Allergy & Hypersensitivity for USMLE Step 2
Start your One-Week Free Trial
Already subscribed? Log in »
Allergy for the USMLE Step 2 Exam
Allergy Overview
- Definition:
- Allergies are hypersensitivity reactions where the immune system overreacts to harmless antigens (allergens), causing a range of symptoms from mild to severe.
- Primarily mediated by IgE antibodies that sensitize mast cells and basophils to release histamine and other inflammatory mediators upon re-exposure to allergens.
- Common Allergens:
- Environmental: Pollens, animal dander, dust mites, mold spores.
- Food: Includes peanuts, tree nuts, shellfish, eggs, and milk.
- Medications: Commonly penicillin, NSAIDs, and certain vaccines.
- Insect Stings: Hymenoptera (e.g., bees, wasps).
- Occupational: Latex, chemicals, and materials in specific workplaces.
Mechanisms of Hypersensitivity
- Type I (IgE-Mediated) Hypersensitivity:
- Mechanism: Sensitization occurs on initial allergen exposure, leading to IgE production. Upon re-exposure, cross-linking of IgE on mast cells triggers degranulation, releasing histamine and other mediators.
- Examples: Allergic rhinitis, asthma, food allergies, and anaphylaxis.
- Type II (Cytotoxic) Hypersensitivity:
- Mechanism: IgG or IgM antibodies bind to cell-bound antigens, activating the complement system and causing cell lysis.
- Examples: Hemolytic anemia, Goodpasture syndrome.
- Type III (Immune Complex) Hypersensitivity:
- Mechanism: Antigen-antibody complexes deposit in tissues, leading to inflammation through complement activation.
- Examples: Serum sickness, systemic lupus erythematosus (SLE).
- Type IV (Delayed-Type) Hypersensitivity:
- Mechanism: T-cell mediated, occurring 24-72 hours post-exposure, involving cytokine release and macrophage activation.
- Examples: Contact dermatitis, tuberculin skin test reaction.
Clinical Presentations
- Allergic Rhinitis:
- Symptoms: Sneezing, nasal congestion, itchy eyes, and runny nose; may be seasonal or perennial.
- Diagnosis: Based on history, physical exam, and skin or IgE testing.
- Treatment: Intranasal corticosteroids, antihistamines, and avoidance of known allergens.
- Asthma:
- Symptoms: Cough, wheezing, dyspnea, and chest tightness, often triggered by allergens.
- Diagnosis: Pulmonary function tests (PFTs) with a reversible obstructive pattern; IgE testing may identify specific triggers.
- Treatment: Inhaled corticosteroids, bronchodilators, leukotriene receptor antagonists, and allergen avoidance.
- Atopic Dermatitis:
- Symptoms: Pruritic, erythematous rash, often affecting flexural surfaces.
- Diagnosis: Clinical evaluation, with allergy testing for suspected food or environmental triggers.
- Treatment: Emollients, topical corticosteroids, and avoidance of known irritants or allergens.
- Food Allergy:
- Symptoms: Urticaria, angioedema, gastrointestinal distress, respiratory symptoms, and anaphylaxis in severe cases.
- Diagnosis: Skin prick tests, serum IgE tests, and oral food challenges if necessary.
- Treatment: Allergen avoidance and carrying an epinephrine autoinjector for anaphylaxis.
- Drug Allergy:
- Symptoms: Ranges from mild rashes to severe anaphylactic reactions.
- Diagnosis: Based on history, skin testing (e.g., penicillin allergy) if available, and drug challenge.
- Treatment: Avoidance of the drug, substitution with alternatives, and desensitization if no alternatives exist.
- Anaphylaxis:
- Symptoms: Rapid-onset reaction involving multiple systems; symptoms include urticaria, angioedema, bronchospasm, hypotension, and shock.
- Diagnosis: Clinical, based on acute presentation following allergen exposure.
- Treatment: Immediate intramuscular epinephrine, followed by antihistamines and corticosteroids. Patients should carry an epinephrine autoinjector.
Diagnostic Testing
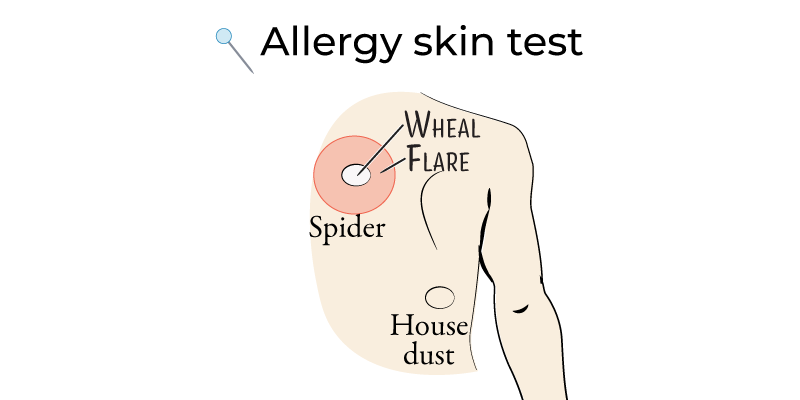
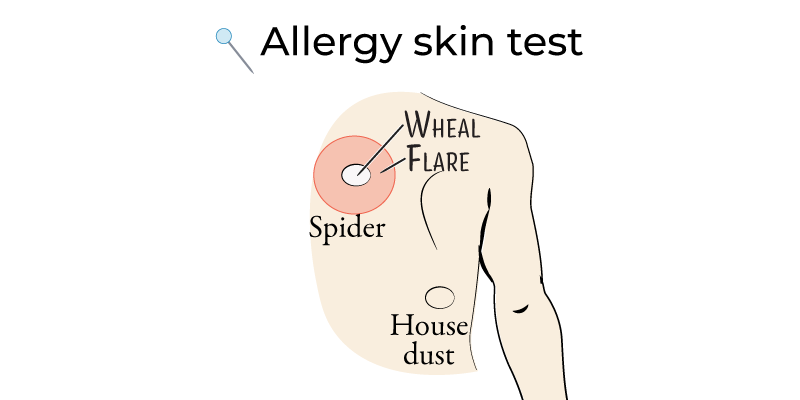
- Skin Prick Testing:
- Procedure: Small allergen amounts are pricked into the skin; a positive response produces a wheal and flare reaction.
- Indications: For allergic rhinitis, asthma triggers, and food allergies.
- Serum IgE Testing:
- Procedure: Measures allergen-specific IgE antibodies in the blood.
- Indications: Useful when skin testing is not possible, such as in patients with severe eczema.
- Oral Food Challenge:
- Procedure: Carefully supervised exposure to suspect allergen; gold standard for food allergy diagnosis.
Treatment Overview
- Avoidance: Key for managing allergies (e.g., allergen-proofing for environmental allergies, dietary restrictions for food allergies).
- Medications:
- Antihistamines: First-line treatment for allergic rhinitis and urticaria.
- Corticosteroids: Intranasal for rhinitis, inhaled for asthma, topical for dermatitis.
- Bronchodilators: Used in asthma for acute symptom relief.
- Immunotherapy:
- Subcutaneous and Sublingual Immunotherapy: For patients with allergic rhinitis or asthma unresponsive to standard therapies.
Key Points
- Allergies result from immune-mediated hypersensitivity, commonly IgE-driven, producing symptoms from mild rhinitis to severe anaphylaxis.
- Common allergens include environmental triggers, certain foods, medications, and insect stings.
- Diagnosis involves history, physical examination, and confirmatory tests like skin prick or IgE testing.
- Management includes allergen avoidance, pharmacologic therapy (antihistamines, corticosteroids), and immunotherapy for persistent cases.
- Anaphylaxis requires immediate epinephrine administration, and high-risk patients should carry an epinephrine autoinjector.
