USMLE/COMLEX 2 - Ischemic Heart Disease Symptoms and Treatments
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 2 & COMLEX-USA Level 2 from the Ischemic Heart Disease Symptoms and Treatments tutorial, as well as points of interest at the end that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
 Below is information not explicitly contained within the tutorial but important for USMLE & COMLEX 2.
Below is information not explicitly contained within the tutorial but important for USMLE & COMLEX 2.
- --
VITAL FOR USMLE/COMLEX 2
Clinical Presentation of Ischemic Heart Disease
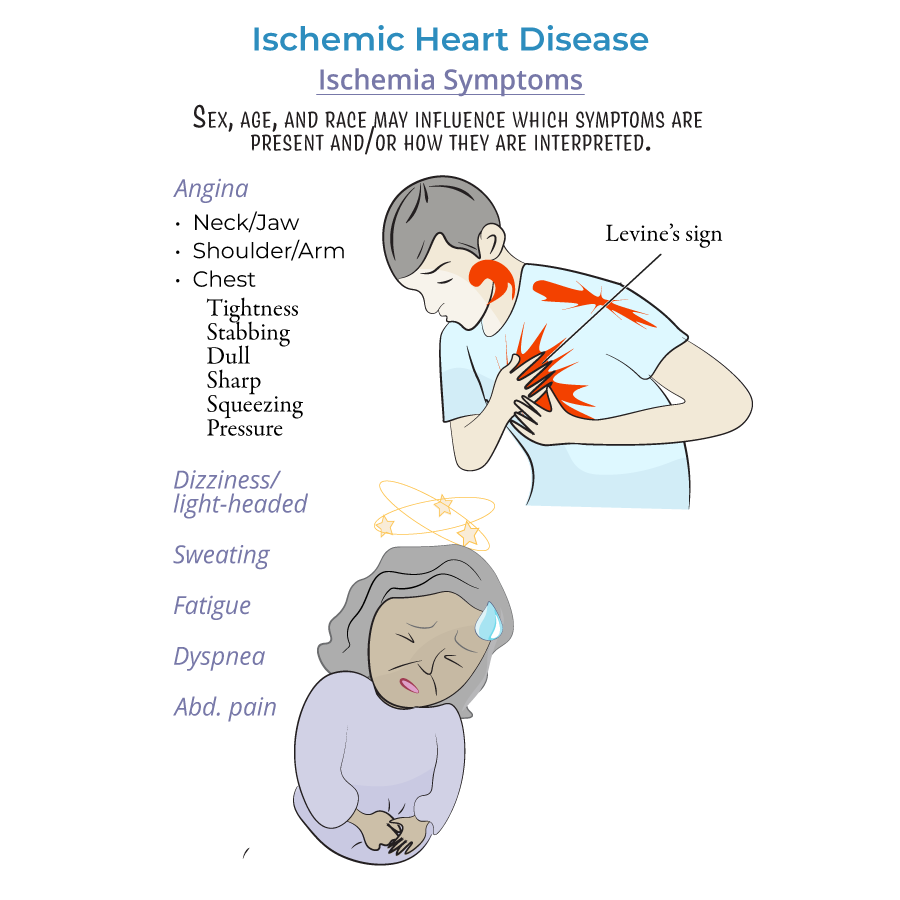
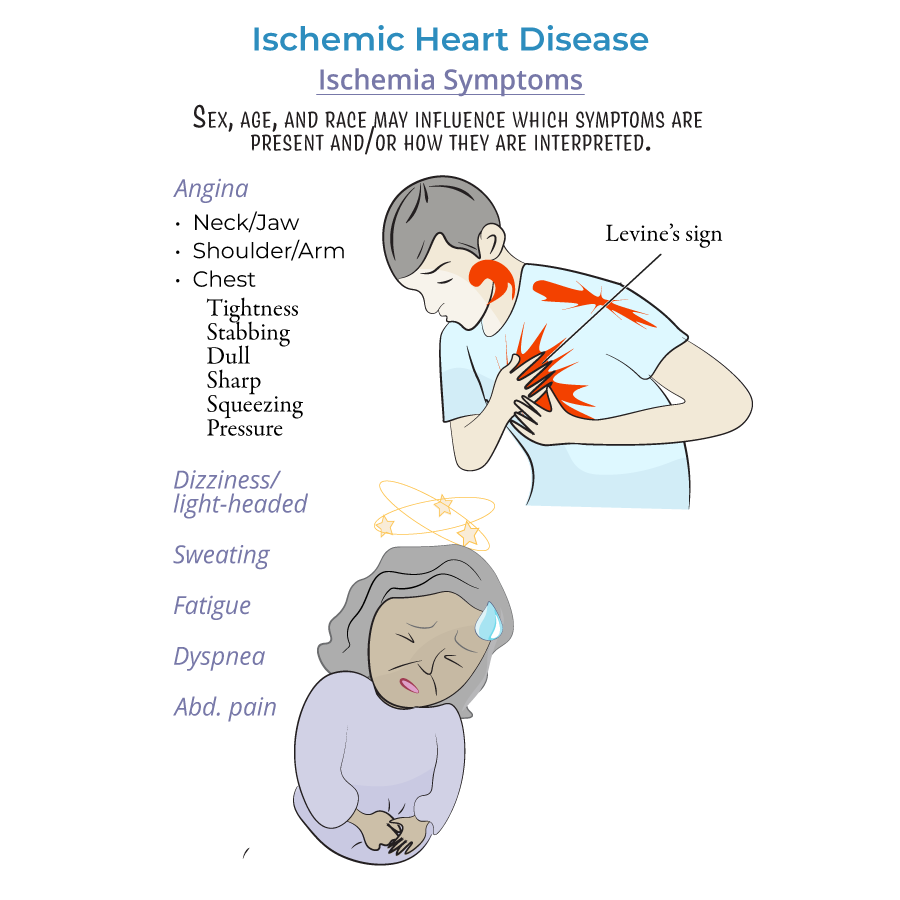
1. Angina pectoris is the hallmark presentation; characterized by chest pain/discomfort radiating to upper extremities, face, with variable presentation based on sex, age, and race.
2. Stable angina presents with predictable triggers, duration, and frequency; resolves with rest and/or nitrates.
3. Unstable angina is unpredictable, doesn't respond to rest/medications, and represents an acute coronary syndrome requiring immediate intervention.
4. Must differentiate from non-ischemic causes of angina: aortic stenosis, anemia, arrhythmias, and hypertrophic cardiomyopathy.
5. Atypical angina and angina equivalents include fatigue and other symptoms that may not include classic chest pain.
Angina Classification and Management
1. Stable angina: Triggered by exertion, resolves with rest/nitrates; requires risk stratification and medical therapy.
2. Unstable angina: Form of acute coronary syndrome, requires emergency evaluation and intervention to prevent myocardial infarction.
3. Vasospastic angina: Occurs spontaneously (typically at night/early morning); most common in women and smokers; responds to nitrates and calcium-channel blockers.
4. Microvascular angina: Accounts for chest pain in up to half of patients without obstructive coronary disease; may respond less well to nitrates.
- --
HIGH YIELD
Clinical Assessment and Diagnosis
1. Levine's sign (clenched fist over sternum) is a characteristic gesture patients use to describe angina.
2. Radiating discomfort to shoulders, arms, neck, and jaw is a key clinical feature requiring evaluation.
3. Gastrointestinal symptoms more common in patients of African descent and may be misinterpreted as indigestion.
4. Women more commonly present with light-headedness, dizziness, and persistent fatigue rather than classic chest pain.
5. Dyspnea and diaphoresis are important associated symptoms that may indicate severity.
6. Diagnostic workup includes ECG, echocardiogram, stress testing, angiograms, and CT scans.
Treatment Strategies
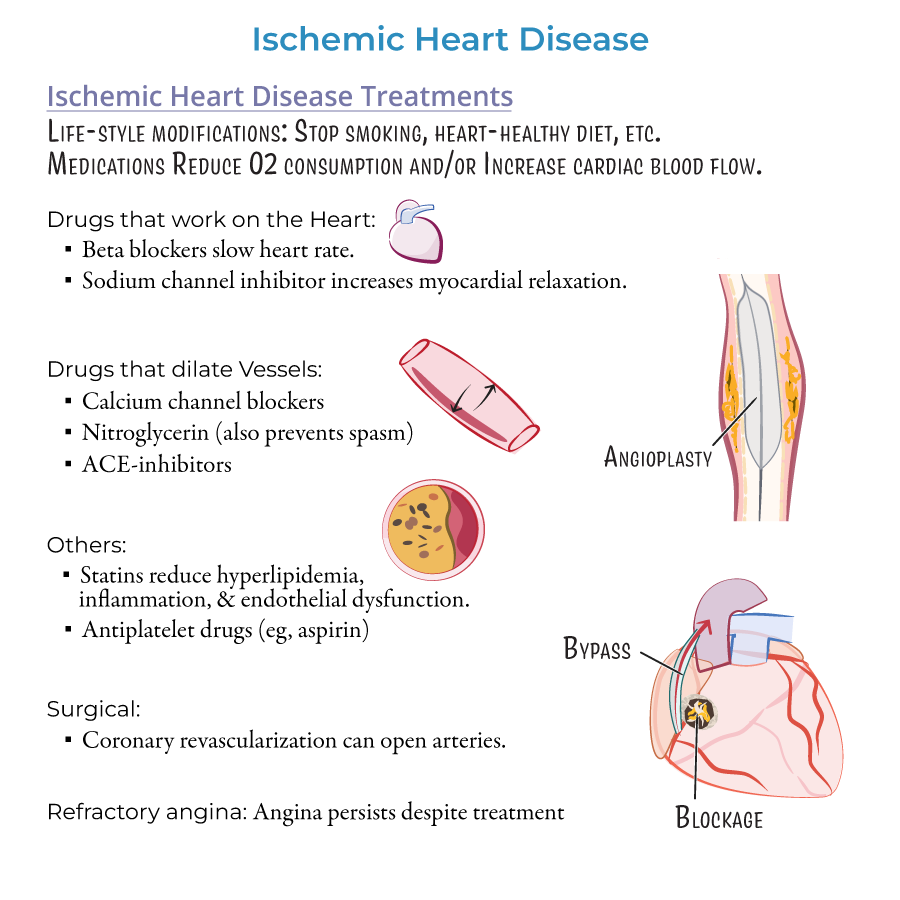
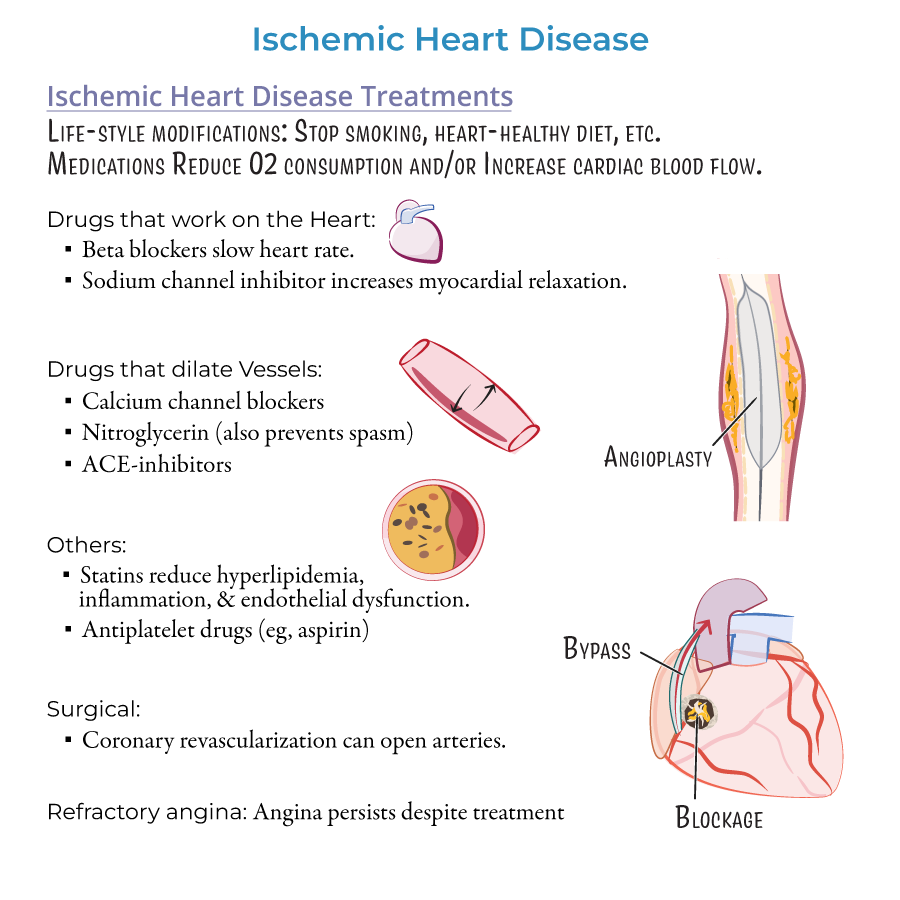
1. Medical management includes combination of lifestyle modifications and pharmacotherapy.
2. Nitroglycerin for acute relief and prophylaxis; dilates vessels and prevents spasms.
3. Beta-blockers reduce oxygen demand by slowing heart rate; contraindicated in vasospastic angina.
4. Calcium channel blockers effective for vasospastic angina by promoting vessel dilation.
5. Ranolazine (sodium channel inhibitor) increases myocardial relaxation, reducing oxygen demand.
6. ACE-inhibitors provide vessel dilation and cardiovascular risk reduction.
7. Statins target multiple mechanisms: reduce hyperlipidemia, vessel inflammation, and endothelial dysfunction.
8. Aspirin therapy requires balancing antithrombotic benefit against bleeding risk.
9. Revascularization options:
- Percutaneous coronary intervention (angioplasty) with possible stent placement
- Coronary artery bypass grafting (CABG) using saphenous vein, radial artery, or left internal mammary artery
- --
Beyond the Tutorial
Advanced Management Considerations
1. HEART score is a clinical decision tool for risk stratification in acute chest pain.
2. High-sensitivity troponin assays have changed the evaluation timeline for possible ACS.
3. Optimal medical therapy (OMT) should be maximized before pursuing elective revascularization.
4. Fractional flow reserve (FFR) guides intervention decisions for intermediate coronary lesions.
Special Populations
1. Diabetes mellitus patients require more aggressive evaluation and treatment of suspected CAD.
2. Chronic kidney disease complicates contrast administration for diagnostic procedures.
3. Pregnancy-associated ACS requires specialized management approaches.
4. Post-PCI anti-platelet therapy duration varies based on stent type, patient risk factors, and bleeding risk.
