USMLE/COMLEX 2 - Jaundice
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 2 & COMLEX-USA Level 2 from the Jaundice tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
 Below is information not explicitly contained within the tutorial but important for USMLE & COMLEX 2.
Below is information not explicitly contained within the tutorial but important for USMLE & COMLEX 2.
- --
VITAL FOR USMLE/COMLEX 2
Clinical Presentation & Diagnosis
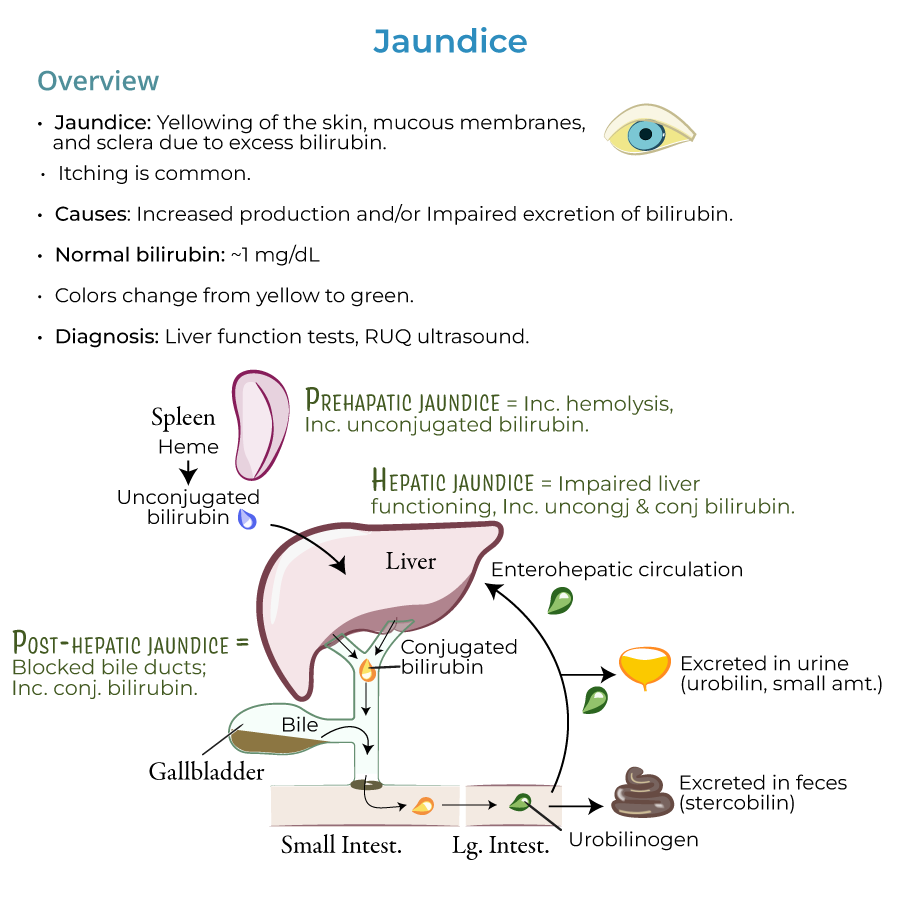
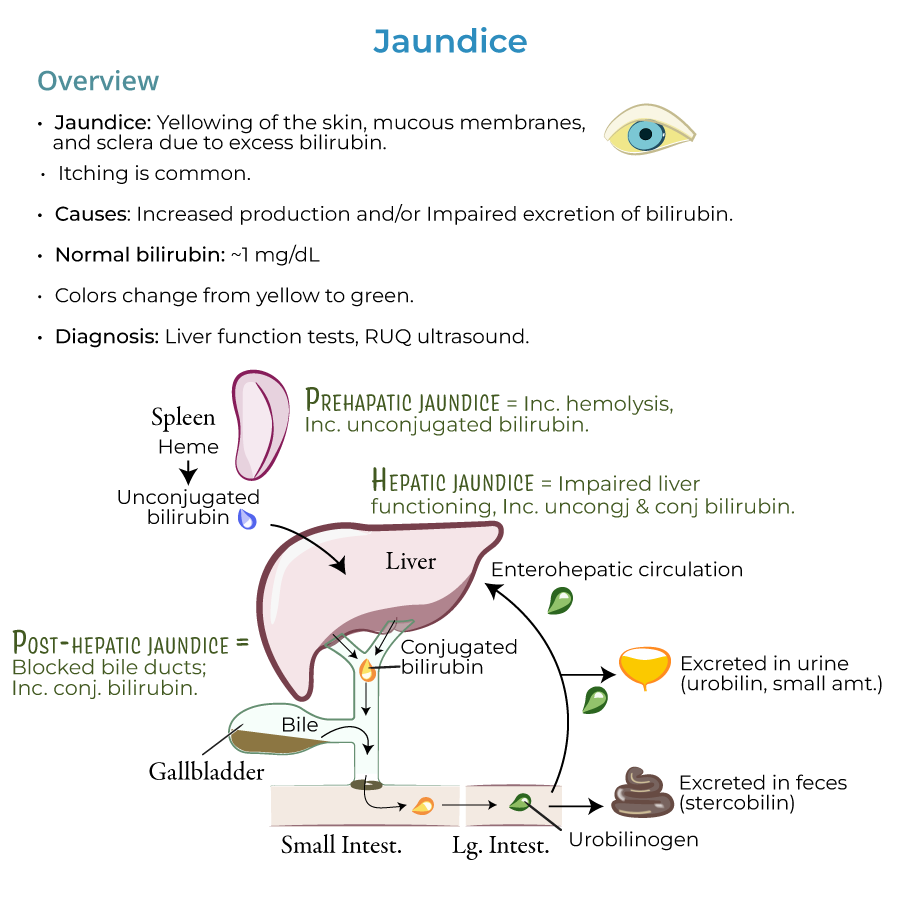
1. Clinical signs: Jaundice presents as yellowing of the skin, mucous membranes, and sclera due to excess bilirubin; itching is also common.
2. Diagnostic threshold: Normal bilirubin values are approximately 1 mg/dL; jaundice is usually present when levels are 2.5 mg/dL and higher.
3. Color progression: As bilirubin accumulates, jaundice can progress from a yellowish to greenish color.
4. Key diagnostic approach: Jaundice is a sign of an underlying disorder, so we need to investigate its causes to find the appropriate treatment.
5. Diagnostic tests: We use liver function tests and, when biliary obstruction is suspected, right upper quadrant ultrasound to discover and treat the origins of jaundice.
Essential Clinical Correlations
1. Demographic considerations: Jaundice is most common in newborns and the elderly due to impaired conjugation in the liver and/or excretion.
2. Clinical mnemonic: HOT Liver – Hemolysis, Obstruction, Tumors, and Liver diseases – captures the main etiologies.
3. Distinguishing types:
- Indirect hyperbilirubinemia: No bilirubin in urine (unconjugated is not water soluble)
- Direct hyperbilirubinemia: Dark urine (conjugated bilirubin is water soluble and appears in urine)
- Cholestasis: Pale, chalky-colored feces (absence of stercobilin)
- --
HIGH YIELD
Pre-hepatic Jaundice (Hemolysis)
1. Key clinical findings: Elevated unconjugated bilirubin without bilirubin in urine.
2. Important causes to recognize:
- Sickle cell anemia and G6PD deficiency - elevated hemolysis is a top cause of jaundice
- Thalassemia and pernicious anemia (inefficient erythropoiesis)
- Massive blood transfusions and hematoma resorption (increased bilirubin production)
Obstructive (Post-hepatic) Jaundice
1. Key clinical findings: Dark urine, pale stools, and direct hyperbilirubinemia.
2. Common obstructive causes:
- Gallstone obstruction in gallbladder (cholelithiasis) or bile duct (choledocholithiasis)
- Biliary system inflammation, atresia, or strictures that narrow the ductal system
- Ductal compression from pancreatic cancer, other tumors, or pancreatitis
Hepatocellular Jaundice
1. Clinical presentation: Mixed hyperbilirubinemia with abnormal liver function tests.
2. Key hepatocellular causes:
- Viral hepatitis, alcoholic hepatitis, autoimmune hepatitis, and nonalcoholic steatohepatitis
- Other viral infections: Yellow fever ("yellow" because of the jaundice), EBV, CMV, and HSV
- Cirrhosis and Wilson's disease
- Drug-induced: estrogen, acetaminophen, and arsenic
Genetic Disorders Presenting with Jaundice
1. Gilbert syndrome: Mild, intermittent symptoms from UDP-glucuronosyltransferase deficiency.
2. Crigler-Najjar syndrome: Can be mild or severe; Type 1 has risk of kernicterus (brain damage).
3. Dubin-Johnson syndrome: Often asymptomatic, defects in bilirubin secretion.
4. Rotor syndrome: Generally benign and self-limiting, defects in bile storage.
Neonatal Jaundice Management
1. Physiologic jaundice: Common and generally benign due to immature hepatic conjugation; resolves in weeks.
2. Breast milk jaundice: Benign form lasting 3-12 weeks, resolves on its own.
3. Breastfeeding jaundice: Occurs with insufficient breastmilk intake; may require supplementation.
4. Critical management point: Must monitor and treat bilirubin excess promptly as newborns are particularly susceptible to kernicterus.
5. Differential diagnosis: Need to rule out congenital and hemolytic disorders, such as G6PD deficiency.
Special Clinical Scenarios
1. Intrahepatic cholestasis of pregnancy: Monitor carefully as a cause of jaundice in pregnant women.
2. Infiltrative disorders: Consider amyloidosis, lymphoma, sarcoidosis, and tuberculosis in differential.
3. Sepsis-associated jaundice: Important to recognize in critically ill patients.
4. Total parenteral nutrition: Can cause intrahepatic cholestasis in hospitalized patients.
- --
Beyond the Tutorial
Clinical Approach to Jaundice
1. History findings: Focus on medication use, alcohol consumption, recent blood transfusions, family history, travel history, and risk factors for viral hepatitis.
2. Physical exam pearls: Look for hepatomegaly, splenomegaly, ascites, spider angiomata, palmar erythema, and caput medusae in cirrhosis.
3. Murphy's sign: Right upper quadrant pain on inspiration during palpation suggests acute cholecystitis.
4. Courvoisier's sign: Painless jaundice with palpable gallbladder suggests pancreatic head carcinoma.
5. Charcot's triad: Fever, jaundice, and right upper quadrant pain suggesting ascending cholangitis (medical emergency).
Diagnostic Workup Algorithm
1. First-line labs: Complete blood count, comprehensive metabolic panel, coagulation studies, and fractionated bilirubin.
2. Hepatocellular pattern: ↑ALT/AST out of proportion to alkaline phosphatase (>5:1 ratio).
3. Cholestatic pattern: ↑Alkaline phosphatase, GGT out of proportion to ALT/AST (<2:1 ratio).
4. Imaging progression: Start with ultrasound; if inconclusive, proceed to MRCP, ERCP, or liver biopsy based on suspected etiology.
5. Non-invasive fibrosis assessment: FibroScan (transient elastography) to evaluate liver stiffness without biopsy.
Management Principles
1. Acute viral hepatitis: Supportive care, avoid hepatotoxins, monitor for fulminant failure (INR > 1.5, encephalopathy).
2. Obstructive jaundice: ERCP with stone removal or stent placement for malignant obstruction.
3. Drug-induced liver injury: Immediately discontinue offending agent; N-acetylcysteine for acetaminophen toxicity.
4. Alcoholic hepatitis: Severe cases (Maddrey's discriminant function >32) may benefit from corticosteroids or pentoxifylline.
5. Autoimmune hepatitis: Corticosteroids and azathioprine are mainstays of therapy.
Neonatal Jaundice Management
1. Nomograms: Use hour-specific bilirubin nomograms (Bhutani curves) to guide intervention.
2. Phototherapy thresholds: Based on age in hours, risk factors, and total serum bilirubin levels.
3. Exchange transfusion: Reserved for severe cases not responding to phototherapy or with bilirubin toxicity signs.
4. IVIG: Consider for isoimmune hemolytic disease to reduce need for exchange transfusion.
5. Follow-up: All infants with severe jaundice require neurodevelopmental follow-up to monitor for kernicterus sequelae.
Special Therapeutic Considerations
1. Primary biliary cholangitis: Ursodeoxycholic acid improves biochemical markers and delays progression.
2. Primary sclerosing cholangitis: Manage dominant strictures with ERCP dilation; no proven medical therapy.
3. Wilson's disease: D-penicillamine or trientine with zinc for copper chelation.
4. Pregnant patients: Ursodeoxycholic acid for intrahepatic cholestasis; early delivery if severe.
5. Hereditary syndromes: Phenobarbital may reduce bilirubin in Crigler-Najjar type II by inducing UGT1A1 enzyme.
