USMLE/COMLEX 2 - Myocardial Infarction Symptoms, Diagnosis, & Treatment
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 2 CK & COMLEX-USA Level 2 from the Myocardial Infarctions: Diagnosis & Treatment tutorial, focusing on clinical management and treatment decision-making that are essential for these exams. See the tutorial notes for further details and relevant links.
 Below is information not explicitly contained within the tutorial but important for USMLE Step 2 CK & COMLEX Level 2.
Below is information not explicitly contained within the tutorial but important for USMLE Step 2 CK & COMLEX Level 2.
- --
VITAL FOR USMLE/COMLEX 2
Epidemiology & Risk Factors
1. Geographic trends: Incidence of myocardial infarctions is declining in high-income countries but rising in middle- and low-income countries.
2. Demographic patterns: Within the United States, MI incidence after age 35, from highest to lowest: Black males > Black females > White males > White females.
3. Gender differences: First MI occurs approximately 10 years earlier in men than women, possibly related to risk factors such as smoking and hyperlipidemia.
4. Mortality disparities: Despite overall declining rates, mortality remains higher in women than male peers, especially for young and/or minority women.
5. Major modifiable risk factors: Dyslipidemia, diabetes mellitus, hypertension, smoking (including e-cigarettes), obesity, psychosocial stress, alcohol consumption, poor diet (low in fruits and vegetables).
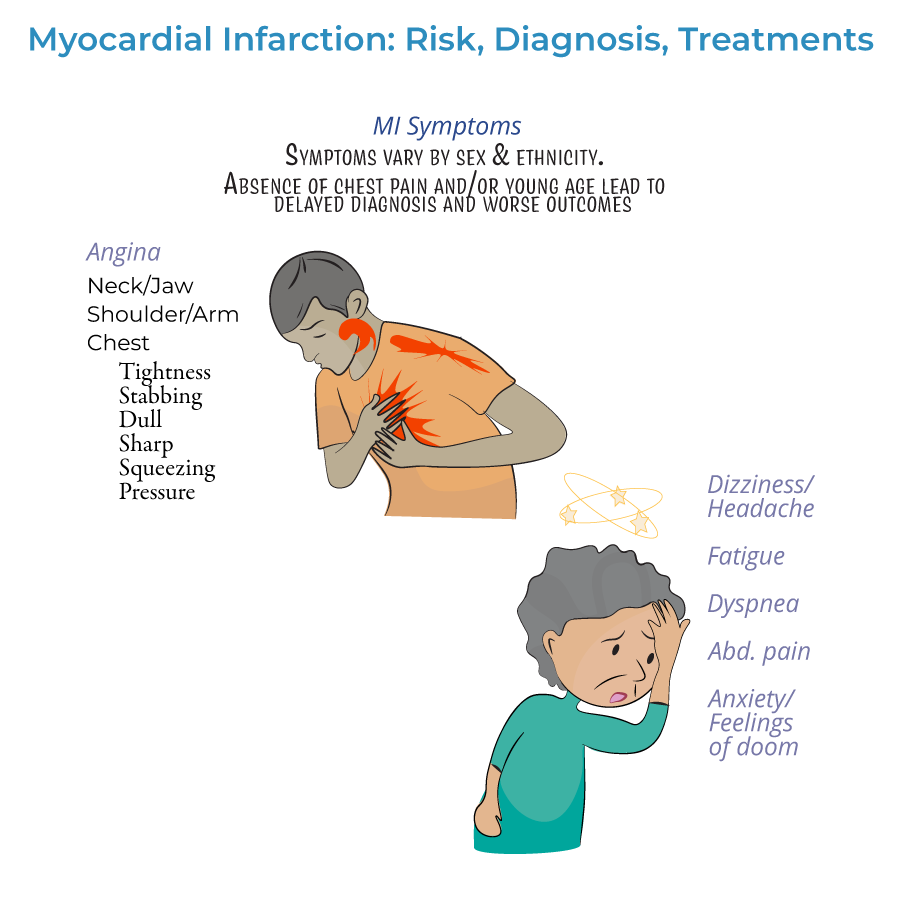
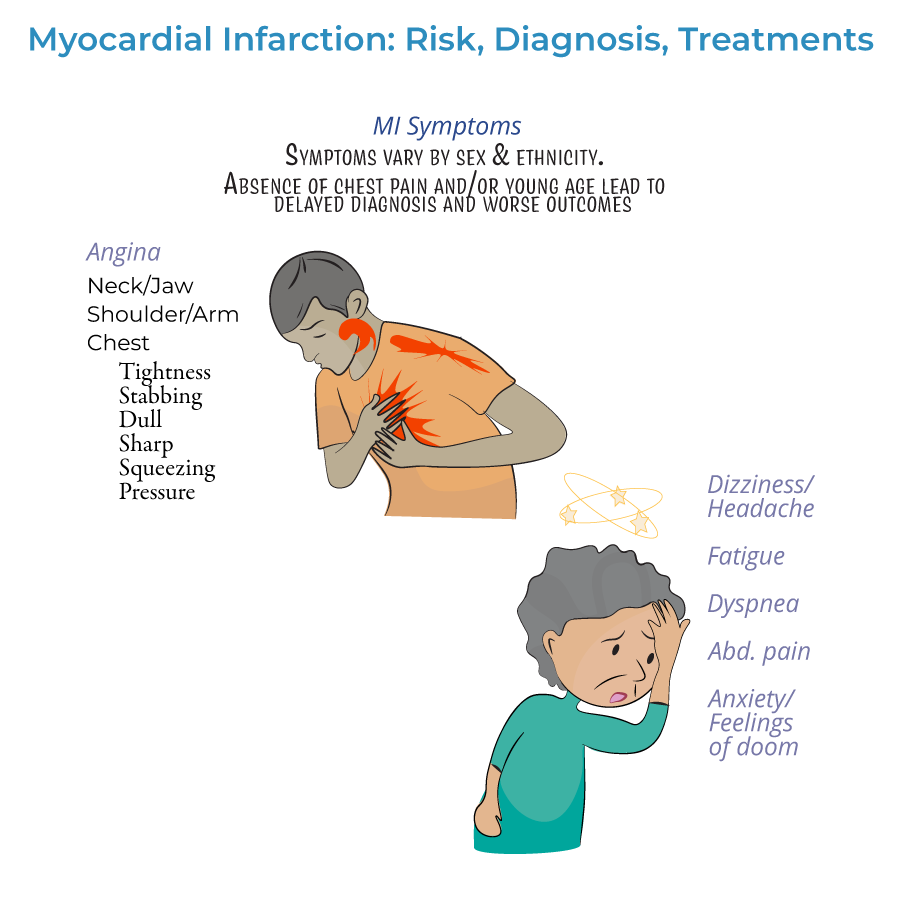
Clinical Presentation & Recognition
1. Presentation patterns:
- Prodromal symptoms: Days, weeks, or months prior to the acute event
- Acute symptoms: Experienced at the time of the event
- Silent MI: No noticeable symptoms
Diagnostic Approach
1. Definition: Myocardial infarction is defined as myocardial injury with ischemia.
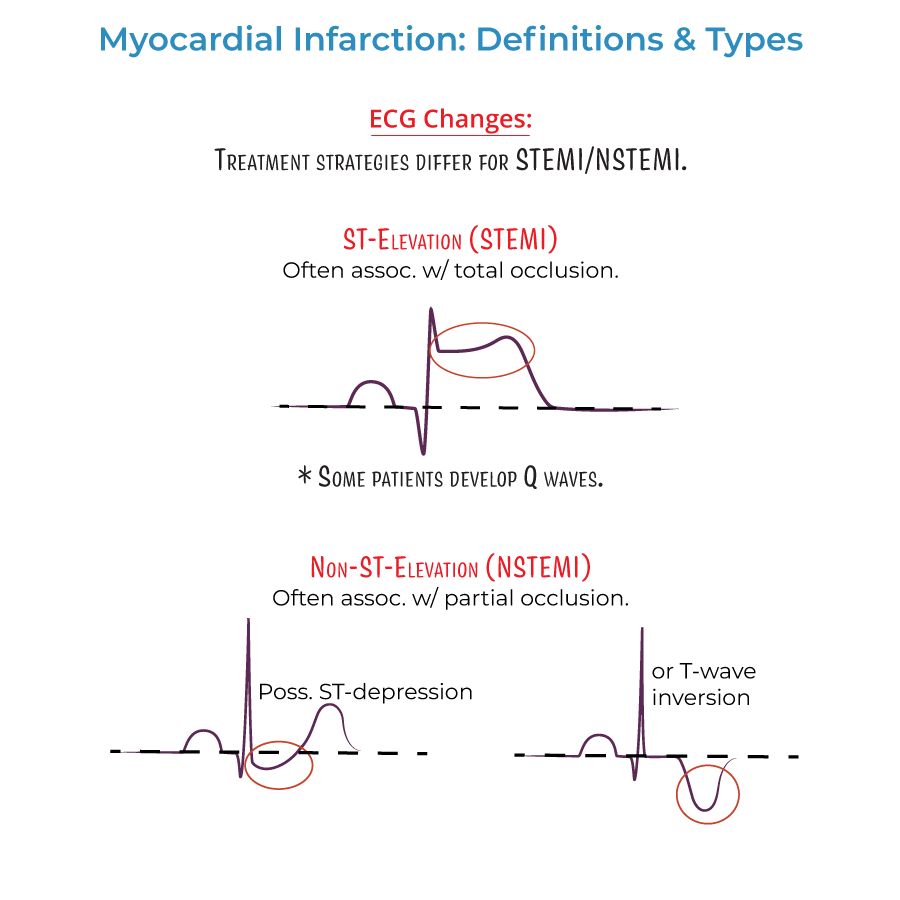
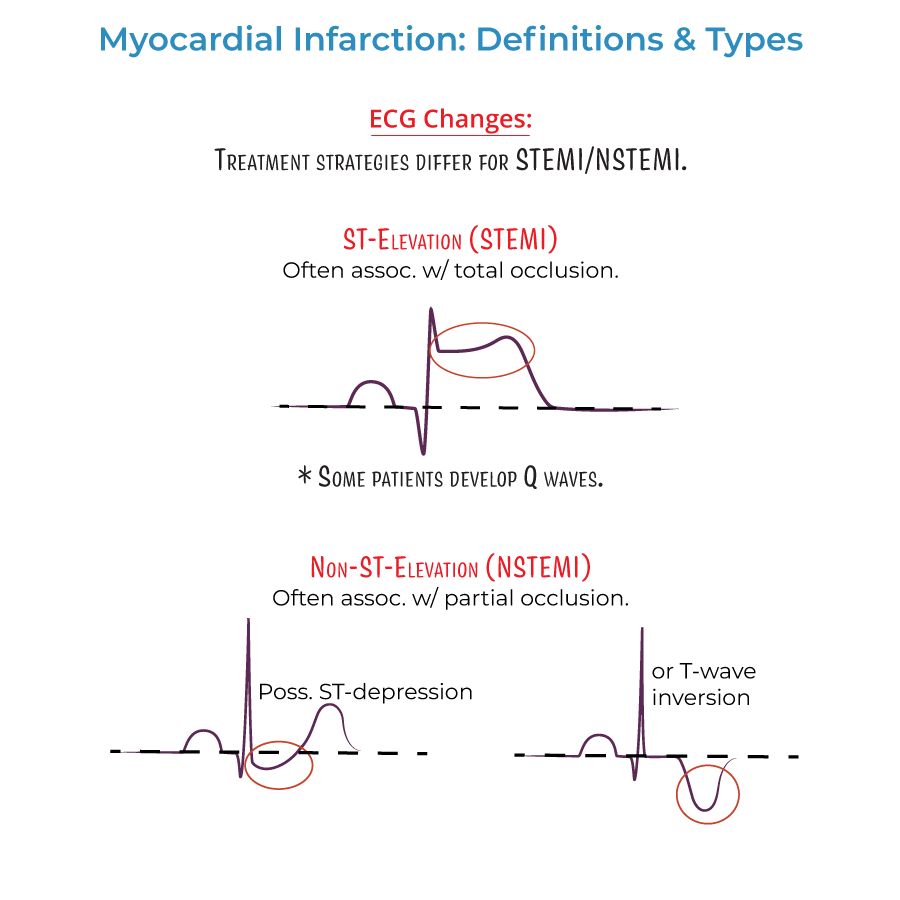
2. ECG timing: Should be administered as soon as possible when MI is suspected, with serial ECGs to observe evolution of the infarction.
3. ECG classification: Distinguishes between ST-segment elevated (STEMI) or Non-ST elevated (NSTEMI) myocardial infarctions, which influences treatment strategies.
4. ECG interpretation:
- Q-wave abnormalities may indicate size/location of current MI or evidence of prior MI
- Lateral infarction: Leads I and aVL; left circumflex artery
- Apical infarction: Leads V5 and V6; left circumflex or right coronary arteries
- Anterior infarction: Leads V3 and V4; left anterior descending artery
- Anteroseptal infarction: Leads V1 and V2; proximal left anterior descending artery
- Inferior infarction: Leads II, aVF, and III; right coronary artery or left circumflex artery (in ~10% with left dominance)
- Right ventricular infarction: Requires additional leads V3R through V6R
- Posterolateral infarction: Requires additional leads V7-V9; right coronary or left circumflex artery
- Cardiac troponin is key to diagnosis
- Help distinguish between NSTEMI (rising/falling troponin) and unstable angina (normal troponin)
- Both cardiac troponin I and CK-MB peak within 24 hours of MI and fall to normal levels over time
Treatment Principles
1. Time-critical approach: Treatment should begin as soon as possible, ideally even before hospital arrival, to reduce the extent of myocardial necrosis.
2. Pre-hospital treatment:
- Oxygen administration when oxygen saturation is less than 90%
- Aspirin for antiplatelet effects
- Nitrates for chest pain (morphine if nitrates ineffective)
- Based on MI classification and severity
- STEMI: Emergency PCI recommended; if unavailable, immediate fibrinolytics
- NSTEMI: Unstable/complicated cases require immediate PCI/CABG; uncomplicated cases may wait longer with possible medical management only
- Fibrinolytics generally not recommended for NSTEMI (risks outweigh benefits)
- Antiplatelets: Aspirin, clopidogrel, or others
- Anticoagulation: Unfractionated or low molecular weight heparin
- Anti-ischemic: Beta-blockers or calcium-channel blockers
- Plaque stabilization: Statins, ACE inhibitors
Prognostic Considerations
1. Disease progression: MI is an important cause of heart failure, which is itself a significant cause of death.
2. Risk factor control: Aggressive modification of modifiable risk factors improves long-term outcomes.
3. Timing of intervention: Earlier reperfusion associated with better myocardial salvage and prognosis.
4. Demographic factors: Higher mortality in women, especially young and/or minority women.
5. Patient education: Awareness of symptoms and risk factors significantly impacts prevention and treatment outcomes.
- --
HIGH YIELD
Clinical Recognition Pearls
1. Atypical presentations: Not all patients experience classic angina—maintain high index of suspicion despite absence of chest pain.
2. Radiation patterns: Pain may radiate from chest to arms, neck, jaw, or back—radiation patterns help confirm diagnosis.
3. Non-cardiac symptoms: Gastrointestinal issues, fatigue, headaches, dizziness, and anxiety may be predominant or only symptoms.
4. Prodromal recognition: Symptoms days to months before acute MI may include fatigue, sleep disturbances, or vague discomfort.
5. Risk of missed diagnosis: Young patients and those without chest pain often experience delayed diagnosis with worse outcomes.
ECG Interpretation Essentials
1. Serial assessment: ECGs should be repeated frequently to observe evolution of infarction patterns.
2. STEMI vs. NSTEMI distinction: Critical treatment decision point based on ECG findings.
3. Lead group interpretation: Different lead sets reflect specific coronary territories:
- Anterior/septal (V1-V4): Left anterior descending artery
- Lateral (I, aVL, V5-V6): Left circumflex artery
- Inferior (II, III, aVF): Right coronary artery or left circumflex
Biomarker Utilization
1. Diagnostic hierarchy: Cardiac troponin is the preferred biomarker for MI diagnosis.
2. Temporal pattern: Both troponin and CK-MB peak within 24 hours of MI onset.
3. Differential diagnosis: Only NSTEMI (not unstable angina) shows rising/falling troponin levels.
4. Serial measurements: More valuable than single determinations for diagnosis.
5. Integration with clinical findings: Always interpret biomarkers within context of symptoms and ECG findings.
Treatment Decision-Making
1. STEMI management: Emergency PCI recommended; if unavailable, immediate fibrinolytic therapy.
2. NSTEMI approach: Risk stratification guides timing of intervention—unstable patients need immediate intervention.
3. Pre-hospital therapy initiation: Early oxygen (when indicated), aspirin, and nitrates can limit infarct size.
4. Fibrinolytic restrictions: Generally not recommended for NSTEMI due to risk/benefit ratio.
5. Comprehensive medication approach: Combination of antiplatelets, anticoagulants, beta-blockers, statins, and ACE inhibitors.
Special Population Considerations
1. Women: Higher mortality rates, more atypical presentations, first MI approximately 10 years later than men.
2. Minority patients: Black males have highest incidence after age 35, followed by Black females.
3. Young patients: Often experience missed or delayed diagnosis due to low clinical suspicion.
4. Elderly: May present with dyspnea or fatigue rather than chest pain.
5. Patient education needs: Many patients, especially women, lack knowledge about risk factors and symptoms—education is crucial.
- --
Beyond the Tutorial
Risk Stratification Tools
1. TIMI Risk Score: Predicts 14-day outcomes in ACS patients.
2. GRACE Risk Score: Predicts in-hospital and 6-month mortality.
3. HEART Score: Stratifies chest pain patients in the emergency department.
4. CRUSADE Score: Assesses bleeding risk in ACS patients.
5. DAPT Score: Guides duration of dual antiplatelet therapy after PCI.
Expanded Treatment Considerations
1. P2Y12 inhibitor selection: Clopidogrel vs. ticagrelor vs. prasugrel based on patient factors.
2. Anticoagulation options: UFH, LMWH, fondaparinux, or bivalirudin based on clinical scenario.
3. Early conservative vs. early invasive strategy: Decision-making for NSTEMI/UA patients.
4. Culprit-only vs. complete revascularization: Strategies for multivessel disease.
5. Optimal timing of intervention: Immediate vs. early vs. delayed based on risk stratification.
Management of Complications
1. Cardiogenic shock: Early recognition, hemodynamic support, and revascularization.
2. Mechanical complications: Diagnosis and management of papillary muscle rupture, ventricular septal defect, free wall rupture.
3. Arrhythmias: Management of post-MI ventricular arrhythmias and conduction disturbances.
4. Right ventricular infarction: Special considerations including volume loading.
5. Heart failure: Recognizing and managing systolic and diastolic dysfunction.
Post-Discharge Management
1. Cardiac rehabilitation: Evidence-based programs improving outcomes.
2. Secondary prevention targets: Goals for lipids, blood pressure, diabetes, and smoking cessation.
3. Medication adherence strategies: Improving compliance with life-saving therapies.
4. Return to activities: Guidance for driving, sexual activity, exercise, and work resumption.
5. Depression screening: Associated with worse outcomes if untreated.
Specific Clinical Scenarios
1. Cocaine-associated MI: Unique management considerations.
2. Perioperative MI: Recognition challenges and management differences.
3. Pregnancy-associated ACS: Management modifications for maternal/fetal safety.
4. Type 2 MI: Supply-demand mismatch without acute plaque rupture.
5. MINOCA (MI with Non-Obstructive Coronary Arteries): Diagnostic approach.
