USMLE/COMLEX 2 - Myocardial Infarctions
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 2 CK & COMLEX-USA Level 2 from the Myocardial Infarctions: Diagnosis & Treatment tutorial, focusing on clinical management and treatment decision-making that are essential for these exams. See the tutorial notes for further details and relevant links.
 Below is information not explicitly contained within the tutorial but important for USMLE Step 2 CK & COMLEX Level 2.
Below is information not explicitly contained within the tutorial but important for USMLE Step 2 CK & COMLEX Level 2.
- --
VITAL FOR USMLE/COMLEX 2
Epidemiology & Risk Factors
1. Demographic patterns: Myocardial infarction incidence after age 35, from highest to lowest: Black males > Black females > White males > White females.
2. Gender differences: Timing of first MI tends to be earlier in men than women by about 10 years, possibly related to risk factors like smoking and hyperlipidemia.
3. Mortality trends: Although mortality has declined overall, rates are higher in women than male peers, especially for young and/or minority women.
4. Key modifiable risk factors: Dyslipidemia, diabetes mellitus, hypertension, smoking (including e-cigarettes), obesity, psychosocial stress, alcohol consumption, poor diet.
5. Awareness challenges: Many people, especially women, are unaware of risk factors and symptoms—a significant obstacle to prevention and treatment.
Clinical Presentation
1. Definition: Myocardial infarction is defined as myocardial injury with ischemia.
2. Typical symptom pattern: Chest pain (angina) variably described as dull, sharp, squeezing, pressure, or simply discomfort, often radiating to arms, neck, jaw, or back.
3. Atypical presentations: Not all patients experience angina—absence of chest pain and/or young age often leads to missed or delayed diagnosis.
4. Symptom timeline:
- Prodromal symptoms: Days, weeks, or months prior to heart attack
- Acute symptoms: Experienced at the time of the event
- Silent MI: No noticeable symptoms
Diagnostic Approach
1. ECG timing: Should be administered as soon as possible when MI is suspected and re-administered frequently to observe the evolution of the infarction.
2. ECG interpretation: Distinguishes between ST-segment elevated (STEMI) or Non-ST elevated (NSTEMI) myocardial infarctions, influencing treatment strategies.
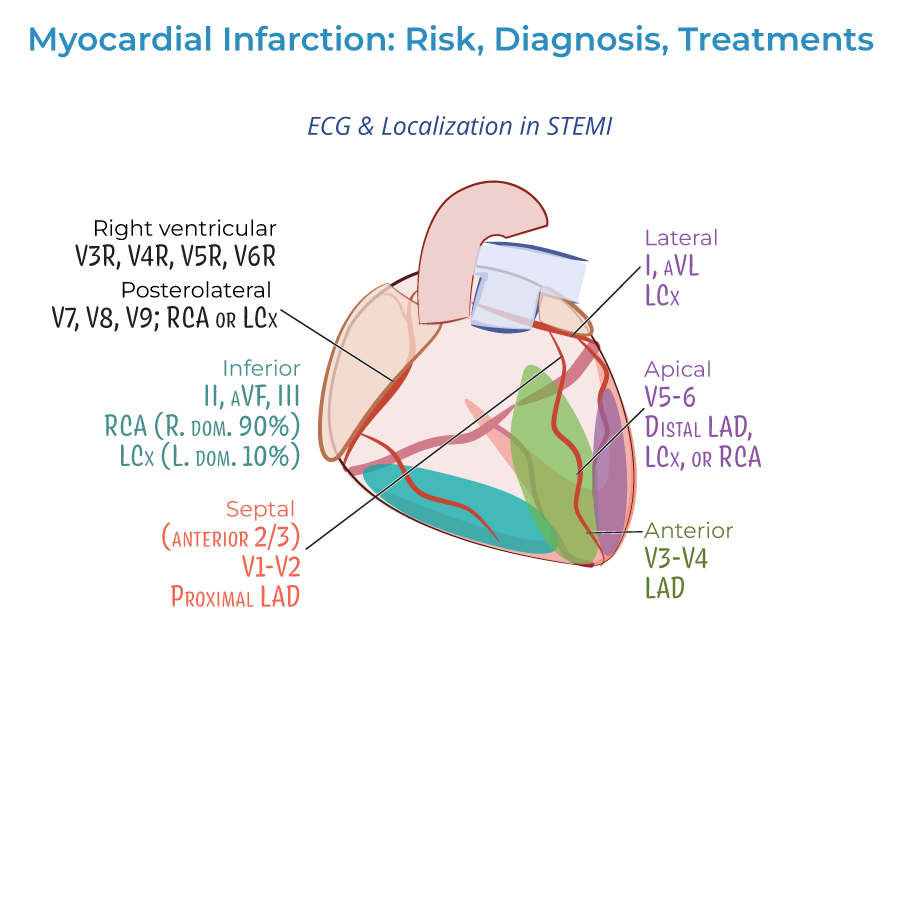
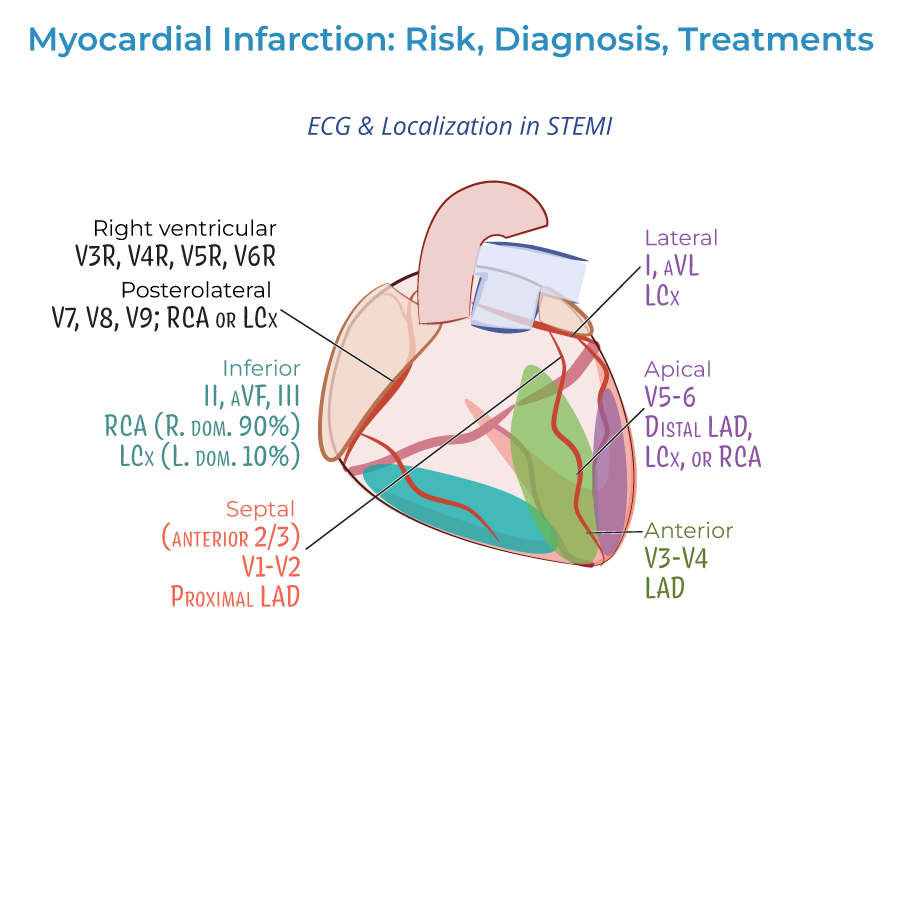
3. ECG localization: Different lead changes indicate specific infarct locations:
- Lateral infarction: Leads I and aVL; left circumflex artery
- Apical infarctions: Leads V5 and V6; left circumflex or right coronary arteries
- Anterior infarctions: Leads V3 and V4; left anterior descending artery
- Anterior septal infarctions: Leads V1 and V2; proximal left anterior descending artery
- Inferior infarctions: Leads II, aVF, and III; right coronary artery or left circumflex artery
- Right ventricular infarctions: Requires additional leads V3R through V6R
- Posterolateral infarctions: Requires additional posterior leads V7-V9; right coronary or left circumflex artery
Treatment Principles
1. Time sensitivity: Treatment should begin as soon as possible, ideally before hospital arrival, to reduce the extent of myocardial necrosis.
2. Pre-hospital treatment:
- Oxygen administration when saturation is less than 90%
- Aspirin for antiplatelet effects
- Nitrates for chest pain (morphine is an option if nitrates are ineffective)
- STEMI: Emergency PCI recommended; if unavailable, fibrinolytic drugs must be given ASAP
- NSTEMI: Unstable, complicated cases require immediate PCI/CABG; uncomplicated cases may wait longer and may not require revascularization
- Fibrinolytic drugs generally not recommended for NSTEMI as potential risks outweigh benefits
- Antiplatelets (aspirin, clopidogrel, others)
- Anticoagulation drugs (unfractionated or low molecular weight heparin)
- Beta-blockers (or calcium-channel blockers)
- Statins
- ACE inhibitors
- --
HIGH YIELD
ECG Localization and Vessel Correlation
1. Anterior infarction: Changes in leads V3 and V4; associated with blockages in the left anterior descending artery.
2. Anterior septal infarction: Changes in leads V1 and V2; associated with blockages in the proximal left anterior descending artery.
3. Lateral infarction: Changes in leads I and aVL; often the result of blockage in the left circumflex artery.
4. Inferior infarction: Changes in leads II, aVF, and III; associated with blockages in the right coronary artery, or less frequently, the left circumflex artery.
5. Apical infarction: Changes in leads V5 and V6; often associated with blockages in the left circumflex or right coronary arteries.
Demographic and Risk Factor Details
1. Mortality variation: Rates are higher in women than men, especially for young and/or minority women.
2. MI as heart failure precursor: Myocardial infarction is an important cause of heart failure, which is itself a significant cause of death.
3. Smoking risk: Includes possible risk from daily use of e-cigarettes.
4. Dietary factors: Poor diet, particularly those low in fruits and vegetables, increases risk.
5. Awareness gap: Unawareness of risk factors and symptoms represents a significant obstacle to prevention and treatment.
Clinical Presentation Nuances
1. Prodromal timeline: Symptoms may appear days, weeks, or even months prior to the heart attack.
2. Sleep disturbances: Many patients report sleep problems, particularly during the prodromal period.
3. Pain radiation patterns: Some patients experience pain in arms, neck, jaw, or back, which may radiate from the chest.
4. Psychological symptoms: Patients may feel unaccountably anxious or experience a sense of impending doom prior to and during the heart attack.
5. Diagnosis challenges: Absence of chest pain and/or young age of a patient often leads to missed or delayed diagnosis, associated with worse outcomes.
Treatment Decision-Making
1. STEMI management: Patients with STEMI should receive emergency PCI; if unavailable, fibrinolytic drugs must be given as soon as possible.
2. NSTEMI approach: Unstable, complicated NSTEMI often requires immediate PCI or CABG; uncomplicated NSTEMI patients may wait longer, and revascularization may not be necessary.
3. Fibrinolytic considerations: Generally not recommended for NSTEMI patients because potential risks outweigh benefits.
4. Long-term management: Focuses on reducing risk factors through improved diet and exercise, as well as medications to manage hypertension and hyperlipidemia.
5. Antithrombotic strategy: Includes both antiplatelet agents (aspirin, clopidogrel) and anticoagulation drugs (heparin) in the acute setting.
Diagnostic Biomarkers
1. Troponin significance: Cardiac biomarkers, especially troponin, are key to diagnosing myocardial infarction.
2. NSTEMI vs. unstable angina: Biomarker values help distinguish between these conditions, as only NSTEMI is associated with rising/falling levels of troponin.
3. Biomarker kinetics: Both cardiac troponin I and CK-MB peak within 24 hours of MI and gradually return to normal.
4. Q-wave significance: May indicate the size or location of a current MI, or may indicate a prior MI.
5. ECG evolution: Serial ECGs help observe the evolution of the infarction, providing important diagnostic and prognostic information.
- --
Beyond the Tutorial
Differential Diagnosis for Chest Pain
1. Cardiac causes: Acute coronary syndrome, pericarditis, myocarditis, aortic dissection, Takotsubo cardiomyopathy.
2. Pulmonary causes: Pulmonary embolism, pneumonia, pneumothorax, pleuritis.
3. Gastrointestinal causes: Esophageal spasm, GERD, peptic ulcer, pancreatitis, cholecystitis.
4. Musculoskeletal causes: Costochondritis, rib fracture, thoracic muscle strain.
5. Psychiatric causes: Anxiety, panic attack, somatization disorder.
Guideline-Based Risk Stratification
1. HEART score: Evaluates History, ECG, Age, Risk factors, and Troponin to classify chest pain risk.
2. TIMI score: Predicts 14-day risk of adverse events in patients with NSTEMI/UA.
3. GRACE score: Estimates in-hospital and 6-month mortality risk for ACS patients.
4. CRUSADE score: Estimates bleeding risk in NSTEMI patients undergoing invasive management.
5. High-risk features: Hemodynamic instability, heart failure, recurrent angina, ventricular arrhythmias, mechanical complications.
Advanced Treatment Considerations
1. P2Y12 inhibitor selection: Clopidogrel vs. ticagrelor vs. prasugrel based on patient characteristics and risk.
2. Anticoagulation options: Unfractionated heparin, low molecular weight heparin, fondaparinux, or bivalirudin.
3. Early conservative vs. early invasive strategy: Decision-making for NSTEMI/UA patients based on risk factors.
4. Culprit-only vs. complete revascularization: Strategies for STEMI patients with multivessel disease.
5. Special populations management: Patients with renal dysfunction, elderly, diabetics, and those with bleeding risk.
Post-MI Care
1. Cardiac rehabilitation: Exercise prescription, risk factor modification, psychosocial support.
2. Secondary prevention medications: Optimizing GDMT (guideline-directed medical therapy).
3. Follow-up testing: Role of stress testing, echocardiography, and other imaging modalities.
4. Return to activities: Recommendations for driving, exercise, sexual activity, and work.
5. Depression screening: Recognition and management of post-MI depression, which affects outcomes.
