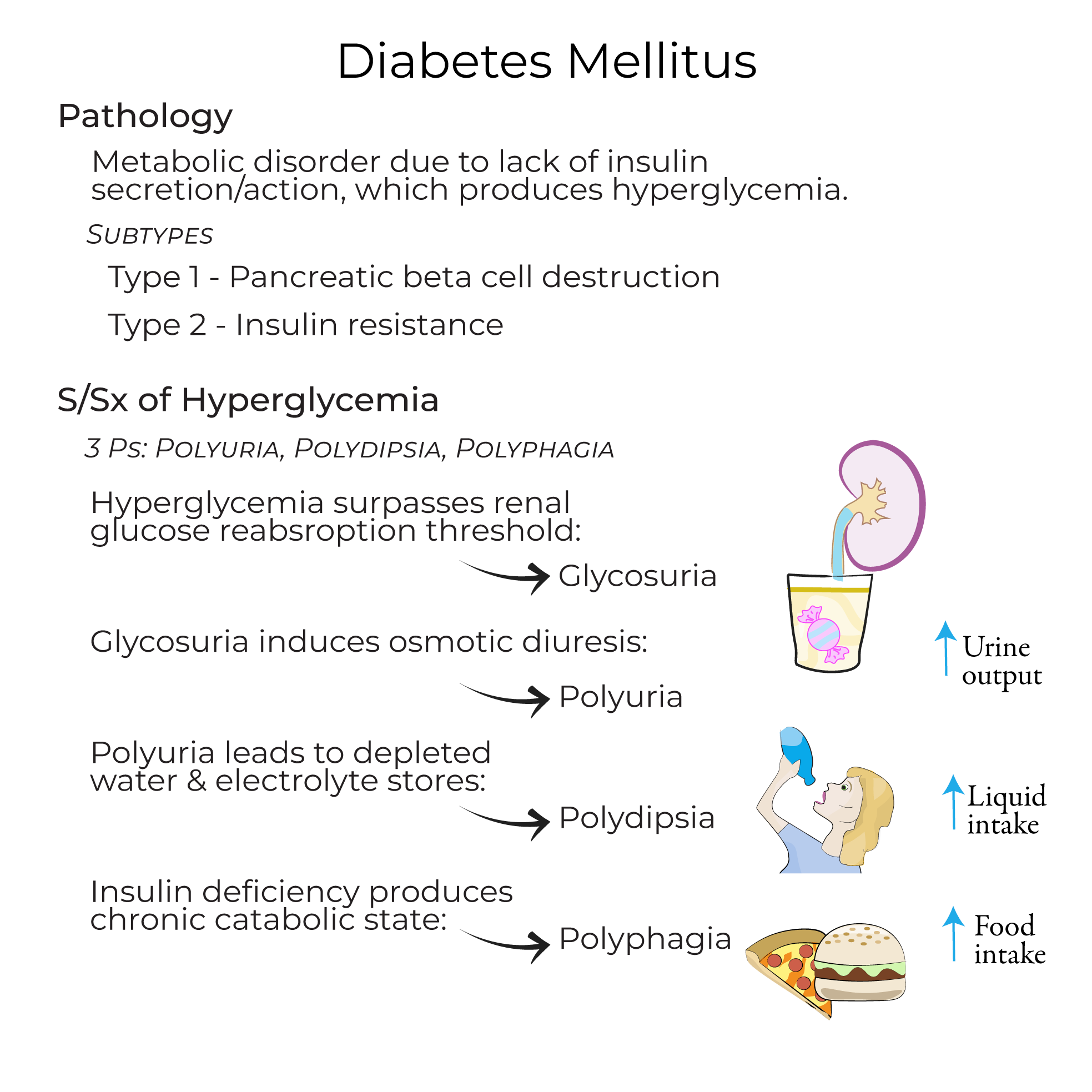
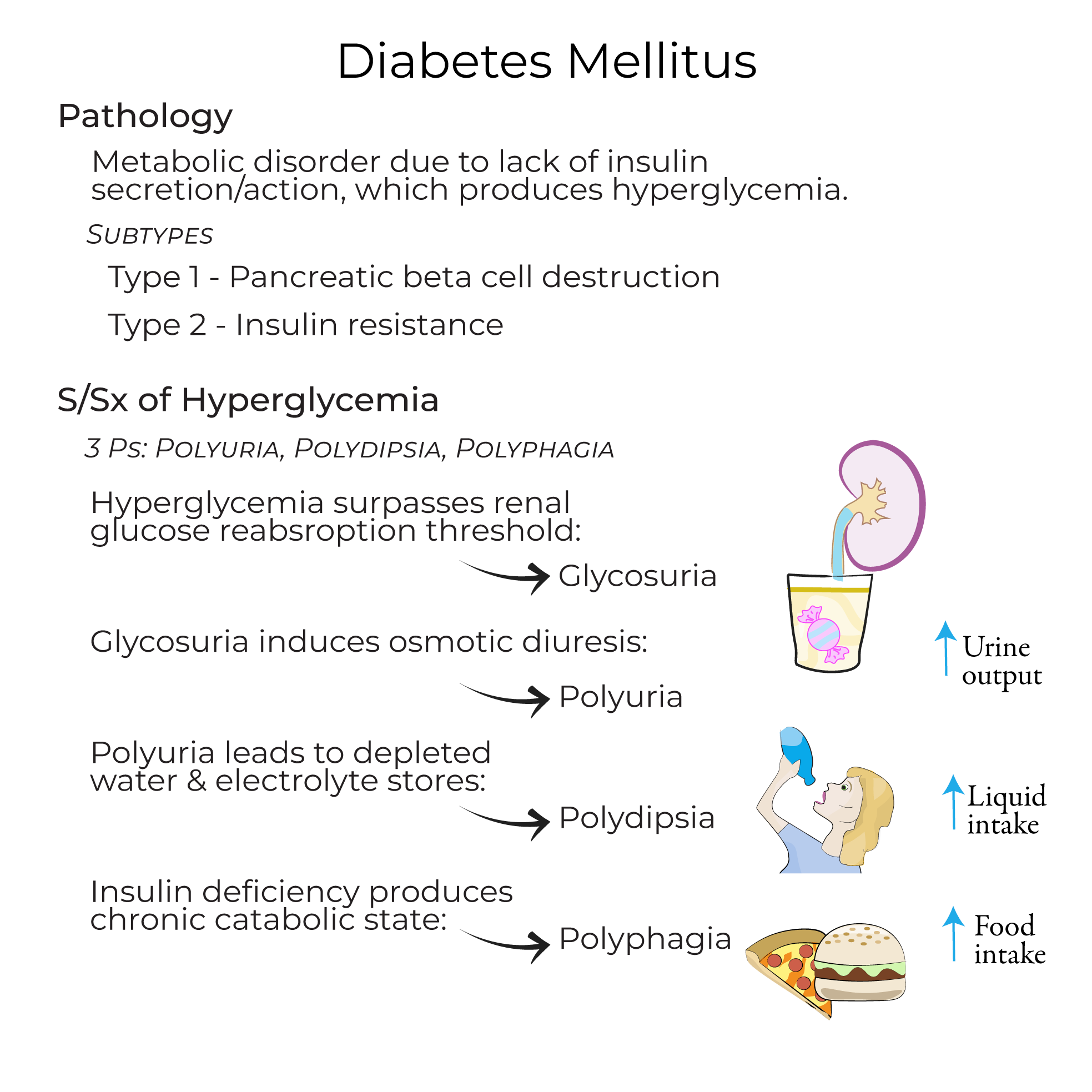
USMLE/COMLEX 3 - Diabetes Mellitus Pathophysiology
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 3 & COMLEX-USA Level 3 from the Diabetes Mellitus - Pathophysiology tutorial, as well as points of interest that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
 Below is information not explicitly contained within the tutorial but important for USMLE & COMLEX 3.
Below is information not explicitly contained within the tutorial but important for USMLE & COMLEX 3.
- --
VITAL FOR USMLE/COMLEX 3
Diabetes Mellitus - Management Principles
1. Diagnostic approach: Utilize random plasma glucose level of 200+ mg/dL or a fasting plasma glucose level of 126+ mg/dL for diagnosis.
2. Clinical goal: Prevent end-organ damage to heart, kidneys, eyes, and peripheral nervous system from chronic hyperglycemia.
3. Type 1 Diabetes management: Requires exogenous insulin administration due to absolute insulin deficiency.
4. Type 2 Diabetes management algorithm:
- First-line therapy: Diet and exercise, and perhaps administration of Metformin, which decreases hepatic glucose production
- Escalation options: Insulin, GLP-1 receptor agonists, or SGLT2-inhibitors if hyperglycemia persists
- Therapeutic goal: Reach glycemic targets to avoid organ damage caused by hyperglycemia
Acute Complications - Recognition and Management
1. Diabetic Ketoacidosis (DKA):
- Population association: Occurs in under-treated Type 1 diabetes
- Clinical presentation: Nausea and vomiting, fatigue, "fruity" odor, and Kussmal breathing (deep, rapid breathing pattern)
- Pathophysiology: Reflects the acidic state of the body, which can ultimately lead to coma
- Management protocol: Administer fluids, electrolytes, and insulin to normalize blood glucose
- Population association: More common in Type 2 diabetes
- Pathophysiology: Occurs when a patient with polyuria has deficient water intake leading to severe dehydration
- High-risk population: Patients unable to drink on their own, such as after a stroke or other debilitating conditions
- Mortality risk: Has a mortality rate of up to 20% - much higher than diabetic ketoacidosis
- Treatment approach: Requires saline, insulin, and electrolytes
- Precipitating factors: Missing a meal, excessive physical exertion, or excessive insulin administration
- Clinical signs: Dizziness, sweating, palpitations, and tachycardia
- Immediate intervention: Treat with glucose to correct the blood sugar levels
- --
HIGH YIELD
Chronic Complication Management
1. Vascular disease prevention:
- Pathogenesis: Results from chronic hyperglycemia
- Macrovascular complications: Monitor and manage risk of heart failure and atherosclerosis (which can produce myocardial infarction or stroke)
- Microvascular complications: Screen for and treat kidney damage, visual impairment, and peripheral nerve dysfunction
- Pediatric monitoring: Watch for impaired growth in children
- Infection prevention: Address increased susceptibility to infection due to immune suppression
Type 1 Diabetes - Clinical Decision Making
1. Diagnostic considerations: Be aware that some adults diagnosed with Type 2 diabetes based on age may be misclassified, which can have deleterious effects on their treatment
2. Clinical course monitoring: Hyperglycemia may be transient in some cases, with variable insulin needs, particularly in adults diagnosed with Type 1 diabetes
3. Variant awareness: Consider idiopathic Type 1 diabetes in differential diagnosis, where autoimmune response is not involved, though very rare
Type 2 Diabetes - Therapeutic Considerations
1. Lifestyle intervention rationale: Exercise increases the number of Glut-4 receptors in skeletal muscle, which is why it's commonly recommended for patients with insulin resistance
2. Medication selection factors:
- Cost considerations: Drugs can be costly for patients
- Contraindication assessment: Medications may have contraindications that must be considered for each patient
- Individualization emphasis: Treatment must be tailored to the individual and achievable glycemic targets
Prediabetes - Preventive Approach
1. Risk assessment: Pre-diabetic patients are at high risk for Type 2 diabetes and cardiovascular complications
2. Population prevalence: The CDC reports that 1 in 3 Americans is pre-diabetic
3. Prevention strategy: Advise patients to take preventive steps such as increasing physical activity and losing weight
- --
Beyond the Tutorial
Complex Clinical Decision Making
1. Individualized A1c targets: Risk-benefit assessment for tight versus relaxed glycemic control based on patient factors.
2. Diabetes medication de-escalation: Approaches to reducing polypharmacy in patients with improved glycemic control.
3. Post-bariatric surgery management: Adjusting diabetes medications after significant weight loss.
Advanced Management Approaches
1. Integrated diabetes care models: Evidence for team-based approaches including endocrinologists, primary care, diabetes educators, and pharmacists.
2. Telehealth in diabetes management: Implementation strategies and outcomes data.
3. Social determinants of health: Addressing barriers to diabetes care including food insecurity, housing instability, and health literacy.
Complex Complication Management
1. Diabetic kidney disease progression: Decision-making around RAS blockade, SGLT2 inhibition, and GLP-1 RAs for nephroprotection.
2. Painful diabetic neuropathy: Evidence-based approaches to symptomatic management.
3. Diabetic cardiomyopathy: Recognition and management distinct from ischemic heart disease.
Special Clinical Scenarios
1. Perioperative management: Protocols for managing diabetes medications around surgery.
2. Critical illness: Glycemic targets and insulin protocols in ICU settings.
3. Steroid-induced hyperglycemia: Management approaches for patients requiring glucocorticoid therapy.
