USMLE/COMLEX 3 - Hypertension Pathophysiology
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 3 & COMLEX-USA Level 3 from the Blood Pressure Regulation and Hypertension tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
 3. Adrenal cortex and aldosterone:
Below is information not explicitly contained within the tutorial but important for USMLE Step 3 & COMLEX Level 3.
3. Adrenal cortex and aldosterone:
Below is information not explicitly contained within the tutorial but important for USMLE Step 3 & COMLEX Level 3.
- --
VITAL FOR USMLE/COMLEX 3
Advanced Blood Pressure Regulation
1. Primary determinants of mean arterial pressure:
- Cardiac output: product of heart rate and stroke volume
- Total peripheral resistance: primarily determined by vasoconstriction of small arteries and arterioles
- Application to management: therapies target one or both components
- Blood volume significantly contributes to preload
- Sodium and water retention in kidneys affects blood volume
- Clinical implication: diuretics and sodium restriction reduce preload
- Small arteries and arterioles are primary resistance vessels
- Vasoconstriction mediators: angiotensin II, norepinephrine, antidiuretic hormone, endothelin
- Management approach: vasodilators target these specific pathways
Key Mediators and Therapeutic Targets
1. Posterior pituitary and ADH:
- Vasopressin functions as vasoconstrictor
- Increases sodium and water retention
- Management implications: ADH antagonists (vaptans) in specific scenarios
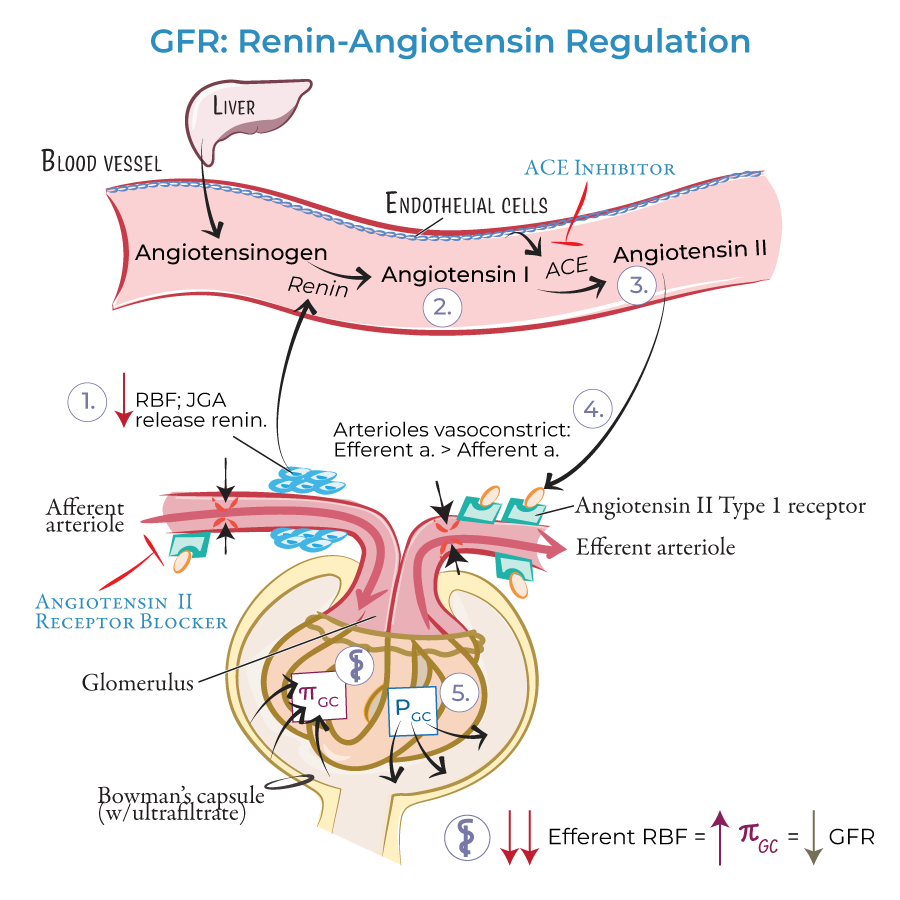
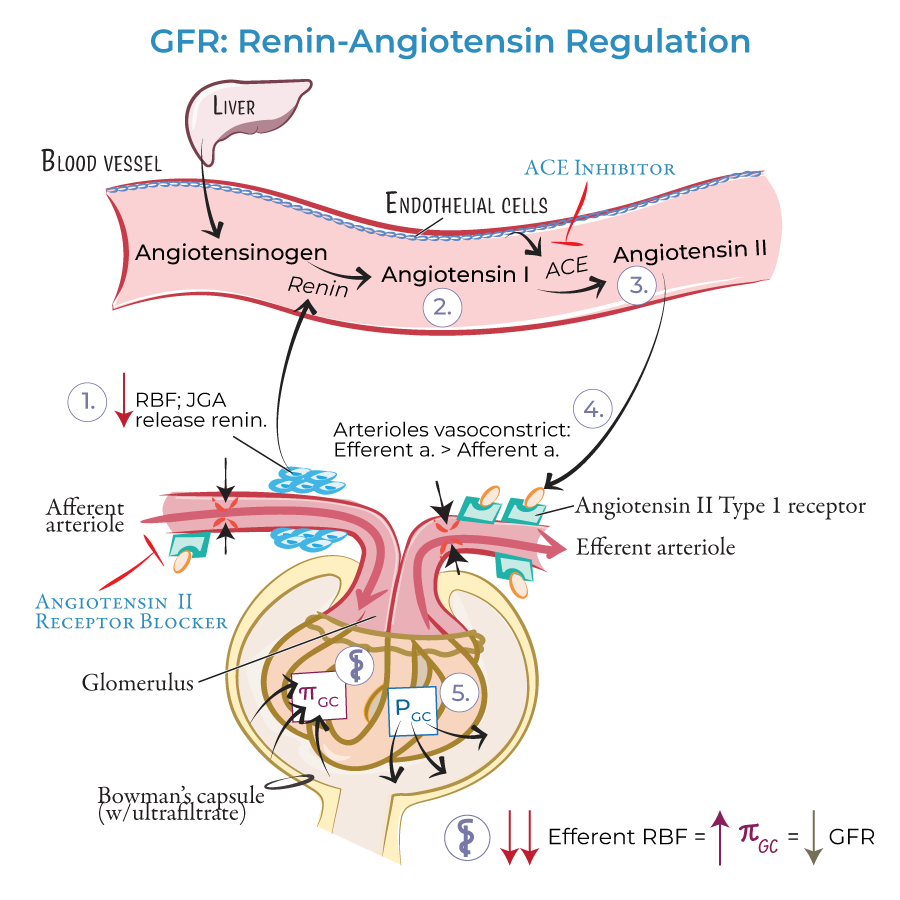
- Angiotensin II: direct vasoconstriction and sodium/water retention
- Indirect effects: stimulates norepinephrine, ADH, and aldosterone
- Multiple antihypertensive classes target this system: ACE inhibitors, ARBs, direct renin inhibitors
 3. Adrenal cortex and aldosterone:
3. Adrenal cortex and aldosterone:
- Similar effects to ADH on sodium/water retention
- Management target: mineralocorticoid receptor antagonists
- Increases heart rate, contractility, and vasoconstriction
- Management targets: beta-blockers, alpha-blockers
Hypertensive Crisis: Assessment and Management
1. Classification and differentiation:
- Hypertensive urgency: BP >180/120 mmHg without end-organ damage
- Hypertensive emergency: BP >180/120 mmHg with end-organ damage
- Management differs based on this critical distinction
- Severe headache, confusion, impaired vision
- Chest pain, shortness of breath
- Nausea/vomiting, anxiety, seizures
- These symptoms suggest end-organ damage requiring immediate intervention
- --
HIGH YIELD
Clinical Applications of Vasodilation Mechanisms
1. Endogenous vasodilators:
- Nitric oxide, prostaglandins, histamine, bradykinin
- Therapeutic implications: medications that enhance these pathways
- Bradykinin is broken down by angiotensin II, contributing to ACE inhibitor effects
- ACE inhibitors reduce angiotensin II and increase bradykinin
- This dual effect explains both efficacy and side effects (cough, angioedema)
- Understanding explains why ARBs have similar efficacy without bradykinin-related side effects
- Chronic hypertension leads to structural changes
- Altered balance of endothelin (increased) and nitric oxide (decreased)
- Therapeutic challenge: may require multiple agents and longer treatment course
Clinical Assessment of Hypertension Mechanisms
1. Salt sensitivity evaluation:
- Some patients develop hypertension due to sodium retention
- Clinical approach: trial of sodium restriction and diuretic therapy
- Response indicates underlying pathophysiology
- Presents with elevated blood volume and preload
- Clinical indicators: hypokalemia, metabolic alkalosis
- Diagnostic approach: aldosterone-renin ratio measurement
- Multiple factors affect various components of blood pressure regulation
- Family history assessment is crucial
- Tailored approach based on identified factors
- --
Beyond the Tutorial
Advanced Clinical Management
1. Comprehensive treatment approach:
- Initial evaluation of predominant mechanism (volume vs. resistance)
- Stepwise medication selection based on underlying pathophysiology
- Monitoring parameters beyond blood pressure (electrolytes, renal function)
- Systematic evaluation for secondary causes
- Medication adherence assessment
- Consideration of interfering substances (NSAIDs, stimulants)
- Therapeutic drug monitoring when appropriate
- Pregnancy: risk-benefit considerations, safe medication selection
- Elderly: focus on systolic hypertension, risk of orthostatic hypotension
- Comorbidities: diabetes, CKD, heart failure - tailored approaches
Practice-Based Learning
1. Implementation of clinical guidelines:
- Evidence-based target selection for different populations
- Risk stratification approaches
- Quality measures and performance improvement
- Team-based care models for hypertension management
- Care coordination for complex patients
- Population health approaches to blood pressure control
- Electronic health record tools for hypertension management
- Remote monitoring integration
- Adherence support strategies
