USMLE/COMLEX 2 - Pulmonary Embolism and Deep Vein Thrombosis
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 2 CK & COMLEX-USA Level 2 from the Pulmonary Embolism & Deep Vein Thrombosis tutorial, focusing on clinical management and treatment decision-making that are essential for these exams. See the tutorial notes for further details and relevant links.
 2. High-Risk Populations:
Below is information not explicitly contained within the tutorial but important for USMLE Step 2 CK & COMLEX Level 2.
2. High-Risk Populations:
Below is information not explicitly contained within the tutorial but important for USMLE Step 2 CK & COMLEX Level 2.
- --
VITAL FOR USMLE/COMLEX 2
Clinical Presentation & Recognition
1. Pulmonary Embolism (PE): Presents with dyspnea, tachypnea, chest pain, hypoxemia, and ventilation-perfusion mismatch.
2. Respiratory Manifestations: Tachypnea, respiratory alkalosis, and hypoxemia due to V/Q mismatch.
3. Cardiovascular Manifestations: Tachycardia and potential right heart failure due to increased pulmonary vascular resistance.
4. Neurological Manifestations: Altered mental state, particularly important to recognize in elderly patients.
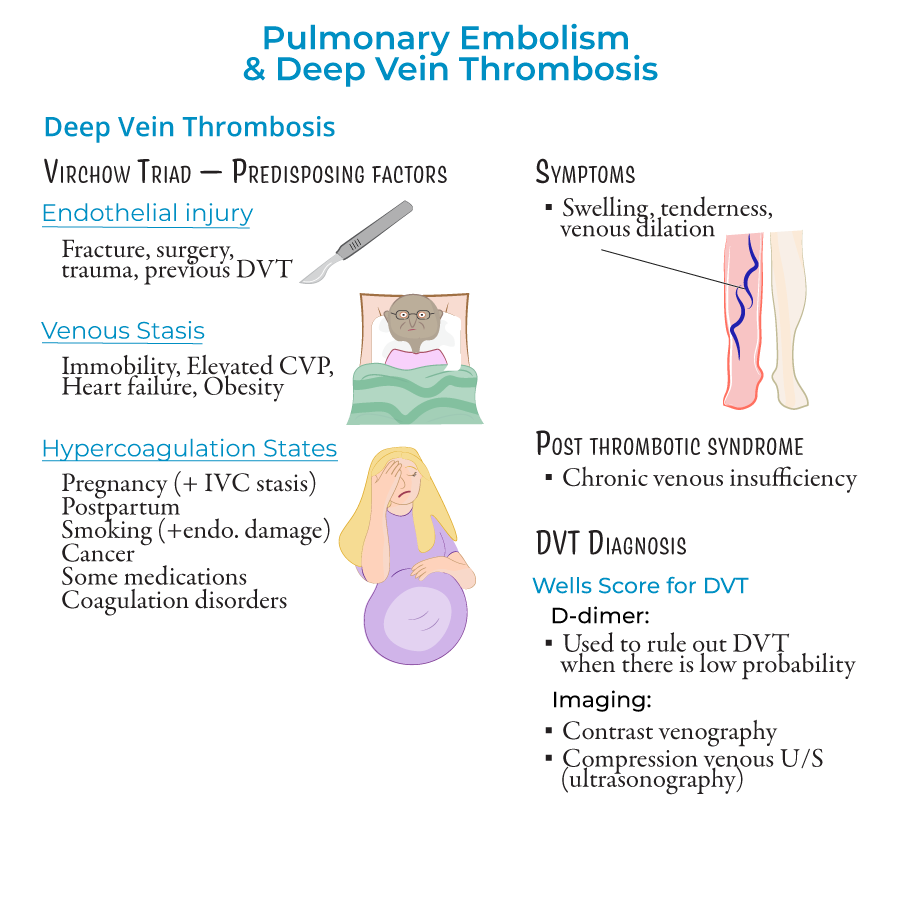
5. Deep Vein Thrombosis (DVT): When symptomatic, presents with unilateral leg swelling, tenderness, and signs of venous dilation; can also occur in upper body (less common).
Risk Stratification & Assessment
1. PE Classification by Risk:
- Massive (High Risk): Hemodynamically unstable with hypotension
- Intermediate (Submassive): Stable but with right ventricular dysfunction
- Low Risk: Hemodynamically stable without right ventricular dysfunction
- Saddle Emboli: Located at pulmonary trunk bifurcation
- Lobar, Segmental, Subsegmental: Located in respective arterial branches
- Wells Score for PE: Score ≥4 indicates PE likely; <2 low probability, 2-6 moderate, >6 high probability
- Wells Score for DVT: Based on swelling, edema, and likelihood of alternative diagnosis
Diagnostic Approach
1. Initial Workup:
- Clinical suspicion based on presentation and risk factors
- Clinical probability assessment using Wells criteria
- D-dimer testing (>500 ng/mL suggests possible PE, requiring further testing)
- CT Angiography: Most widely used; visualizes disruption of blood flow in pulmonary arteries
- Ventilation-Perfusion Scan: Non-invasive test indicating blood clot presence
- Chest X-ray: May show atelectasis, Hampton hump (pulmonary infarction), Westermark sign (oligemic areas), or pleural effusion
- Sinus tachycardia
- S1Q3T3 pattern (S wave in lead I, inverted Q and T waves in lead III)
- Venous Ultrasonography with Compression: First-line imaging
- Contrast Venography: Alternative when ultrasound inconclusive
- D-dimer: Fibrin degradation product used to rule out low-probability cases
- Arterial blood gases: May show hypoxemia and respiratory alkalosis
Treatment Strategies
1. Supportive Care:
- Oxygen administration
- Fluid resuscitation with saline
- Vasopressors for hemodynamic support if needed
- Initial Treatment: Heparin, enoxaparin, or fondaparinux
- Long-term Treatment: Warfarin
- Embolectomy: Surgical removal of clot
- Clot Dissolution: Thrombolytic therapy to restore pulmonary artery flow
- Mechanical: Sequential compression devices (SCDs) to prevent venous stasis
- Pharmacologic: Low-dose enoxaparin or heparin
Risk Factors & Prevention
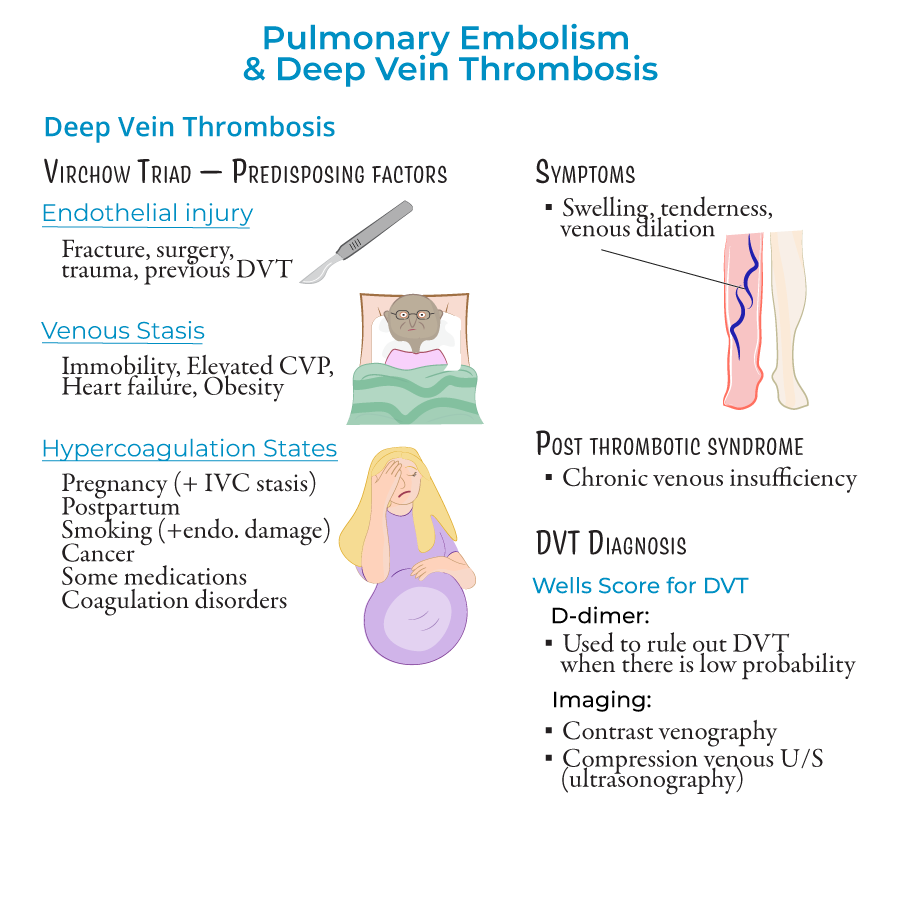
1. Virchow's Triad (Factors predisposing to DVT):
- Endothelial Injury: Fracture, surgery, trauma, previous DVT
- Venous Stasis: Immobility, elevated central venous pressure, heart failure, obesity
- Hypercoagulable States: Pregnancy, postpartum period, smoking, cancer, hormonal contraceptives/replacement therapies, coagulation disorders (e.g., Factor V Leiden)
 2. High-Risk Populations:
2. High-Risk Populations:
- Individuals with multiple predisposing factors (e.g., pregnant women on bed rest)
- Post-surgical patients, especially orthopedic procedures
- Malignancy patients
- Early mobilization
- Mechanical prophylaxis (SCDs)
- Pharmacologic prophylaxis in selected patients
- --
HIGH YIELD
Clinical Decision Making
1. When to Suspect PE: Unexplained dyspnea, tachypnea, chest pain, especially with risk factors for DVT.
2. Differential Diagnosis Considerations: Non-specific symptoms can make diagnosis challenging.
3. Risk Factor Assessment: Identifying patients with multiple predisposing factors from Virchow's Triad.
4. Wells Score Application: Using clinical decision tools appropriately to guide diagnostic workup.
5. Recognition in Special Populations: Altered presentation in elderly (mental status changes) requires high clinical suspicion.
Diagnostic Test Selection & Interpretation
1. D-dimer Utilization: Useful for ruling out PE in low-probability patients; levels >500 ng/mL warrant further investigation.
2. Imaging Selection Logic:
- CT angiography as first-line imaging for suspected PE
- Venous ultrasonography with compression for suspected DVT
- Hampton Hump: Wedge-shaped shadow indicating pulmonary infarction, typically in lower lobes
- Westermark Sign: Focal oligemia appearing as poorly perfused area
Treatment Decision Points
1. Anticoagulation Initiation: When to start therapy based on clinical suspicion and risk assessment.
2. Intervention Selection: Determining appropriate anticoagulant based on clinical context.
3. Advanced Treatment Decisions: When to consider embolectomy or thrombolysis for massive PE.
4. Prophylaxis Decision-Making: Risk stratification to determine appropriate preventive measures.
5. Management of Complications: Addressing post-thrombotic syndrome and recurrent events.
Pulmonary Infarction Management
1. Recognition: Small emboli causing tissue ischemia, most often in lower lobes.
2. Radiographic Identification: Wedge-shaped "Hampton Hump" on chest X-ray.
3. Clinical Significance: Indicates tissue damage requiring appropriate management.
4. Treatment Approach: Anticoagulation and supportive care.
5. Monitoring: Follow-up imaging to assess resolution.
Special Considerations
1. Pregnancy-Associated VTE: Higher risk during pregnancy and postpartum period.
2. Cancer-Associated Thrombosis: Requires specific management approaches.
3. Recurrent VTE Management: Long-term anticoagulation strategies.
4. Upper Extremity DVT: Less common but requires similar diagnostic approach.
5. Post-thrombotic Syndrome: Long-term complication of DVT due to venous valve damage.
- --
Beyond the Tutorial
Advanced Management Considerations
1. Anticoagulation Selection: Direct oral anticoagulants (DOACs) vs. warfarin vs. low molecular weight heparin based on patient factors.
2. Thrombolytic Therapy: Specific indications, contraindications, and administration protocols.
3. Inferior Vena Cava Filters: Indications, placement considerations, and complications.
4. Extended Anticoagulation: Decision-making for duration based on risk factors and recurrence risk.
5. Managing Anticoagulation Complications: Approaching bleeding events in anticoagulated patients.
Special Population Management
1. Pregnancy: Anticoagulation selection and monitoring during pregnancy and postpartum.
2. Renal Impairment: Dose adjustments and monitoring for anticoagulants.
3. Malignancy: Cancer-associated thrombosis management strategies.
4. Elderly: Balancing bleeding and thrombotic risks in older patients.
5. Thrombophilia: Management approaches for inherited hypercoagulable states.
Procedural Skills
1. Central Line-Associated DVT Prevention: Techniques to reduce catheter-associated thrombosis.
2. Thrombolytic Administration: Proper protocols for systemic and catheter-directed thrombolysis.
3. Ultrasonography Technique: Compression ultrasound approach for DVT diagnosis.
4. Arterial Blood Gas Interpretation: Recognizing PE-associated changes.
5. Post-PE Functional Assessment: Exercise testing and functional capacity evaluation.
Quality Measures & Systems-Based Practice
1. VTE Prophylaxis Protocols: Institutional approaches to prevent hospital-acquired VTE.
2. Care Transitions: Anticoagulation management across inpatient and outpatient settings.
3. Quality Metrics: Hospital-acquired VTE rates as healthcare quality indicator.
4. Cost-Effective Diagnostic Strategies: Using clinical decision rules to guide testing.
5. Patient Education Programs: Improving compliance with prevention and treatment.
Emerging Concepts
1. Risk-Adapted Treatment Duration: Individualizing anticoagulation duration based on risk assessment.
2. Subsegmental PE Management: Controversial approaches to small peripheral emboli.
3. Post-PE Syndrome: Chronic complications following PE similar to post-thrombotic syndrome.
4. Catheter-Directed Interventions: Advanced approaches for massive and submassive PE.
5. Outpatient Management: Selection criteria for ambulatory treatment of PE and DVT.
