USMLE/COMLEX 3 - Bacterial Endocarditis
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 3 & COMLEX-USA Level 3 from the Bacterial Endocarditis tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards.
 Below is information not explicitly contained within the tutorial but important for USMLE Step 3 & COMLEX-USA Level 3.
Below is information not explicitly contained within the tutorial but important for USMLE Step 3 & COMLEX-USA Level 3.
- --
VITAL FOR USMLE/COMLEX 3
Clinical Management Priorities
1. S. aureus endocarditis requires prolonged intravenous administration of antibiotics; S. aureus is resistant to penicillin.
2. For methicillin-resistant strains (MRSA), vancomycin or daptomycin, sometimes in combination with other antibiotics, are administered intravenously.
3. High-risk populations requiring aggressive management include individuals with compromised immune systems and/or prosthetic cardiac devices.
Antimicrobial Resistance Considerations
1. Methicillin-resistant strains (MRSA) display changes in their penicillin-binding proteins to increase tolerance.
2. MRSA is increasingly common in both hospital and community settings, requiring careful antibiotic selection.
3. S. aureus produces a protective biofilm (slime layer) comprising polysaccharides and proteins that inhibit thrombus destruction and antibiotic penetration.
Complications Management
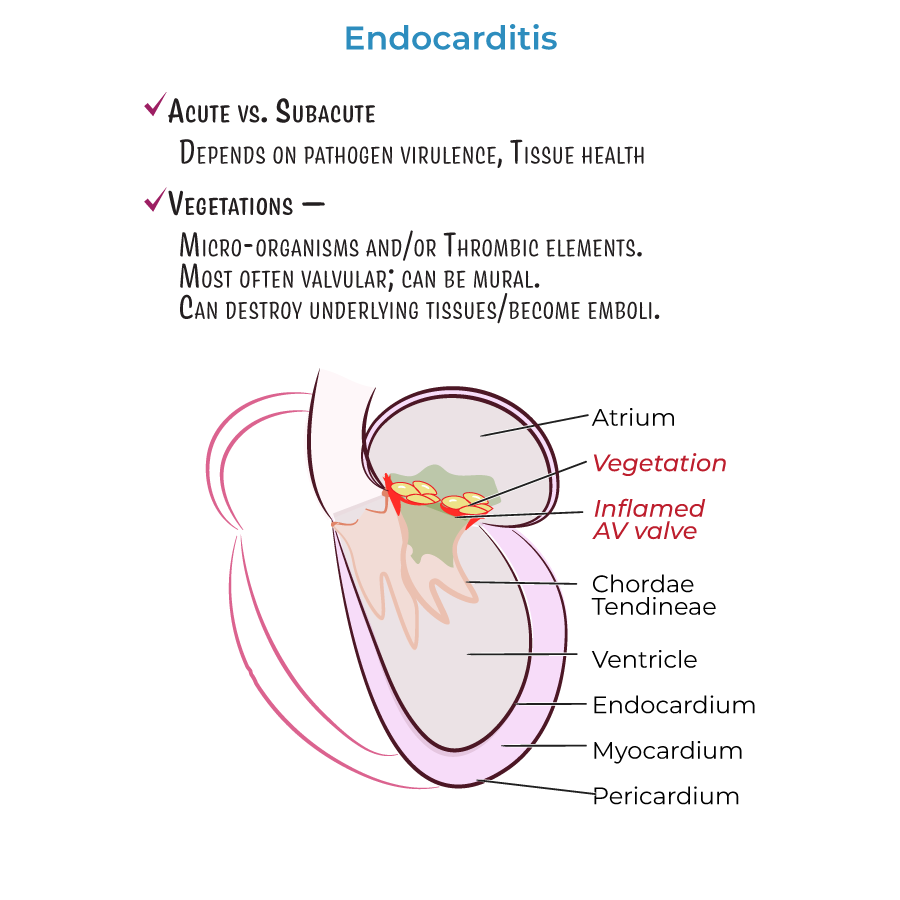
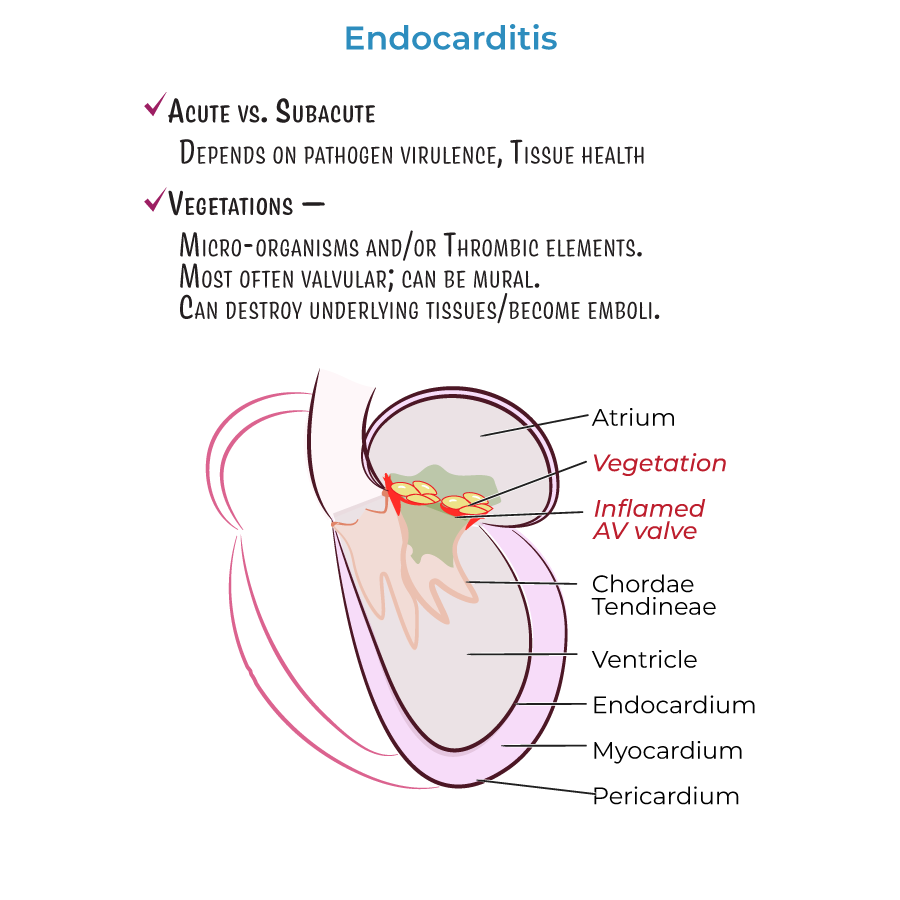
1. If vegetation breaks free from the valve and travels in the bloodstream, it can become lodged in a vessel and cause embolism, even stroke.
2. S. aureus can lie dormant within host tissues as small colony variants, evading host defenses and antibiotics, only to reemerge later.
3. Endocarditis can affect the atrioventricular valve or walls of the heart (mural endocarditis), requiring different management approaches.
Prevention Strategies
1. S. aureus exists in the normal human flora, commonly found in the nares (nostrils), which can be a source for preventative measures.
2. Patients with prosthetic cardiac devices require specialized prevention protocols.
3. The aggressive nature of S. aureus necessitates rapid identification and treatment to prevent complications.
- --
HIGH YIELD
Treatment Decision Making
1. S. aureus endocarditis has a high mortality rate due to its aggressive nature and antibiotic resistance.
2. Prolonged IV antibiotic therapy must be tailored to overcome bacterial evasion mechanisms.
3. Treatment must address the intracellular location of bacteria, as S. aureus can enter host cells through endocytosis.
4. Antibiotic selection must consider the ability to penetrate biofilms and reach intracellular bacteria.
Evidence-Based Approach to Therapy
1. Methicillin, a synthetic derivative of penicillin, has been used to treat S. aureus infections since the 1960s.
2. S. aureus employs phenotypic switching to become small colony variants that can evade antibiotics.
3. Combination therapy may be necessary to address multiple virulence mechanisms.
4. Treatment must continue long enough to eradicate dormant bacteria that may reemerge.
Monitoring and Follow-up
1. Within host cells, S. aureus releases toxins and acts as a superantigen, requiring monitoring for systemic inflammatory responses.
2. Platelet activation by S. aureus induces pro-inflammatory and pro-coagulation molecules, necessitating monitoring for thrombotic complications.
3. The risk of embolism remains high during treatment as vegetations may dislodge.
4. Regular assessment for treatment response is critical due to S. aureus ability to "hide" from the host immune system and antibiotic treatments.
Systems-Based Considerations
1. Adherence to endothelial cells via surface adhesion proteins requires prolonged therapy to eradicate.
2. Invasion of endocardial cells releasing toxins promotes inflammatory processes that destroy host tissues, requiring anti-inflammatory consideration.
3. Fibronectin and fibrinogen act as "connecting bridges" to form thrombotic vegetation, potentially requiring anticoagulation management.
4. Thrombus formation promotes additional platelet activation, creating a cycle that must be interrupted by comprehensive treatment.
- --
Beyond the Tutorial
Advanced Management Considerations
1. Multidisciplinary approach involving infectious disease specialists, cardiologists, and cardiac surgeons is essential for complicated cases.
2. Point-of-care ultrasound can provide bedside evaluation of vegetation size and valvular function to guide urgent management decisions.
3. Pharmacokinetic/pharmacodynamic principles should guide antibiotic dosing, with consideration of drug penetration into vegetations and biofilms.
Evidence-Based Protocols
1. Timing of surgery in S. aureus endocarditis remains controversial; early surgical intervention may be beneficial in select high-risk patients.
2. Outpatient parenteral antibiotic therapy (OPAT) can be considered for stable patients after initial hospitalization, with careful patient selection.
3. Newer antibiotics like dalbavancin and oritavancin with extended half-lives may allow for simplified dosing regimens in select patients.
Systems-Based Practice
1. Transition of care from inpatient to outpatient settings requires careful coordination to ensure completion of prolonged antibiotic courses.
2. Quality measures related to S. aureus bacteremia include echocardiography performance, follow-up blood cultures, and appropriate duration of therapy.
3. Antimicrobial stewardship programs should guide appropriate empiric therapy while balancing concerns of resistance development.
