USMLE/COMLEX 3 - Endocarditis
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 3 & COMLEX-USA Level 3 from the Endocarditis tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
- --
VITAL FOR USMLE/COMLEX 3
Clinical Assessment & Diagnosis
1. Acute endocarditis presents with fever, chills, and other flu-like symptoms.
2. Vegetation complications include tissue invasion/destruction and emboli formation leading to stroke, organ failure, and sepsis.
3. Blood culture patterns:
- Infective endocarditis: Most commonly caused by gram-positive bacteria (Staphylococcus aureus, Viridans streptococci, Enterococci)
- Culture-negative endocarditis: Consider Coxiella burnetii, Brucella species, and Tropheryma whipplei
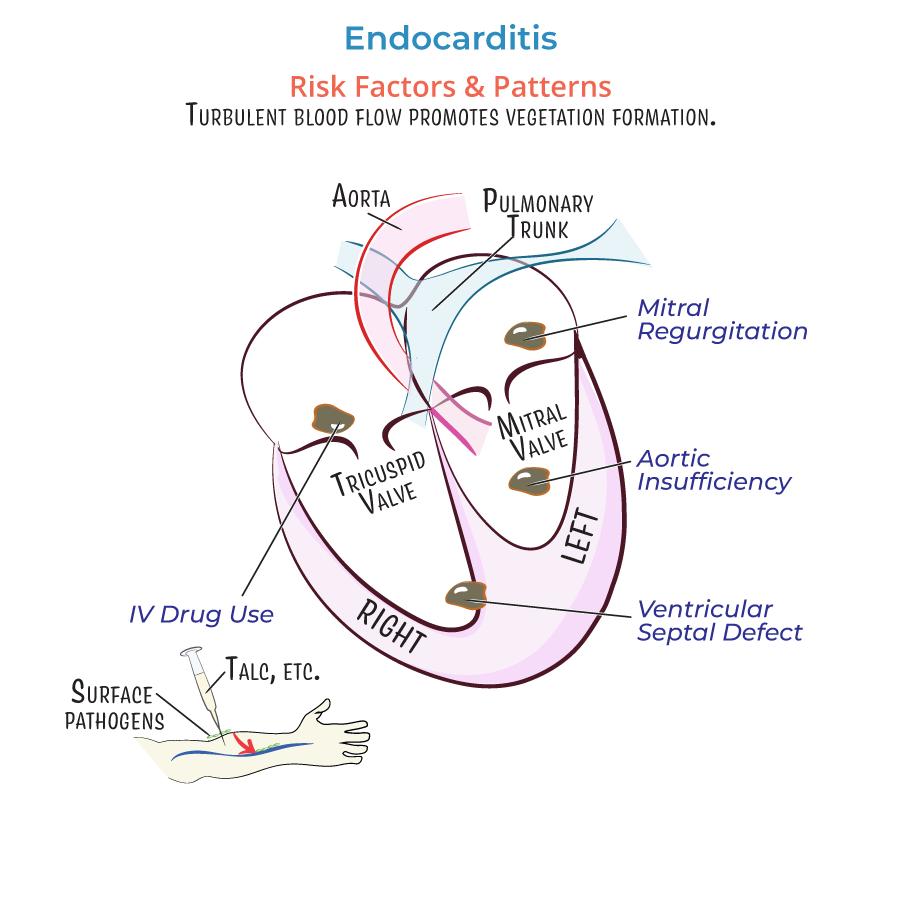
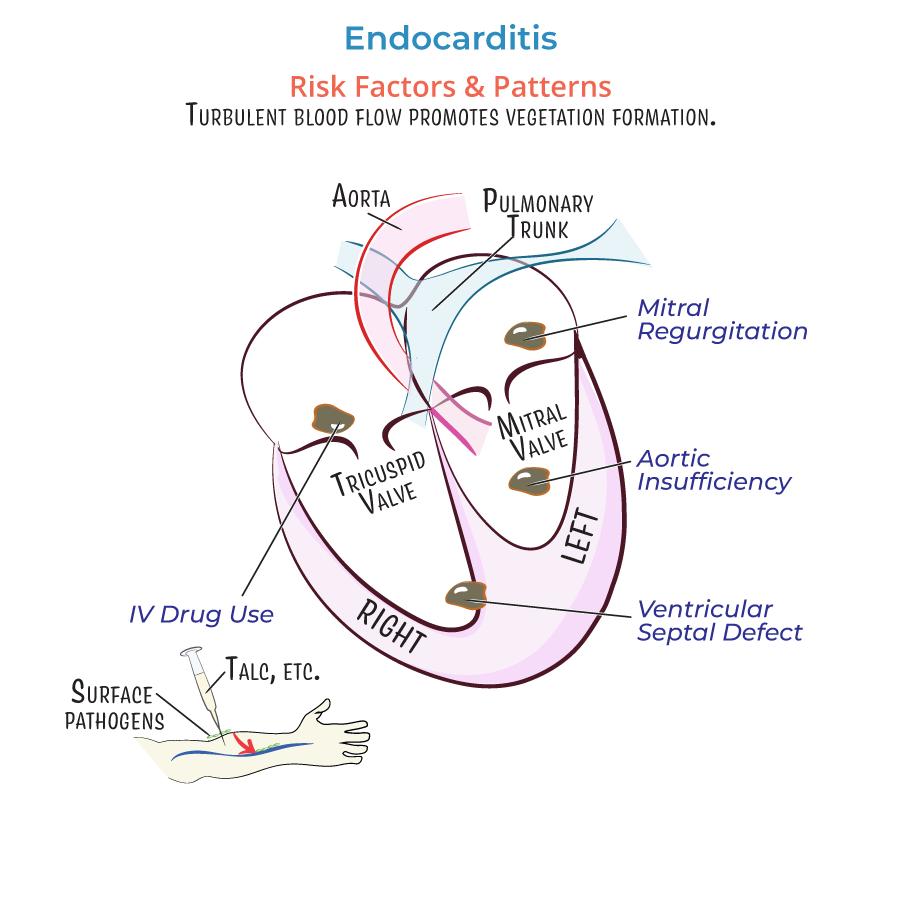
High-Risk Populations
1. IV drug users:
- Risk of right-sided valvular endocarditis
- Introduction of particulate matter (talc), skin pathogens, or oral flora (if saliva used on needles)
- Higher infection susceptibility (bacteria adhere to prosthetic materials)
- Common pathogens: Staphylococcus aureus and Coagulase-negative Staphylococci
- Invasive vegetations can form at prosthetic-tissue junction
- Often requires surgical valve replacement
Complication Assessment
1. Embolic events more common with:
- Libman-Sacks endocarditis (SLE): Loosely attached vegetations increase embolism risk
- Large mobile vegetations that can break free
- --
HIGH YIELD
Management Considerations by Valve & Condition
1. Mitral valve regurgitation: Monitor for vegetations on atrial leaflet surface.
2. Aortic insufficiency: Watch for vegetations on ventricular side.
3. Ventricular septal defects: Assess for right-sided vegetations near the orifice.
4. Prosthetic valve endocarditis:
- Evaluate annular ring-tissue junction for invasive vegetations
- Assessment for valvular deformation
- Higher likelihood of requiring surgical intervention
Pathogen-Specific Considerations
1. Gram-positive bacteria: Primary targets for empiric therapy in suspected cases.
2. Gram-negative bacteria (including HACEK group): Consider in culture-negative cases.
3. Fungal endocarditis (Candida, Aspergillus): Higher mortality; often requires combined medical and surgical approaches.
4. Libman-Sacks endocarditis:
- Associated with Systemic Lupus Erythematosus
- May require anticoagulation management
- Less inflammation but higher embolism risk
Special Clinical Scenarios
1. Endocarditis following catheter procedures or device implantation:
- Initial inflammation from catheter-induced abrasion
- Endothelial damage promoting fibronectin deposition and vegetation formation
- Small vegetations typically near edge of leaflet
- Different management approach than infectious endocarditis
- --
Beyond the Tutorial
Comprehensive Management Approach
1. Antimicrobial therapy:
- Empiric therapy based on likely pathogens and local resistance patterns
- Targeted therapy after culture results (4-6 weeks for native valves, 6+ weeks for prosthetic)
- Monitoring for therapeutic efficacy and drug levels
- Heart failure from valvular dysfunction
- Perivalvular extension with abscess formation
- Persistent bacteremia despite appropriate antibiotics
- Large vegetations with embolic potential
- Fungal endocarditis
- Early prosthetic valve endocarditis (<12 months post-implantation)
- Embolic events: Anticoagulation considerations
- Heart failure: Medical optimization before surgery
- Stroke management: Timing of anticoagulation and surgical intervention
- Renal dysfunction: Antibiotic dose adjustments
- IV drug users: Addiction services referral, consideration of valve replacement versus repair
- Elderly patients: Balancing surgical risk with benefit
- Immunocompromised hosts: Broader antimicrobial coverage, lower threshold for surgical intervention
- Serial echocardiography
- Blood culture monitoring
- Long-term antibiotic suppression in select cases
- Recurrence prevention strategies
- Endocarditis prophylaxis education for high-risk patients
