USMLE/COMLEX 2 - Aortic Aneurysm & Dissection
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 2 & COMLEX-USA Level 2 from the Aortic Aneurysm & Dissection, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.

- --
VITAL FOR USMLE/COMLEX 2
Aortic Aneurysm
1. Abdominal Aortic Aneurysm (AAA) typically occurs in men over 65 with history of smoking, hypertension, and atherosclerosis.
2. Screening: One-time abdominal ultrasound for men aged 65 to 75 who have ever smoked.
3. AAA is defined as an aortic diameter greater than 3.0 cm; repair is recommended at ≥5.5 cm or rapid growth >0.5 cm in 6 months.
4. Asymptomatic AAAs are monitored by periodic ultrasound until they reach the size threshold for surgery.
5. Symptomatic AAAs (pain, pulsatile mass, or hypotension) require immediate surgical intervention.

Thoracic Aortic Aneurysm
6. Thoracic aortic aneurysms are associated with cystic medial degeneration seen in Marfan syndrome, Loeys-Dietz, and Ehlers-Danlos.
7. Symptoms may include chest pain, back pain, dysphagia, hoarseness, or cough due to mass effect.
8. Thoracic aneurysms are diagnosed with CT angiography.
9. Surgical repair is indicated for thoracic aneurysms ≥5.5 cm, or ≥5.0 cm in patients with connective tissue disorders or rapid expansion.
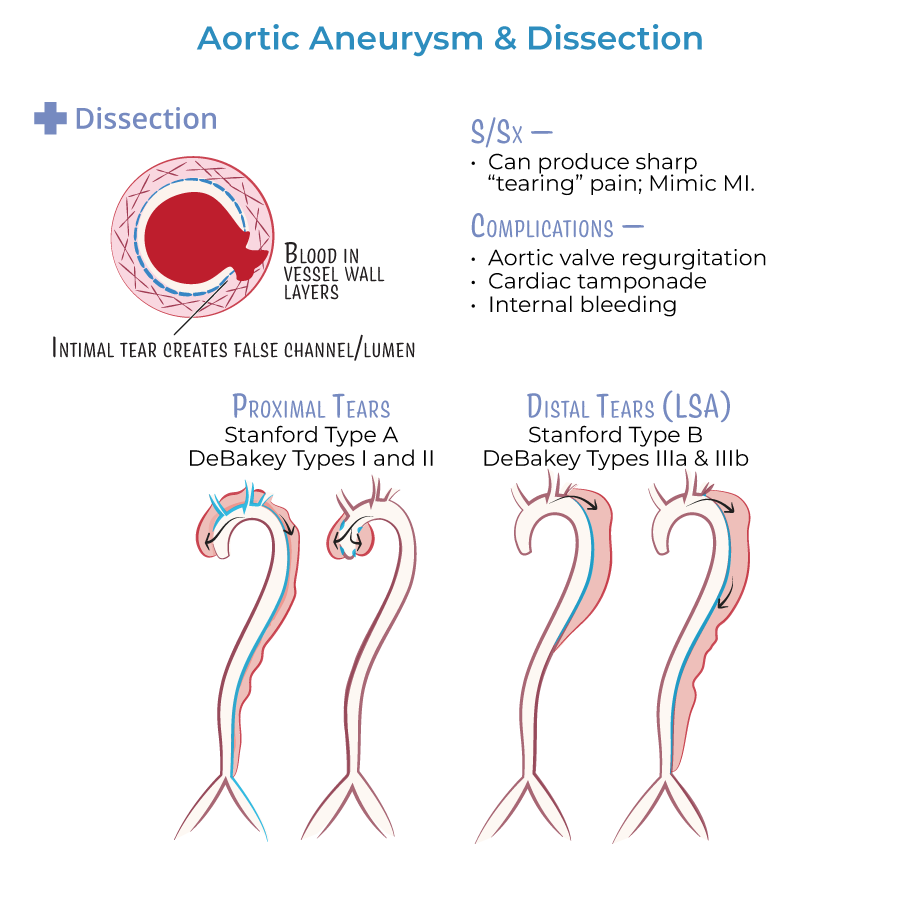
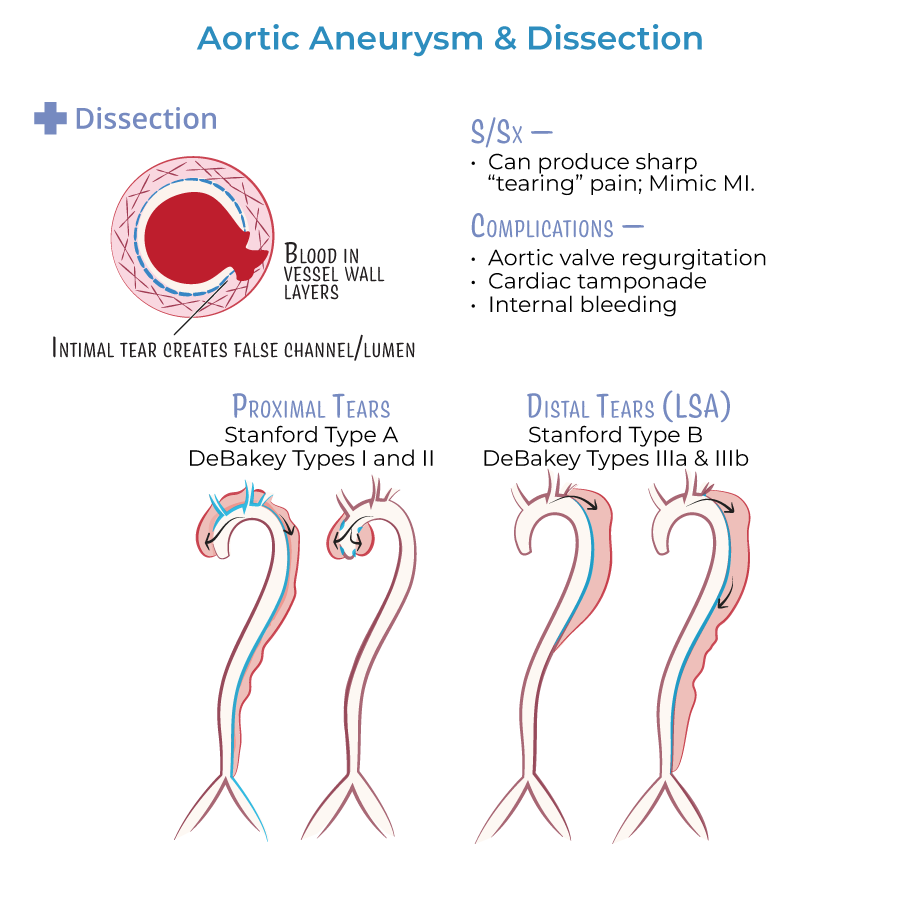
Aortic Dissection
10. Stanford Type A dissections (ascending aorta) are surgical emergencies.
11. Stanford Type B dissections (descending aorta) are managed medically first with blood pressure and heart rate control unless complications occur.
12. Initial management of aortic dissection includes immediate administration of IV beta-blocker (e.g., esmolol).
13. Chest x-ray may show a widened mediastinum; CT angiography is the gold standard for stable patients.
- --
HIGH YIELD
Etiology and Risk Factors
1. Hypertension is the most important risk factor for aortic dissection.
2. Smoking is the strongest modifiable risk factor for AAA development and progression.
3. Marfan syndrome and Ehlers-Danlos syndrome predispose to thoracic aneurysms and dissections.
Presentation
4. Aortic dissection presents with sudden onset severe, tearing chest or back pain.
5. Pulse deficits or blood pressure differentials between limbs are highly suggestive of dissection.
6. Dissection may involve aortic valve regurgitation, presenting as a new diastolic murmur.
7. Syncope, stroke symptoms, or limb ischemia can occur if major arterial branches are involved.
8. Abdominal aneurysms are often asymptomatic until they cause abdominal pain or rupture.
Diagnostic Approach
9. Stable patients with suspected dissection should undergo CT angiography.
10. Unstable patients (hypotension, pericardial tamponade suspicion) require bedside transesophageal echocardiography (TEE).
11. MRI angiography is ideal for stable patients with renal insufficiency or contrast allergy but is less available acutely.
Pharmacology
12. Use IV beta-blockers to lower heart rate and systolic blood pressure rapidly.
13. Fluoroquinolones should be avoided in patients with existing aneurysms due to increased risk of rupture.
Complications
14. Aortic dissection complications include stroke, myocardial infarction, pericardial tamponade, and renal failure.
15. Aortic aneurysm rupture presents with hypotension, flank or back pain, and may lead to sudden death if not rapidly repaired.
- --
Beyond the Tutorial
General Pathophysiology
1. Cystic medial necrosis is the underlying histopathologic finding in many thoracic aortic aneurysms and dissections.
2. Marfan syndrome involves FBN1 gene mutation affecting fibrillin-1, leading to weak aortic media.
3. Ehlers-Danlos vascular type involves COL3A1 mutations leading to fragile blood vessels.
Screening and Surveillance
4. Annual ultrasound surveillance for small AAA (3.0–3.9 cm); every 6 months if 4.0–5.4 cm.
5. Smoking cessation dramatically slows AAA expansion rate.
Management Priorities
6. In aortic dissection, beta-blocker first, then nitroprusside or other vasodilator if needed for further blood pressure control.
7. Avoid sole vasodilators without beta-blockade due to risk of reflex tachycardia worsening dissection.
Emergency Care
8. Stanford Type A dissection requires urgent surgical repair even if the patient is initially hemodynamically stable.
9. Stanford Type B dissection is treated medically unless there is end-organ ischemia, rupture, or uncontrolled pain/hypertension.
10. Surgical repair for rupture is mandatory for both abdominal and thoracic aneurysms.
