USMLE/COMLEX 2 - Supraventricular & Ventricular Arrhythmias
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 2 & COMLEX-USA Level 2 from the Supraventricular & Ventricular Arrhythmias tutorial, as well as points of interest that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
 Below is information not explicitly contained within the tutorial but important for USMLE Step 2.
Below is information not explicitly contained within the tutorial but important for USMLE Step 2.
- --
VITAL FOR USMLE/COMLEX 2
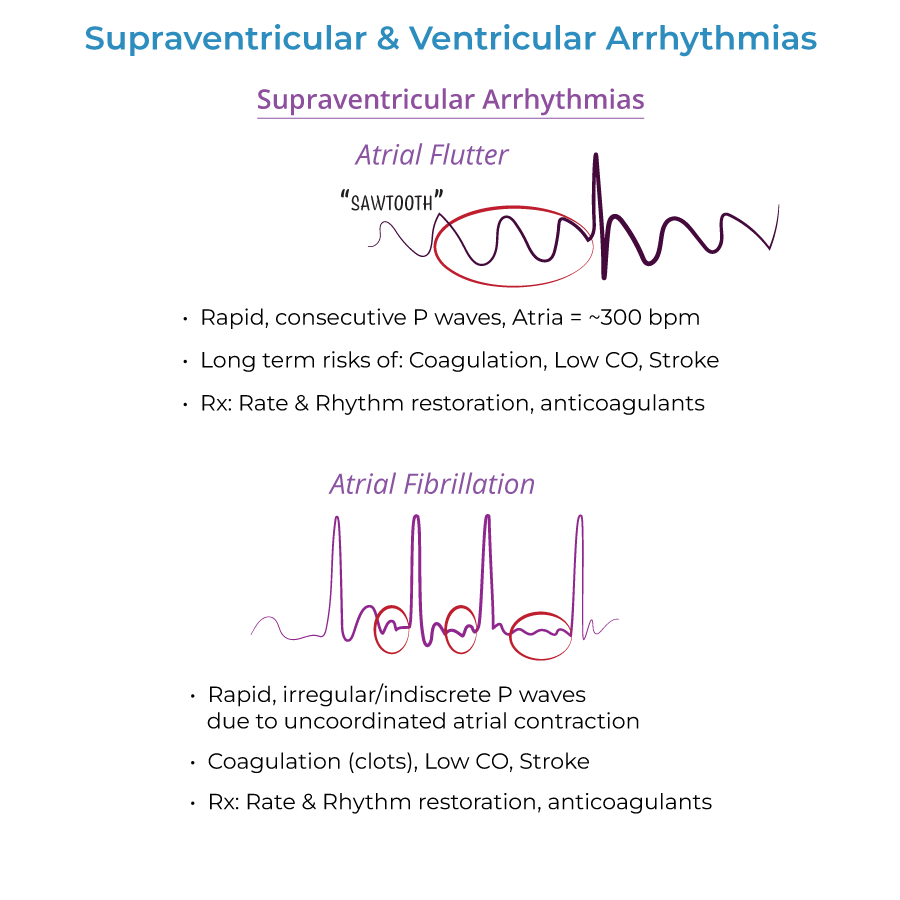
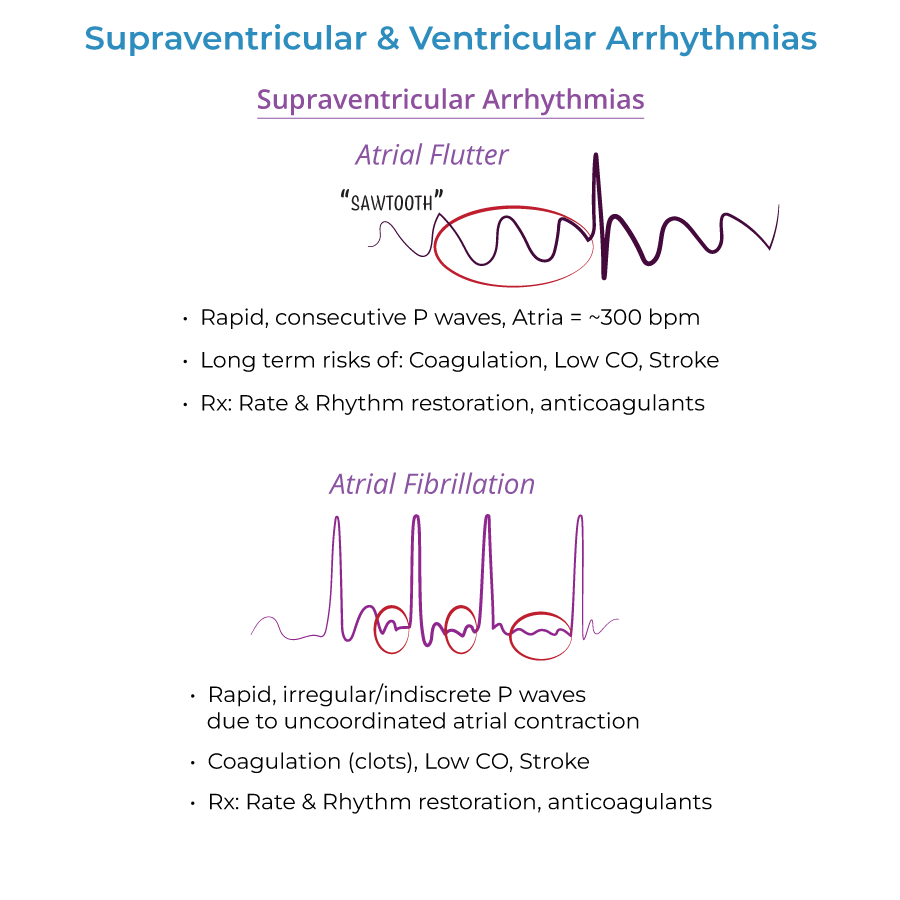
Atrial Flutter
1. Clinical presentation: May be none. Or, may cause palpitations, and reduced CO, difficulty breathing, weakness, chest discomfort, syncope.
2. Management approach: Rate control with drugs: beta-blockers, calcium channel blockers (verapamil, diltiazem). Rhythm control with cardioversion, drugs (antiarrhythmics), possibly ablation.
3. Anticoagulation: Anticoagulants (warfarin) are used to prevent thromboembolism.
Atrial Fibrillation
1. Diagnostic workup: Echocardiography to check for structural defects, thyroid function tests.
2. Treatment strategy: Rate control with beta blockers and nondihydropyridine calcium channel blockers. Anticoagulation before cardioversion therapy to prevent thromboembolism.
3. AV node blocker caution: AV node blockers possible (but rule out Wolff-Parkinson-White Syndrome with accessory pathway; look for wide QRS).
4. Complications: Stroke, systemic emboli.
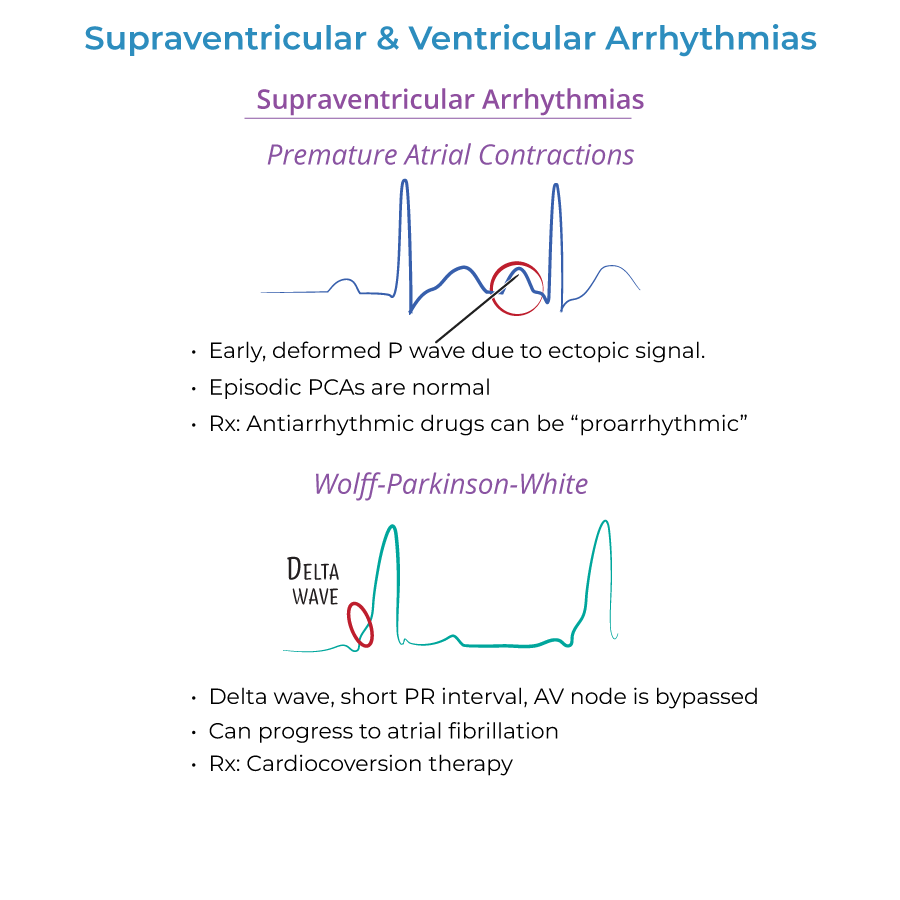
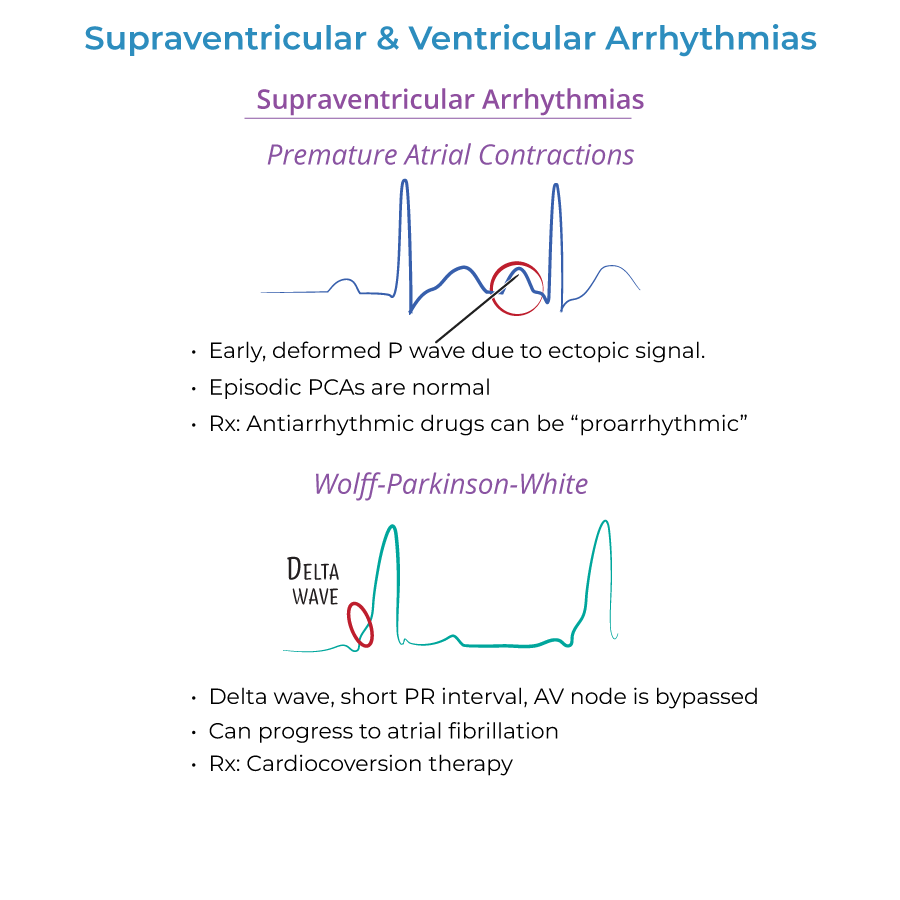
Wolff-Parkinson-White Syndrome
1. ECG findings: Short PR interval and positive delta wave at beginning of broad QRS complex; delta wave reflects early depolarization.
2. Treatment approach: Direct-current cardioversion therapy is preferred; long term treatment may require catheter ablation.
3. Critical medication warning: Beware digoxin/nondihydropyridine calcium channel blockers to WPW patients, as they may trigger ventricular fibrillation (fatal).
Ventricular Arrhythmias
1. Ventricular tachycardia management: Cardioversion, antiarrhythmic drugs, defibrillator implant.
2. Torsades de Pointes treatment: Magnesium.
3. Ventricular fibrillation emergency management: CPR & Defibrillation.
- --
HIGH YIELD
Atrial Arrhythmias
1. Atrial flutter pathophysiology: Only ½ - 1/3 of the electrical impulses make it through the AV node and reach the ventricles, so heart rate is increased ~150 beats per minute.
2. Atrial fibrillation mechanism: Atria do not contract in coordinated fashion, but send fast and irregular signals to ventricles increase heart rate.
3. Risk factors for atrial flutter: Commonly occurs in healthy people, but risk increases with other cardiac conditions, binge alcohol consumption, diabetes.
4. Risk factors for atrial fibrillation: Other cardiac problems, hyperthyroidism, obesity, diabetes, lung disease, binge alcohol consumption.
Wolff-Parkinson-White Syndrome
1. Pathophysiology: Occurs as result of AV node bypass, called bundle of Kent.
2. Clinical presentation: May be asymptomatic. May have episodes of increased heart rate, chest pain, dizziness, palpitations, difficulty breathing.
3. Associated cardiac anomalies: Associated with Ebstein anomaly, displaced tricuspid valve.
4. Potential complications: Atrial fibrillation can develop (depends on presence of antegrade conduction through accessory connection).
Ventricular Arrhythmias
1. Ventricular tachycardia presentation: May be asymptomatic if duration is short (aka, paroxysmal) or rate is not excessive; If sustained, palpitations, difficulty breathing, chest pain, dizziness, fainting, death.
2. Complications of ventricular tachycardia: Can lead to heart failure, unconsciousness, sudden death by cardiac arrest.
3. Torsades de Pointes presentation: Recurrent palpitations, dizziness, fainting, difficulty breathing.
4. Triggers for Torsades: Electrolyte imbalances (hypocalcemia, hypokalemia); Medications (antiarrhythmics, tricyclic antidepressants, anti-histamines when taken with erythromycin. In individuals with Long QT Syndrome, can be triggered by stress, fear, etc.
Long QT Syndrome
1. Clinical significance: Prone to torsades de pointes, which can cause syncope, ventricular fibrillation, and sudden death.
2. Etiology: Often inherited, but can be acquired (electrolyte imbalances, antihistamines, decongestants, diuretics, antiarrhythmic drugs, antidepressants, etc.).
3. Inherited forms: Romano-Ward Syndrome (Types 1-3) and Jervell and Lange-Nielsen Syndrome, which is also associated with congenital deafness.
- --
Beyond the Tutorial
Management Considerations
1. Rate vs. rhythm control: When to choose rate control vs. rhythm control strategies based on patient characteristics, symptom burden, and comorbidities.
2. Anticoagulation scoring systems: Use of CHA₂DS₂-VASc score to guide anticoagulation decisions in atrial fibrillation.
3. Ablation indications: When to refer for catheter ablation for various arrhythmias.
4. Device therapy selection: Indications for pacemakers vs. ICDs vs. cardiac resynchronization therapy.
Acute Management
1. Hemodynamically unstable arrhythmias: Immediate synchronized cardioversion for unstable tachyarrhythmias.
2. Adenosine use: Role in diagnosis and treatment of supraventricular tachycardias.
3. Advanced cardiac life support: Current ACLS algorithms for various arrhythmias.
4. Post-arrest care: Management after successful resuscitation from cardiac arrest.
Special Populations
1. Arrhythmias in pregnancy: Modifications to evaluation and management during pregnancy.
2. Pediatric considerations: Approach to arrhythmias in children versus adults.
3. Perioperative arrhythmias: Evaluation and management in surgical patients.
4. Athletes with arrhythmias: Sports participation considerations for athletes with various arrhythmias.
Emerging Concepts
1. Atrial fibrillation ablation: Pulmonary vein isolation and newer ablation strategies.
2. Subcutaneous ICDs: Role compared to traditional transvenous devices.
3. Wearable defibrillators: Indications and limitations.
4. Genetic testing: Implications for family screening and management of inherited arrhythmia syndromes.
