Dermatologic manifestations: pyoderma vs. erythema nodosum vs. psoriasis
- Ocular manifestations: urgent referral criteria
- PSC-IBD: surveillance and management
Health Maintenance
1. Vaccination guidelines:
- Live vs. inactivated vaccines based on immunosuppression
- Pre-biologic vaccination protocol
- Annual influenza and pneumococcal vaccination
- Herpes zoster vaccination strategy
- DEXA scanning frequency
- Vitamin D and calcium supplementation
- Bisphosphonate indications
- Steroid-sparing strategies
- Depression and anxiety screening
- CBT and mindfulness-based interventions
- Stress management impact on disease course
- Addressing stigma and quality of life issues
- Malnutrition screening tools
- Targeted supplementation strategies
- Enteral nutrition as primary or adjunctive therapy
- Dietary pattern recommendations based on disease phenotype
