USMLE/COMLEX 3 - H. pylori Infection
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 3 & COMLEX-USA Level 3 from the Helicobacter pylori tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards.
 Below is information not explicitly contained within the tutorial but important for USMLE & COMLEX-USA Level 3.
Below is information not explicitly contained within the tutorial but important for USMLE & COMLEX-USA Level 3.
- --
VITAL FOR USMLE/COMLEX 3
Clinical Management of H. pylori Infection
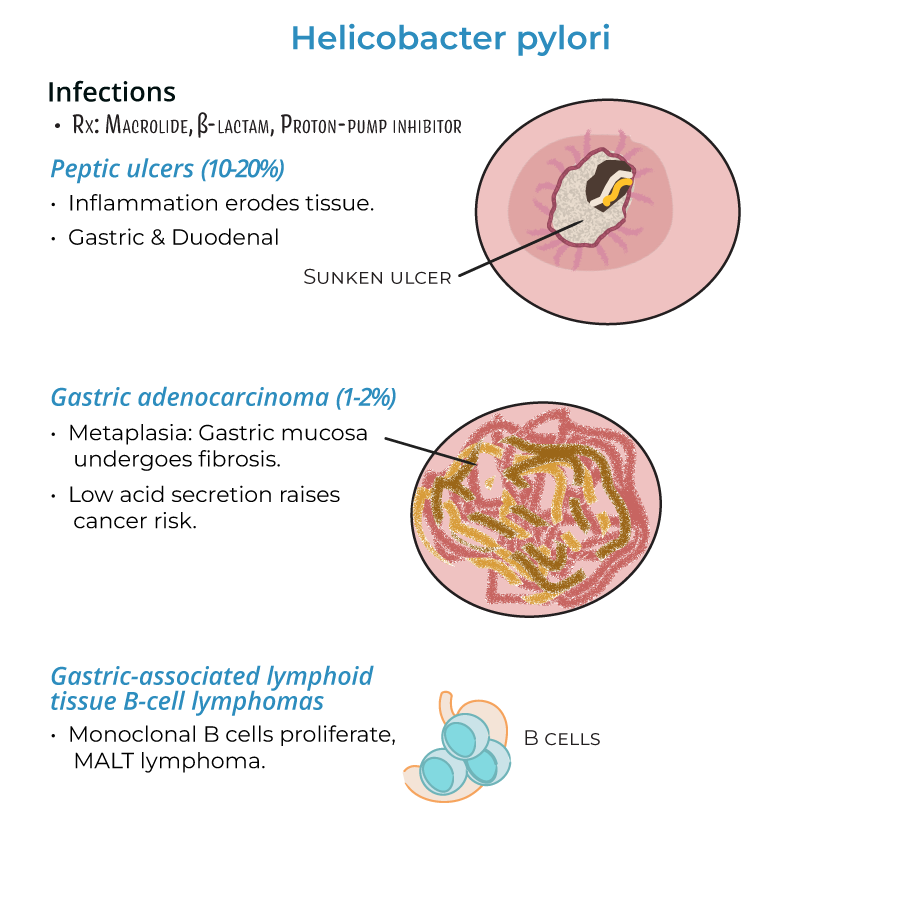
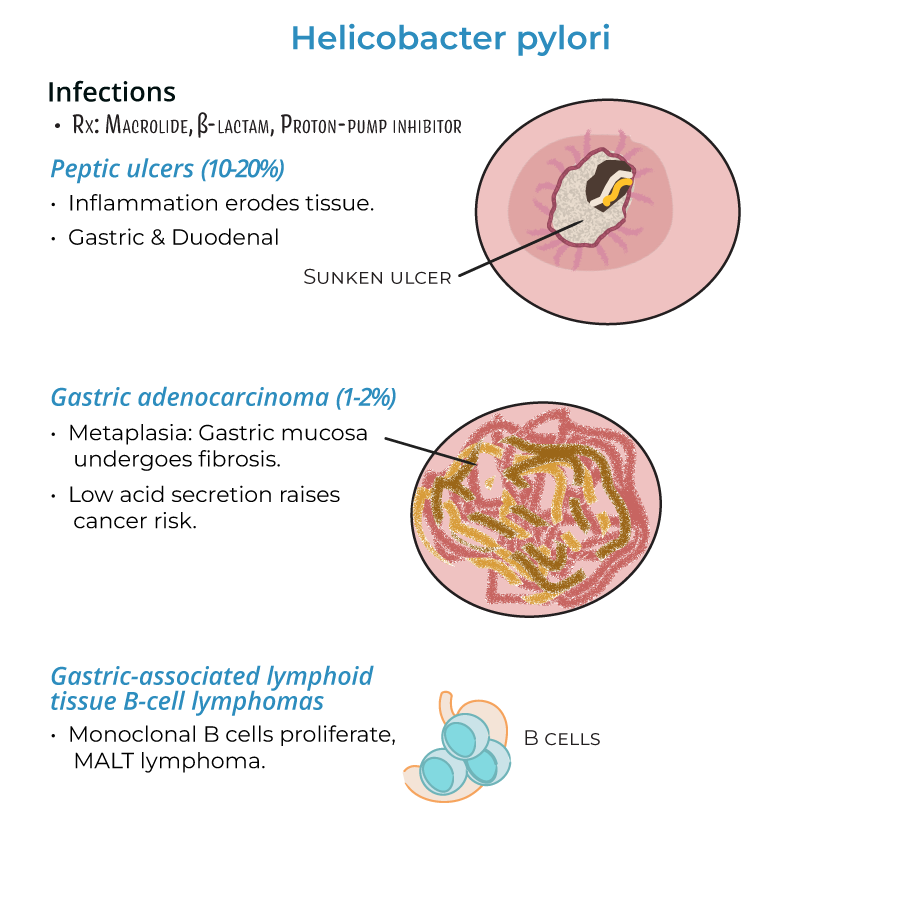
1. Treatment regimens include macrolides, beta-lactams, and proton-pump inhibitors.
2. Treatment is important because chronic gastritis can lead to severe consequences.
3. Chronic infection requires eradication therapy to prevent progression to serious complications.
Complications and Risk Assessment
1. Peptic ulcers develop in 10-20% of patients with gastritis, requiring prompt treatment.
2. Gastric adenocarcinoma occurs in 1-2% of chronic infections, making risk assessment critical.
3. MALT lymphomas develop when monoclonal B cells proliferate in response to infection.
4. Inflammation patterns predict complication risk: antral gastritis associates with duodenal ulcers while pangastritis increases gastric cancer risk.
Pathogenesis Relevant to Management
1. Virulence factors like CagA and VacA influence disease severity and treatment outcomes.
2. Type IV secretion systems that inject CagA into host cells are associated with more severe disease.
3. H. pylori destroys mucosa, allowing acids and toxins access to deeper tissues, leading to bleeding, perforation, and metaplasia.
Special Patient Populations
1. Enterohepatic helicobacters (H. cinaedi and H. fennelliae) cause gastroenteritis and bacteremia in immunocompromised individuals.
2. Consider H. pylori testing in patients with unexplained dyspepsia, NSAID use, or family history of gastric cancer.
- --
HIGH YIELD
Disease Progression and Monitoring
1. Gastritis can progress from acute phase (nausea, bloating, vomiting) to chronic inflammation.
2. Chronic inflammation leads to metaplasia where gastric mucosa is replaced by fibrotic tissue that can become neoplastic.
3. Reduced gastric acid secretion is associated with higher risk of adenocarcinoma, requiring monitoring.
4. Patients with persistent symptoms after treatment warrant follow-up testing for eradication.
Treatment Considerations
1. Standard treatments target both the bacteria and the acidic environment that damages tissues.
2. Bacterial resistance mechanisms (including production of superoxide dismutase and catalase) can affect treatment efficacy.
3. Treatment regimens must account for regional resistance patterns.
4. Treatment failure requires alternative antibiotic combinations.
Clinical Decision Making
1. Localized gastritis typically causes increased acid production and duodenal ulcers, guiding therapy choices.
2. Widespread inflammation (pangastritis) associates with atrophy, reduced acid, and cancer risk, requiring surveillance.
3. Symptomatic patients with risk factors for complications need more aggressive management.
4. Family screening may be warranted in patients with MALT lymphoma or gastric cancer.
Diagnostic Approach
1. Diagnosis relies on tests detecting urease activity (H. pylori is urease positive).
2. Endoscopic evaluation allows assessment of inflammation patterns and complications.
3. Post-treatment testing confirms eradication, especially in high-risk patients.
4. Antimicrobial susceptibility testing guides therapy in treatment failures.
- --
Beyond the Tutorial
Advanced Treatment Strategies
1. Sequential therapy: amoxicillin + PPI followed by clarithromycin + metronidazole + PPI.
2. Concomitant therapy: PPI + amoxicillin + clarithromycin + metronidazole simultaneously.
3. Bismuth quadruple therapy for areas with high clarithromycin resistance.
4. Antibiotic susceptibility-guided therapy for multiple treatment failures.
5. Evaluation of compliance and adherence in treatment failures.
Long-term Management
1. Post-eradication surveillance for patients with pre-neoplastic lesions.
2. Endoscopic surveillance schedule based on risk stratification.
3. Management of refractory MALT lymphoma not responding to H. pylori eradication.
4. Screening and prevention strategies for high-risk families.
5. Nutritional counseling for patients with atrophic gastritis.
Special Clinical Scenarios
1. Management of H. pylori in patients requiring chronic NSAID or anticoagulant therapy.
2. Approach to the patient with recurrent dyspepsia after successful eradication.
3. Management of extraintestinal manifestations associated with H. pylori.
4. Considerations in elderly and multimorbid patients.
5. Decision algorithms for dyspepsia management in resource-limited settings.
Emerging Approaches
1. Vaccine development status and potential prevention strategies.
2. Novel diagnostic technologies including molecular testing for resistance.
3. Microbiome-based approaches to H. pylori management.
4. Role of probiotics as adjunctive therapy.
5. Impact of H. pylori eradication on healthcare systems and antibiotic stewardship.
