Interstitial Lung Diseases for USMLE Step 2
Start your One-Week Free Trial
Already subscribed? Log in »
Interstitial Lung Diseases for the USMLE Step 2 Exam
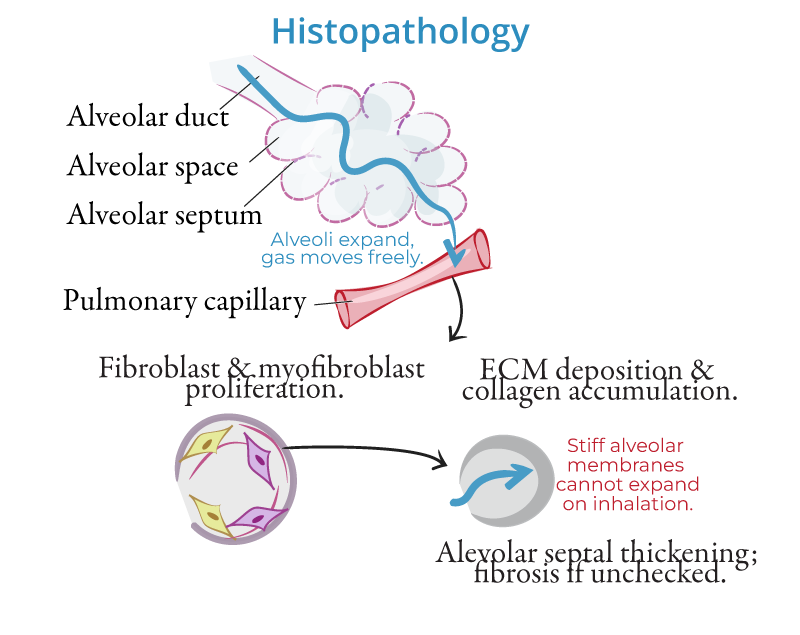
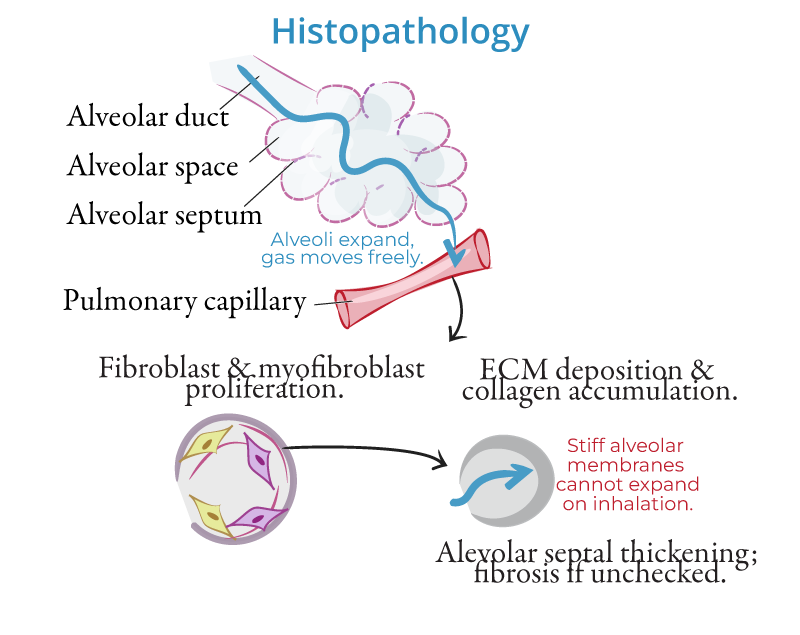
Pathophysiology
- Chronic Inflammation and Fibrosis:
- Interstitial lung diseases (ILDs) are a group of disorders characterized by inflammation and fibrosis of the lung interstitium, the tissue surrounding the alveoli. Repeated lung injury leads to abnormal wound healing, activation of fibroblasts, and excess deposition of collagen, resulting in scarring and stiffening of the lung tissue.
- Impaired Gas Exchange:
- Fibrosis thickens the alveolar walls, impairing gas exchange, reducing lung compliance, and leading to restrictive lung disease. Progressive fibrosis can lead to hypoxemia and respiratory failure.
- Mechanisms of Damage:
- Chronic inflammation, driven by immune responses, environmental toxins, or autoimmune diseases, triggers the fibrotic process. Persistent alveolar damage from inhaled toxins or immune dysregulation drives fibroblast activation, resulting in excessive collagen deposition.
Etiologies
- Idiopathic Pulmonary Fibrosis (IPF):
- A chronic, progressive form of ILD with no identifiable cause. IPF is characterized by a histologic pattern of usual interstitial pneumonia (UIP) and has a poor prognosis.
- Pneumoconioses:
- Occupational lung diseases caused by inhalation of inorganic dusts:
- Asbestosis: Caused by asbestos exposure.
- Silicosis: Due to inhalation of silica dust.
- Coal Workers' Pneumoconiosis: Results from long-term exposure to coal dust.
- Hypersensitivity Pneumonitis (HP):
- An immune-mediated disease caused by inhalation of organic antigens (e.g., bird feathers, mold). Repeated exposure leads to granulomatous inflammation and fibrosis.
- Sarcoidosis:
- A systemic granulomatous disease that commonly affects the lungs. Noncaseating granulomas form in the lungs, potentially leading to fibrosis if untreated.
- Connective Tissue Diseases:
- ILD can be secondary to systemic autoimmune diseases such as:
- Rheumatoid arthritis (RA): ILD occurs in a subset of patients with RA.
- Systemic sclerosis (scleroderma): Causes diffuse pulmonary fibrosis.
Clinical Features
- Dyspnea:
- Gradual onset of shortness of breath, worsening over time, particularly with exertion.
- Dry Cough:
- A persistent, nonproductive cough often accompanies dyspnea.
- Inspiratory Crackles:
- Fine, "velcro-like" crackles heard on auscultation, particularly in the lung bases.
- Clubbing:
- Finger clubbing is commonly seen in advanced cases of IPF and other fibrotic ILDs.
- Extrapulmonary Symptoms:
- In cases of connective tissue disease-associated ILD, systemic symptoms like joint pain and skin changes may be present.
Diagnosis
- High-Resolution CT (HRCT):
- The gold standard for diagnosing ILD. Findings may include:
- Honeycombing: Seen in IPF, indicating advanced fibrosis.
- Ground-glass opacities: Suggestive of inflammation, common in hypersensitivity pneumonitis and early fibrosis.
- Pulmonary Function Tests (PFTs):
- Reveal a restrictive pattern with reduced total lung capacity (TLC) and forced vital capacity (FVC). The diffusion capacity of carbon monoxide (DLCO) is typically decreased.
- Lung Biopsy:
- May be necessary for definitive diagnosis, particularly in cases where the cause of ILD is unclear.
Management
General Approach
- Smoking Cessation:
- Essential in patients with ILD to prevent further lung damage.
- Avoidance of Triggers:
- In hypersensitivity pneumonitis, avoidance of antigen exposure (e.g., birds, mold) is critical.
- Oxygen Therapy:
- For patients with hypoxemia, oxygen therapy can improve symptoms and quality of life.
Pharmacologic Therapy
- Idiopathic Pulmonary Fibrosis (IPF):
- Antifibrotic agents such as pirfenidone and nintedanib slow the progression of fibrosis in IPF.
- Corticosteroids and Immunosuppressants:
- Used in inflammatory ILDs, such as sarcoidosis or hypersensitivity pneumonitis. In severe cases, drugs like methotrexate or mycophenolate may be added.
- Pulmonary Rehabilitation:
- Exercise training and education programs improve functional capacity and quality of life in ILD patients.
Surgical Therapy
- Lung Transplantation:
- Considered for patients with advanced ILD who fail to respond to medical therapy. Transplantation can significantly improve survival and quality of life.
Key Points
- Interstitial lung diseases (ILDs) involve inflammation and fibrosis of the lung interstitium, leading to progressive dyspnea and impaired gas exchange.
- Major etiologies include idiopathic pulmonary fibrosis (IPF), pneumoconioses, hypersensitivity pneumonitis, sarcoidosis, and connective tissue diseases.
- High-resolution CT (HRCT) is the gold standard for diagnosis, while pulmonary function tests show a restrictive pattern.
- Management includes antifibrotic agents for IPF, corticosteroids for inflammatory ILDs, and lung transplantation for advanced disease.
