USMLE/COMLEX 2 - Small Vessel Vasculitis
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 2 & COMLEX-USA Level 2 from the Small Vessel Vasculitis tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
 5. Eosinophilic granulomatosis with polyangiitis (EGPA):
5. Eosinophilic granulomatosis with polyangiitis (EGPA):
 6. Microscopic polyangiitis (MPA):
6. Microscopic polyangiitis (MPA):
- --
VITAL FOR USMLE/COMLEX 2
General Concepts of Small Vessel Vasculitis
1. Small vessel vasculitides cause inflammation and necrosis of capillaries, venules, and small arterioles, leading to multiorgan ischemia and damage.
2. Common systemic symptoms include fever, fatigue, weight loss, arthralgia, and myalgias.
3. First-line treatment for most cases is high-dose corticosteroids plus immunosuppressants for organ-threatening disease.
ANCA-Associated Vasculitides
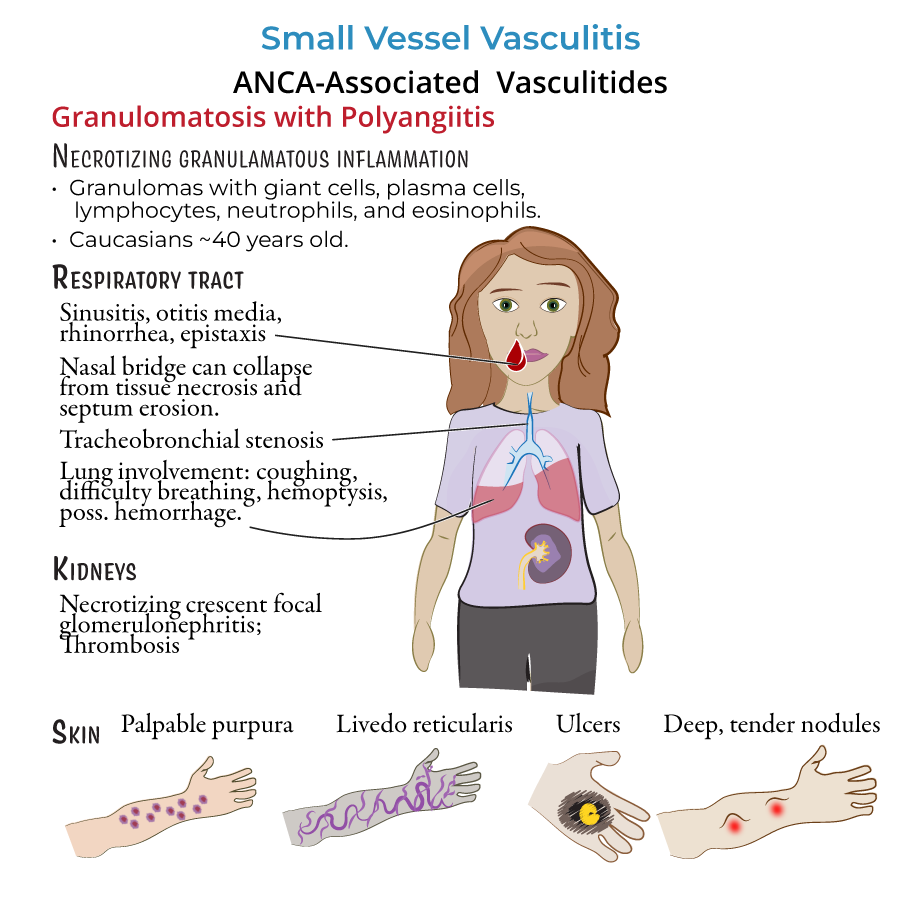
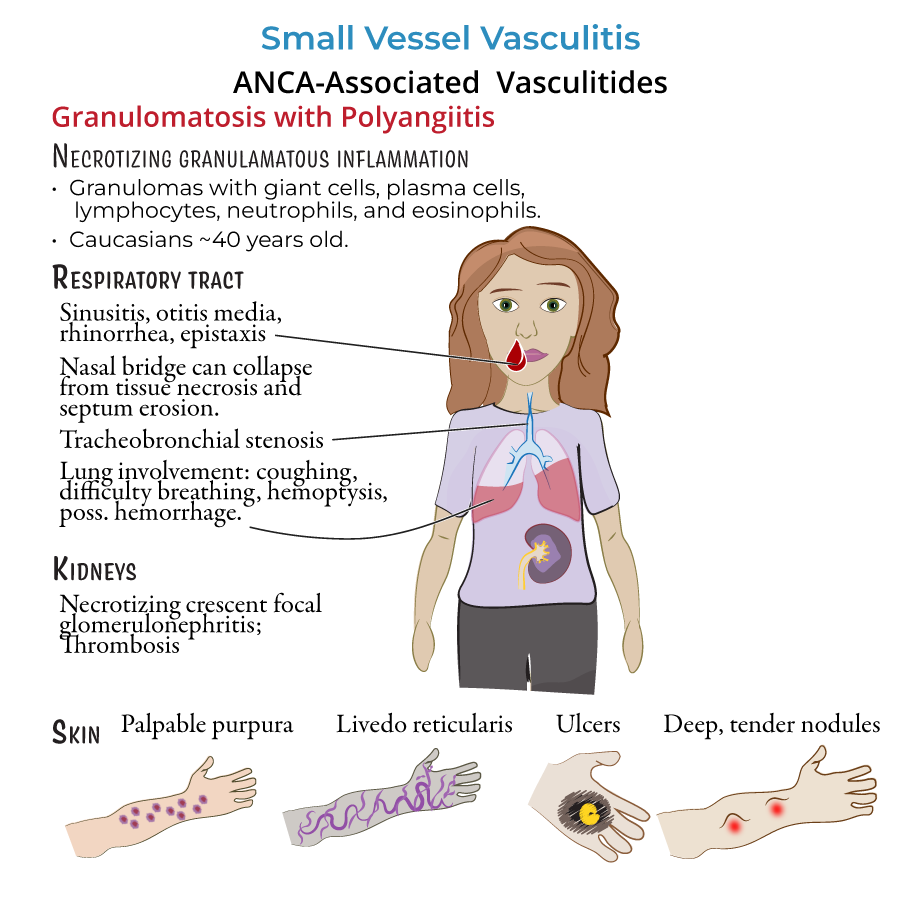
4. Granulomatosis with polyangiitis (GPA):
- Involves upper and lower respiratory tracts and kidneys.
- Clinical signs:
- Sinusitis, otitis media, epistaxis, nasal septal perforation (saddle nose).
- Lung involvement: cough, hemoptysis, cavitary lesions.
- Rapidly progressive glomerulonephritis (RPGN) leading to renal failure.
- Palpable purpura, livedo reticularis.
- Associated with c-ANCA (anti-proteinase 3).
- Chest imaging: nodular cavitary lesions.
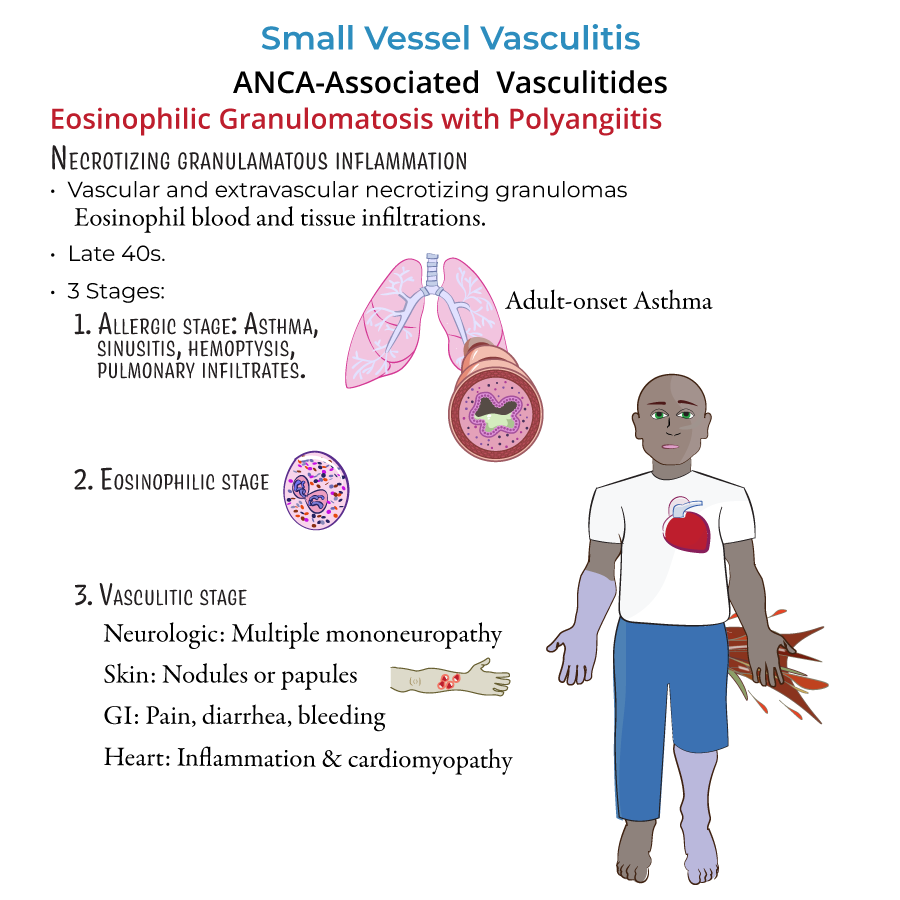
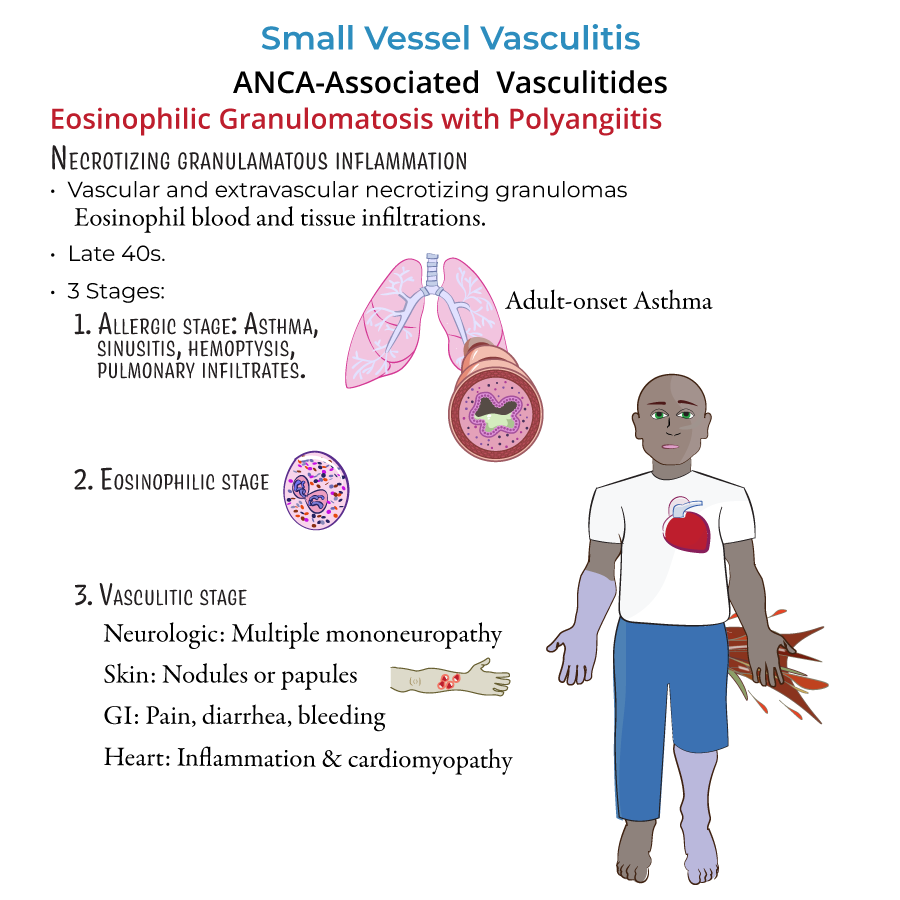
 5. Eosinophilic granulomatosis with polyangiitis (EGPA):
5. Eosinophilic granulomatosis with polyangiitis (EGPA):
- Triad: asthma, eosinophilia, vasculitis.
- Key stages:
- Allergic phase: adult-onset asthma, allergic rhinitis, sinusitis.
- Eosinophilic phase: peripheral blood eosinophilia, eosinophilic pneumonia.
- Vasculitic phase: mononeuritis multiplex, cardiac involvement (leading cause of death), palpable purpura.
- Associated with p-ANCA (anti-MPO).
- Cardiac monitoring is essential due to risk of myocarditis.
 6. Microscopic polyangiitis (MPA):
6. Microscopic polyangiitis (MPA):
- Presents with RPGN (rapid renal decline) and palpable purpura.
- Lung involvement possible (alveolar hemorrhage, pulmonary fibrosis).
- No granulomas on biopsy (vs GPA).
- Associated with p-ANCA.
- --
HIGH YIELD
Non-ANCA Small Vessel Vasculitides
1. IgA Vasculitis (Henoch-Schönlein Purpura):
- Common in children, follows upper respiratory infection.
- Classic tetrad:
- Palpable purpura on buttocks and legs.
- Arthralgias.
- Abdominal pain (possible GI bleeding).
- Renal involvement (IgA nephropathy, hematuria).
- Diagnosis is clinical; biopsy shows IgA deposition in mesangium.
- Management: supportive care; corticosteroids if severe.
- Systemic immune-complex vasculitis caused by circulating cryoglobulins.
- Triad:
- Palpable purpura.
- Arthralgia.
- Glomerulonephritis.
- Associated with Hepatitis C infection.
- Diagnosis:
- Serum cryoglobulins positive.
- Low complement levels (especially C4).
- Treatment includes antiviral therapy for Hepatitis C and immunosuppressants if severe.
- Both systemic autoimmune diseases can involve secondary small vessel vasculitis.
- Clinical presentation varies based on organs affected (skin, kidneys, CNS).
Diagnostic Testing
4. ANCA testing:
- c-ANCA (PR3) for GPA.
- p-ANCA (MPO) for MPA and EGPA.
- GPA: necrotizing granulomatous inflammation.
- MPA: necrotizing, non-granulomatous.
- EGPA: eosinophilic granulomas.
- --
Beyond the Tutorial
Management Specifics
1. GPA and MPA:
- Induction: corticosteroids + rituximab or cyclophosphamide.
- Maintenance: azathioprine, methotrexate, or rituximab.
- Mild disease: corticosteroids alone.
- Severe disease: corticosteroids plus cyclophosphamide or mepolizumab (IL-5 inhibitor).
- Corticosteroids for severe GI, renal, or joint involvement.
- Treat underlying HCV plus immunosuppression if needed.
Complications to Monitor
5. GPA:
- Pulmonary hemorrhage.
- Renal failure.
- Saddle nose deformity.
- Heart failure from eosinophilic myocarditis.
- Pulmonary-renal syndrome.
- Chronic kidney disease.
