USMLE/COMLEX 3 - Aortic Aneurysm & Dissection
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 3 & COMLEX-USA Level 3 from the Aortic Aneurysm & Dissection, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.

- --
VITAL FOR USMLE/COMLEX 3
Aortic Aneurysm
1. AAA rupture presents with hypotension, abdominal or back pain, and requires immediate surgical intervention.
2. One-time screening ultrasound is recommended for men aged 65–75 who have ever smoked.
3. Elective repair of AAA is indicated if ≥5.5 cm in diameter or rapidly enlarging.
4. Symptomatic AAA, regardless of size, requires urgent surgery.
5. Manage asymptomatic small AAA (<5.5 cm) with periodic ultrasound surveillance and smoking cessation counseling.

Thoracic Aortic Aneurysm
6. Repair thoracic aneurysms when size ≥5.5 cm or faster than expected expansion; in Marfan or Ehlers-Danlos syndrome, intervene at ≥5.0 cm.
7. CT angiography is preferred imaging for diagnosis in stable patients.
8. Thoracic aneurysms can cause compressive symptoms (e.g., hoarseness, dysphagia, cough).
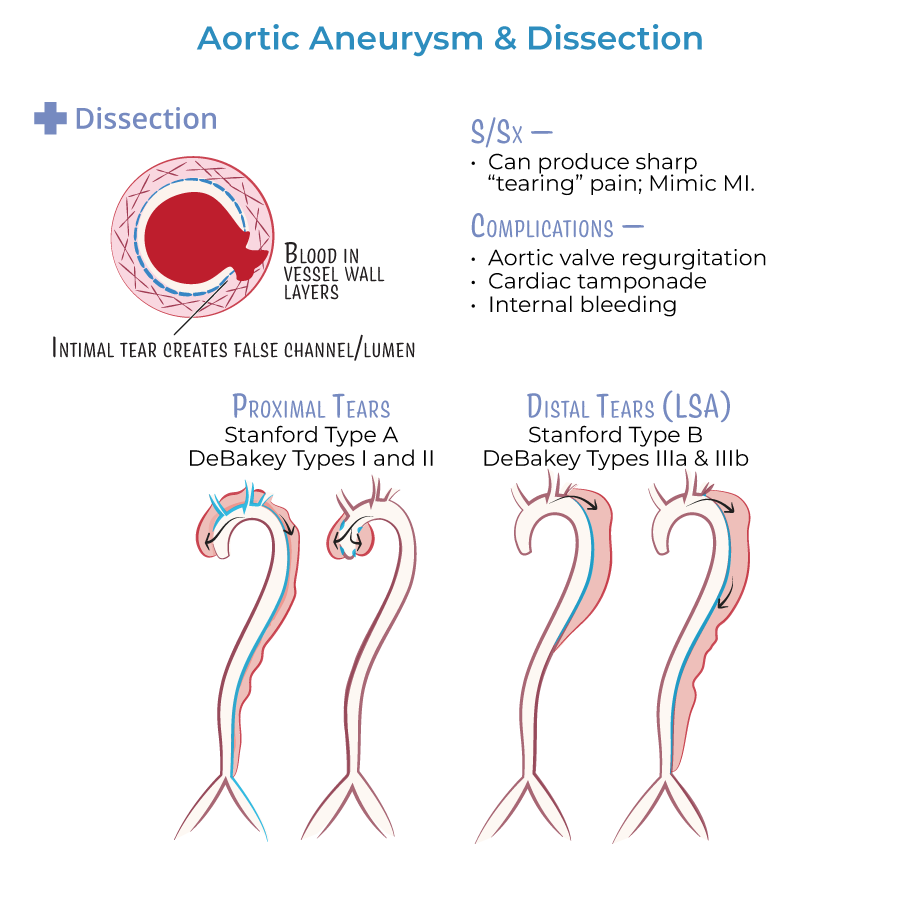
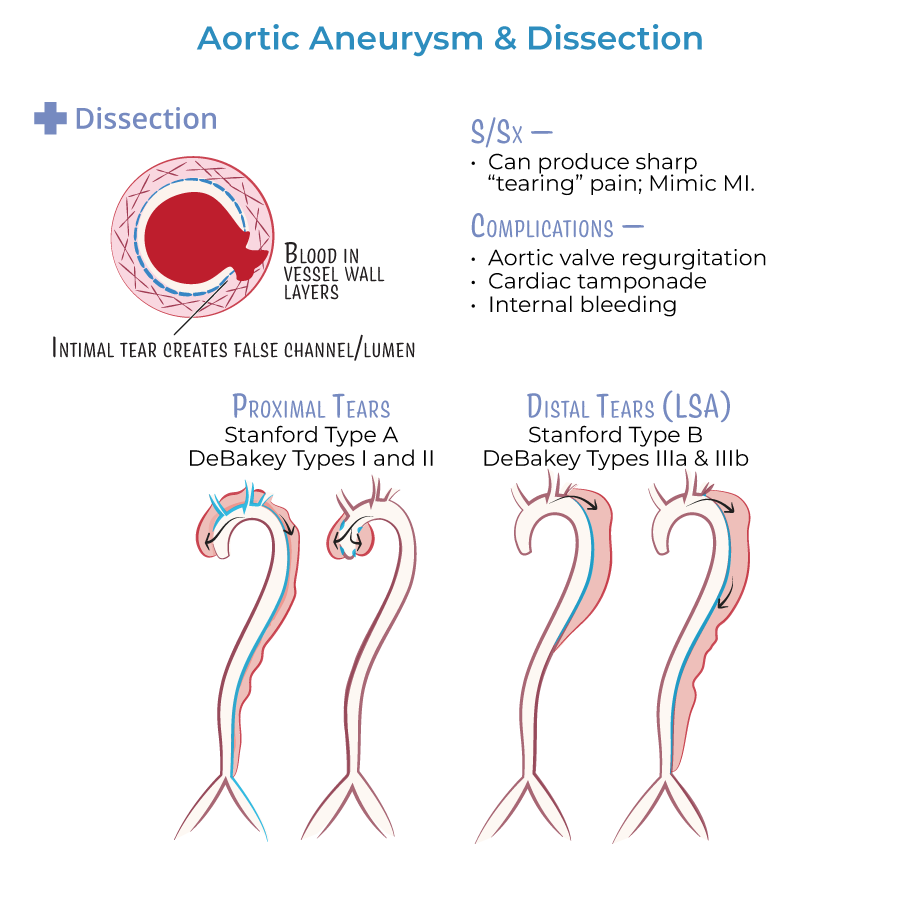
Aortic Dissection
9. Stanford Type A dissection (ascending aorta) is a surgical emergency, even if patient is initially stable.
10. Stanford Type B dissection (descending aorta) is treated medically first, unless there are complications (malperfusion, rupture, persistent pain).
11. Initial management of dissection involves IV beta-blocker (e.g., esmolol) to reduce heart rate and shear stress.
12. Goal heart rate is 60 beats per minute, and systolic BP 100-120 mmHg after beta-blocker initiation.
13. Add IV vasodilator (e.g., nitroprusside) only if blood pressure remains elevated after beta-blockade.
- --
HIGH YIELD
Etiology and Risk Factors
1. Hypertension is the leading risk factor for aortic dissection.
2. Smoking is the most important modifiable risk factor for abdominal aortic aneurysm.
3. Marfan syndrome and Loeys-Dietz syndrome predispose to thoracic aneurysms and early dissections.
Presentation
4. Aortic dissection presents with sudden severe tearing chest or back pain.
5. Pulse deficits, asymmetric blood pressures, or neurologic deficits suggest dissection.
6. Aortic regurgitation may occur in Type A dissections, presenting with a new diastolic murmur and acute heart failure.
7. Hoarseness or dysphagia suggest thoracic aneurysm pressing on adjacent structures.
8. Aneurysm rupture typically presents with hypovolemic shock, sudden pain, and syncope.
Diagnostic Approach
9. CT angiography is first-line imaging for stable patients.
10. Transesophageal echocardiography (TEE) is first-line in unstable patients or those too sick for CT.
11. MRI angiography can be used if contrast is contraindicated, but is less practical acutely.
Pharmacologic Management
12. Start beta-blockers first to control heart rate, preventing extension of the dissection.
13. Vasodilators (e.g., nitroprusside) are used second-line if systolic blood pressure remains elevated.
Complications
14. Dissection can cause cardiac tamponade, aortic regurgitation, stroke, renal failure, and bowel ischemia.
15. AAA rupture has a very high mortality rate if not immediately corrected surgically.
- --
Beyond the Tutorial
Advanced Management and Prognostic Points
1. Patients with Type A dissection need emergency cardiothoracic surgery consultation immediately after initial stabilization.
2. In Type B dissection, surgery is only indicated if there is malperfusion, aneurysmal expansion, refractory pain, rupture, or hypertension unresponsive to medication.
3. After Type A repair, monitor for pericardial effusion, pseudoaneurysm formation, or re-dissection.
4. Long-term management includes strict blood pressure control with beta-blockers and lifestyle modification.
5. In patients post-aortic repair, lifelong imaging surveillance is required (CT or MRI at scheduled intervals).
6. Avoid fluoroquinolone antibiotics in patients with known aneurysms due to increased risk of rupture.
Clinical Integration for Step 3
7. In patients with syncope, sudden severe chest pain, and unequal pulses, immediately rule out aortic dissection before attributing symptoms to myocardial infarction.
8. Pain migration (e.g., from chest to abdomen) suggests propagation of aortic dissection.
9. Multisystem involvement (neurologic, cardiac, renal) points strongly to dissection, especially in hypertensive older adults.
