Asthma for USMLE Step 2
Start your One-Week Free Trial
Already subscribed? Log in »
Asthma for the USMLE Step 2 Exam
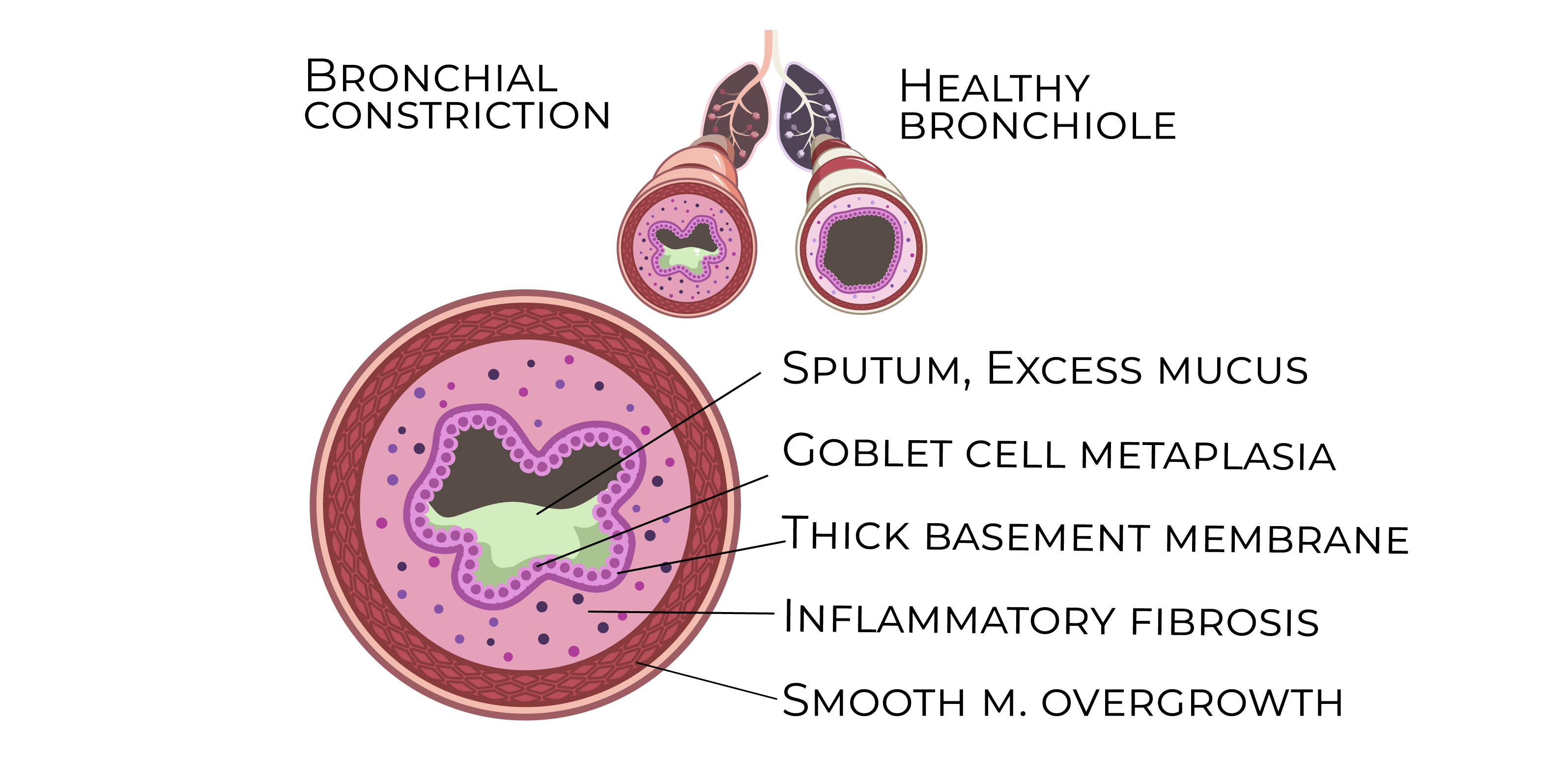
Pathophysiology
- Chronic Inflammation:
- Asthma involves chronic inflammation of the airways, driven by immune cells like eosinophils, mast cells, and Th2 cells. This inflammation leads to airway hyperresponsiveness, bronchoconstriction, and mucus overproduction.
- Inflammatory mediators such as histamine, leukotrienes, and prostaglandins cause bronchospasm and edema, contributing to airflow obstruction.
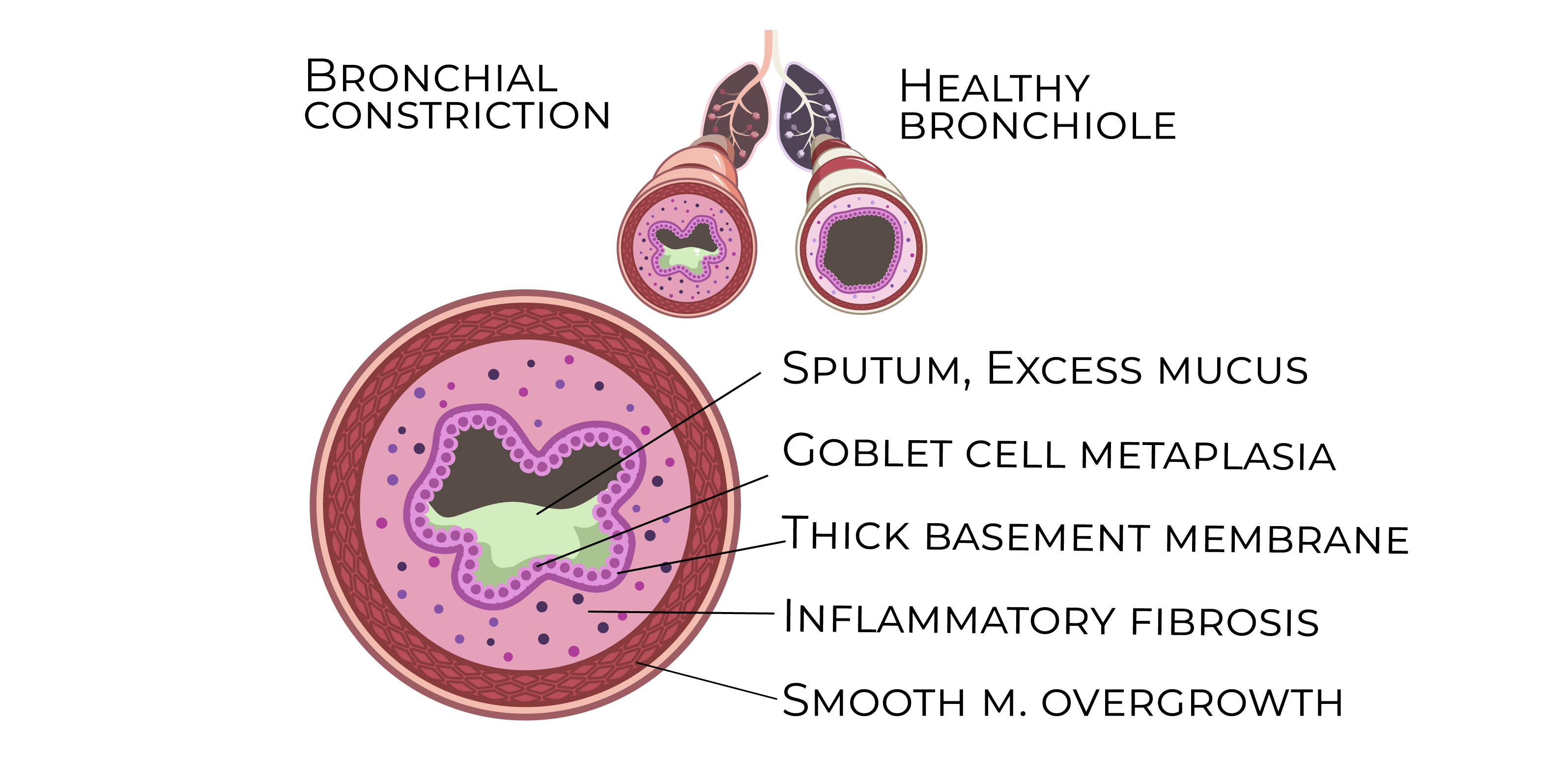
- Airway Hyperresponsiveness:
- Asthma is marked by an exaggerated response of the airway smooth muscle to stimuli such as allergens, cold air, or exercise, resulting in reversible bronchoconstriction.
- Airway Remodeling:
- Chronic inflammation can cause long-term structural changes in the airways, including smooth muscle hypertrophy, goblet cell hyperplasia, and subepithelial fibrosis. This can lead to more permanent airflow limitation over time.
Risk Factors
- Genetics:
- A family history of asthma, allergic rhinitis, or eczema increases the risk of asthma. Atopy, the tendency to develop IgE-mediated allergic responses, is a major risk factor.
- Environmental Exposures:
- Common asthma triggers include allergens (e.g., pollen, dust mites, animal dander), viral infections (particularly in children), air pollution, and tobacco smoke.
- Occupational Exposures:
- Certain jobs expose workers to asthma triggers, such as chemical fumes, dust, and industrial allergens.
Clinical Features
- Wheezing:
- Expiratory wheezing is the classic symptom of asthma, often episodic and triggered by specific stimuli like exercise or allergens.
- Dyspnea:
- Shortness of breath is common, especially during or after physical activity or at night.
- Cough:
- Asthma may present with a nonproductive cough, particularly at night.
- Chest Tightness:
- Many patients report a sensation of tightness or discomfort in the chest, often during exacerbations.
Diagnosis
- Spirometry:
- Asthma diagnosis is confirmed by demonstrating reversible airflow obstruction:
- Reduced FEV1/FVC ratio: Indicates obstructive lung disease.
- Reversibility: An increase in FEV1 by at least 12% and 200 mL after bronchodilator use confirms reversible airway obstruction.
- Peak Expiratory Flow (PEF):
- PEF monitoring helps assess asthma control and detect early signs of worsening disease.
- Methacholine Challenge Test:
- This bronchoprovocation test is used when spirometry is inconclusive. A significant drop in FEV1 after inhaling methacholine suggests airway hyperreactivity.
Management
- Stepwise Treatment Approach:
- Step 1 (Intermittent Asthma):
- Short-acting beta-agonists (SABAs) (e.g., albuterol) are used as needed for symptom relief.
- Step 2 (Mild Persistent Asthma):
- Low-dose inhaled corticosteroids (ICS) are the preferred maintenance therapy.
- Step 3 (Moderate Persistent Asthma):
- Combination of low-dose ICS + long-acting beta-agonists (LABAs) (e.g., salmeterol) or medium-dose ICS alone.
- Step 4 (Severe Persistent Asthma):
- High-dose ICS + LABA, with possible addition of tiotropium (a long-acting muscarinic antagonist) or biologics (e.g., omalizumab for allergic asthma).
- Acute Exacerbation Management:
- SABAs: First-line treatment for bronchospasm relief during exacerbations.
- Systemic Corticosteroids: Oral or IV prednisone is used in moderate-to-severe exacerbations to reduce inflammation.
- Oxygen: Administered to maintain SpO2 >90% in severe cases.
Complications
- Status Asthmaticus:
- A life-threatening asthma exacerbation that is unresponsive to standard treatment, requiring intensive care and potentially mechanical ventilation.
- Airway Remodeling:
- Chronic poorly controlled asthma can lead to irreversible structural changes in the airways, causing fixed airflow limitation.
- Pneumothorax:
- Rare but serious, this complication may occur during severe exacerbations, especially with overuse of bronchodilators.
Key Points
- Asthma is a chronic inflammatory disorder of the airways, often triggered by allergens, respiratory infections, and environmental factors.
- Diagnosis is confirmed by spirometry showing reversible airflow obstruction (FEV1/FVC improvement with bronchodilator use).
- The stepwise approach to management ranges from SABAs for intermittent asthma to ICS and LABAs for persistent disease, with biologics added in severe cases.
- Acute exacerbations are managed with SABAs, systemic corticosteroids, and oxygen if needed.
- Complications include status asthmaticus, airway remodeling, and pneumothorax, emphasizing the need for early diagnosis and proper management.
