USMLE/COMLEX 2 - Liver Disease Overview
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 2 & COMLEX-USA Level 2 from the Liver Pathophysiology Overview tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
 Below is information not explicitly contained within the tutorial but important for USMLE & COMLEX 2.
Below is information not explicitly contained within the tutorial but important for USMLE & COMLEX 2.
- --
VITAL FOR USMLE/COMLEX 2
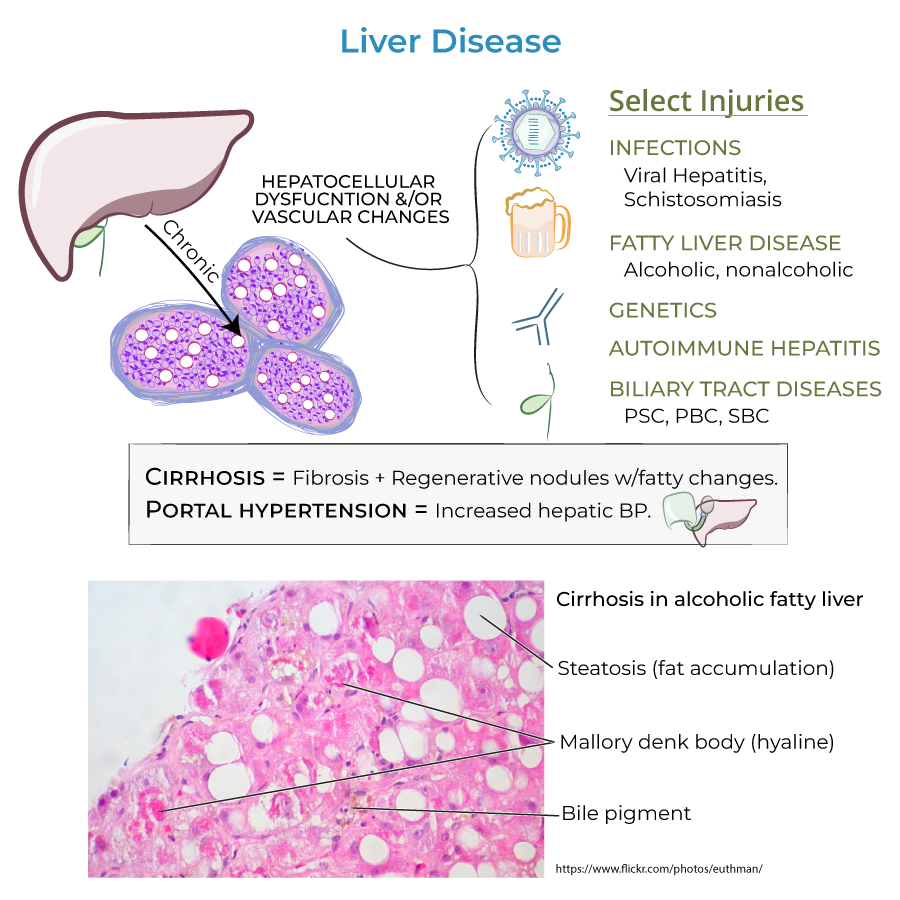
Clinical Presentation of Liver Disease
1. Early vs. Late Disease: Early stages of liver disease are asymptomatic; later stages can present with jaundice, abdominal pain and swelling, edema, dark urine, pale stool, and other signs of liver dysfunction.
2. Diagnosis Importance: Early diagnosis is key for proper treatment, and even reversal, of damage.
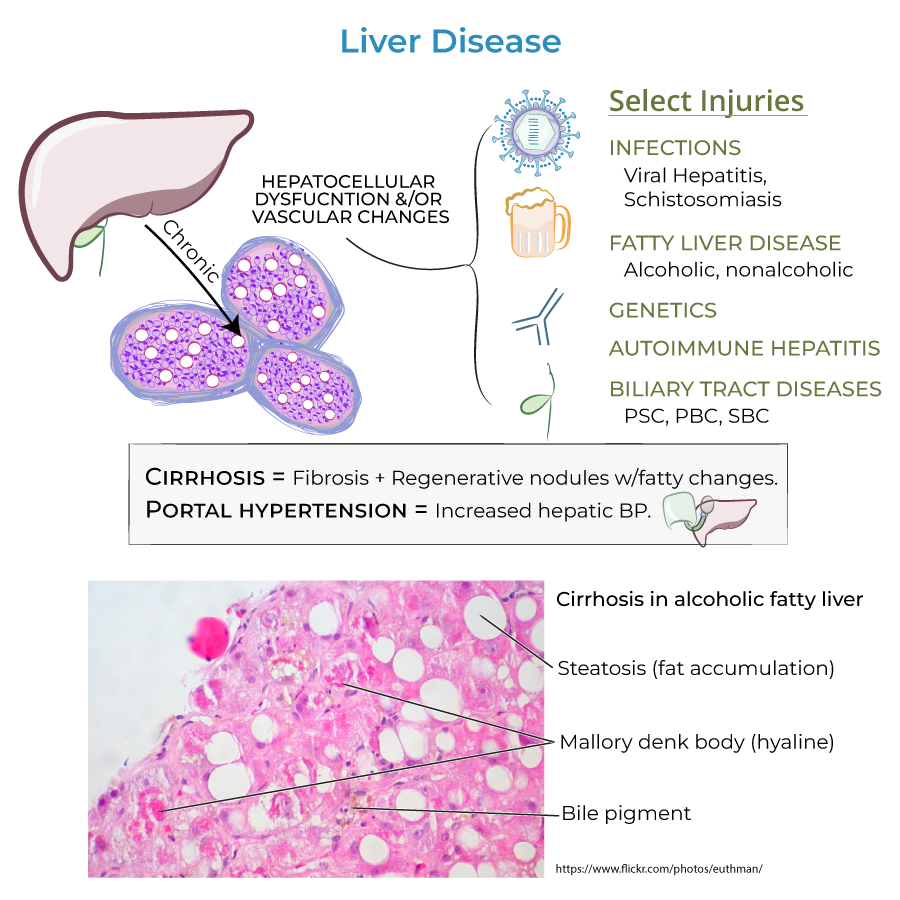
3. Staging Importance: Liver damage is accumulative and progressive, and can be described according to stages from inflammation to liver failure.
4. Reversibility: Newer research indicates that cirrhosis (stage 3) is also reversible, not just stages 1 and 2.
Assessment & Diagnosis
1. Liver Function Grading: The Child-Pugh score is used to grade liver functioning.
2. Transplantation Consideration: In cases of cirrhosis or failure, transplants may be the best option.
Hepatic Encephalopathy
1. Pathophysiology: Result of toxin build-up in the blood; ammonia specifically is thought to be a key culprit.
2. Clinical Finding: Asterixis ("flapping hand tremor" or "liver flap") is the inability for a patient to sustain a posture due to involuntary, brief, "shock-like" movements.
3. Examination Technique: Test by having patient sit with closed eyes, outstretched arms, dorsiflexed wrists, and spread fingers – sudden "flapping" of hands is positive for asterixis.
Portal Hypertension Complications
1. Varices: Collateral blood vessels that form to provide alternative blood flow routes; significant risk for hemorrhage and an important cause of GI bleeding.
2. Ascites: Accumulation of fluid in the peritoneum caused by systemic dilation that allows fluid leakage; a main complication of cirrhosis.
3. Spontaneous Bacterial Peritonitis (SBP): Acute infection resulting from bacteria and endotoxins leaking from the GI tract; can lead to septic shock if not treated promptly.
- --
HIGH YIELD
Systemic Manifestations of Liver Disease
1. Estrogen-Mediated Signs: Elevated estrogen levels can cause spider angiomas (spider-looking collections of blood vessels visible beneath the skin), palmar erythema (reddening of the palms and fingers), and gynecomastia (enlargement of breast tissue in males).
2. Coagulopathy: Results from decreased storage of vitamin K and synthesis of clotting factors.
3. Glucose Abnormalities: Patients can be hyper- or hypoglycemic due to dynamically altered glucose metabolism.
Renal Complications
1. Mechanism: Result of local vasoconstriction (in response to systemic hypotension) and inflammatory processes that reduce filtration.
2. SBP Connection: Spontaneous bacterial peritonitis is often a trigger for renal failure, as it induces release of pro-inflammatory molecules that contribute to renal dysfunction.
Pulmonary Complications
1. Hepatopulmonary Syndrome: Pulmonary vasodilation leads to a ventilation/perfusion mismatch, reduced oxygenation, and hypoxemia.
Bile Flow Complications
1. Clinical Manifestations: Impaired bile flow can lead to hyperlipidemia, jaundice, and malabsorption of GI contents.
Liver Cancer Risk
1. Progression: Increased risk of liver cancer in advanced liver disease.
- --
Beyond the Tutorial
Clinical Management Approaches
1. Ascites Management: Sodium restriction (2g/day), diuretics (spironolactone ± furosemide), therapeutic paracentesis for refractory cases.
2. Variceal Bleeding: Acute management with vasoactive drugs (octreotide), endoscopic band ligation, and antibiotic prophylaxis.
3. Hepatic Encephalopathy: Lactulose, rifaximin, and addressing precipitating factors (GI bleeding, infection, medications, electrolyte imbalances).
4. SBP Prophylaxis: Indicated in patients with prior SBP, ascites with low protein, or variceal bleeding.
Advanced Clinical Assessment
1. MELD Score: Model for End-Stage Liver Disease used for transplant prioritization based on bilirubin, INR, creatinine, and sodium.
2. Differential Diagnosis: Distinguishing between acute liver failure, acute-on-chronic liver failure, and decompensated cirrhosis.
3. HCC Surveillance: 6-monthly ultrasound with or without alpha-fetoprotein in cirrhotic patients.
Special Considerations
1. Medication Dosing: Dosage adjustments for hepatically metabolized drugs based on Child-Pugh classification.
2. Procedural Risks: Increased bleeding risk, infection risk, and sedation complications in advanced liver disease.
3. Nutrition Management: Adequate protein intake (contrary to older practices of restriction), BCAA supplementation in encephalopathy, addressing malnutrition.
4. Pregnancy Considerations: Differential diagnosis of liver disease unique to pregnancy (HELLP, acute fatty liver, intrahepatic cholestasis).
Emerging Therapies
1. Antifibrotic Agents: Targeting hepatic stellate cell activation and collagen deposition.
2. Novel Encephalopathy Treatments: Ammonia scavengers, probiotics, and fecal microbiota transplantation.
3. Artificial Liver Support: Bioartificial systems, albumin dialysis, and molecular adsorbent recirculating systems as bridges to transplantation.
4. Precision Medicine Approaches: Genotype-directed therapy for specific liver diseases (e.g., HCV, NAFLD, AIH).
