USMLE/COMLEX 2 - Ischemic Heart Disease Pathophysiology
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 2 & COMLEX-USA Level 2 from the Ischemic Heart Disease tutorial, as well as points of interest at the end that are not directly addressed in this tutorial but should help you prepare for the boards.
 2. Plaque erosion:
2. Plaque erosion:
 Below is additional information important for USMLE Step 2 CK not explicitly contained within the tutorial.
Below is additional information important for USMLE Step 2 CK not explicitly contained within the tutorial.
- --
VITAL FOR USMLE STEP 2
Acute Coronary Syndrome: Clinical Framework
1. Definition: Umbrella term for events resulting from sudden cardiac ischemia.
2. Includes: Unstable angina, myocardial infarction, and sudden cardiac death.
3. Epidemiology: Leading cause of death in both men and women.
4. Sex-based differences: May delay diagnosis and treatment, particularly in women.
Key Risk Factor Assessment
1. Traditional factors: Family history, age, smoking, hypertension, diabetes, hyperlipidemia, obesity.
2. Sex-specific factors: Early menopause, gestational diabetes, gestational hypertension.
3. Additional considerations: Chronic inflammatory rheumatoid diseases.
4. Clinical note: Several risk factors are stronger predictors in women than men.
Pathophysiologic Models for Clinical Reasoning
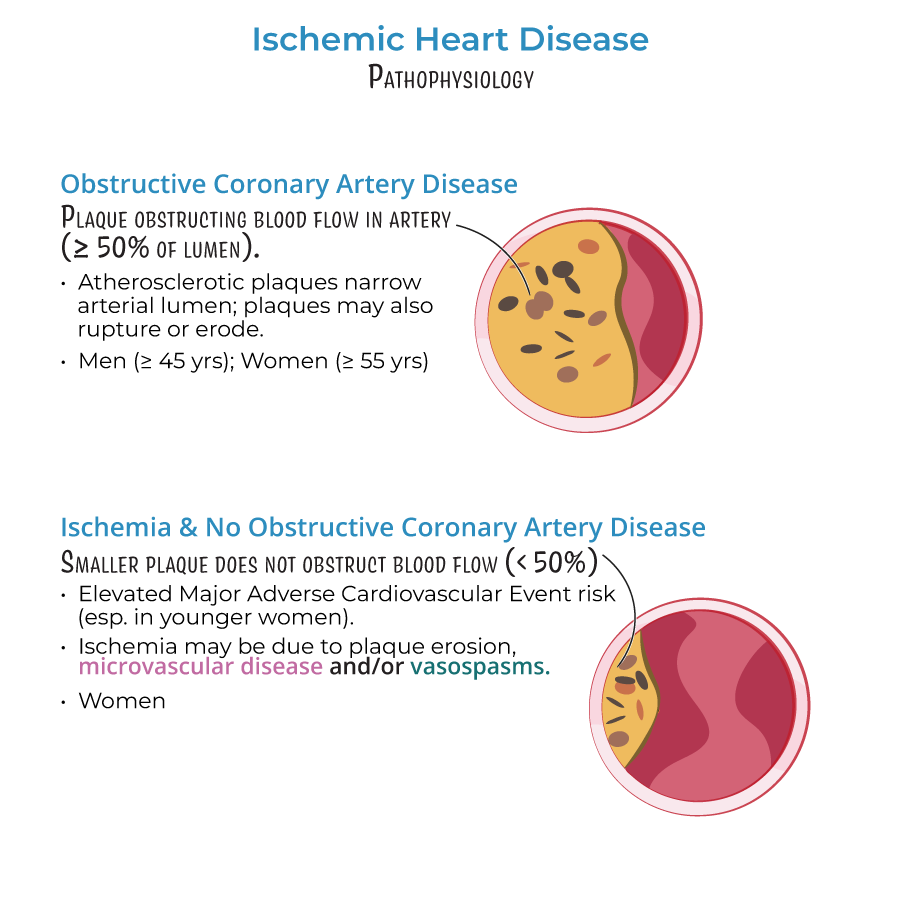
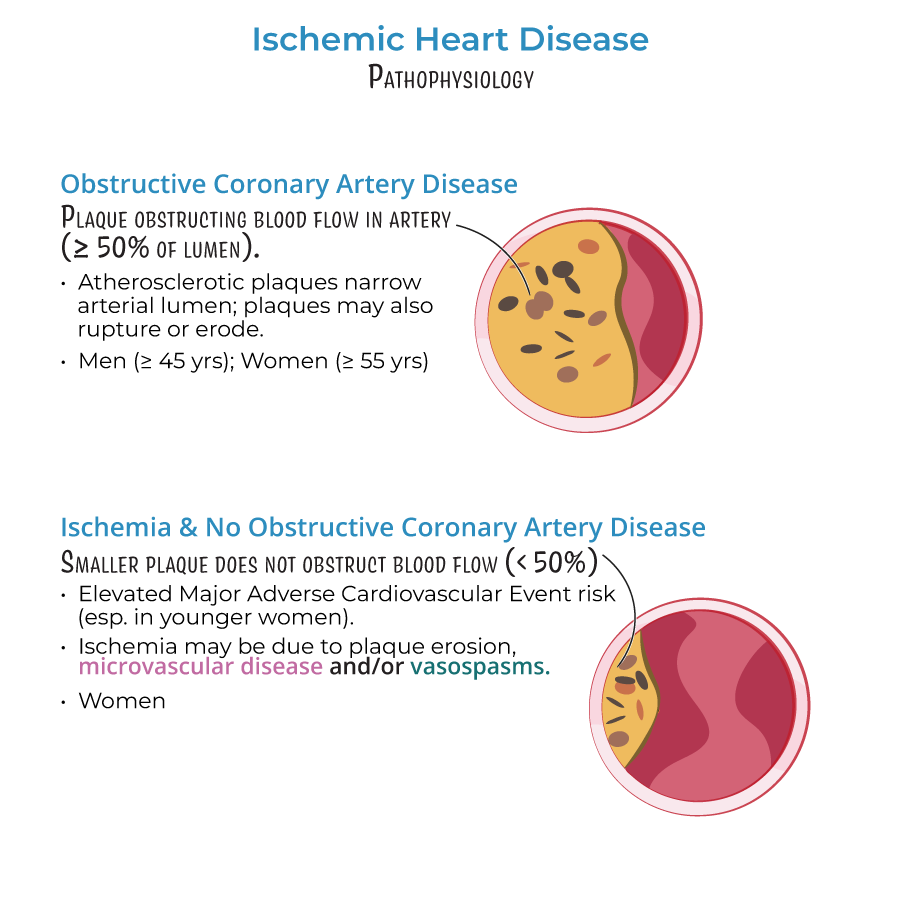
1. Obstructive CAD (≥50% stenosis):
- Demographics: Primarily men >45 years, women >55 years
- Presentation: Classic exertional symptoms, positive stress tests
- Diagnostic approach: Standard coronary angiography typically positive
- Demographics: More common in women, present in ~30% of men
- Clinical significance: Associated with elevated MACE (Major Adverse Cardiovascular Events)
- Diagnostic challenge: Normal or near-normal coronary angiograms despite symptoms
- Key fact: Formerly thought benign but now recognized as clinically important
- Up to 50% of symptomatic patients have no significant coronary obstruction
- Absence of obstruction does not rule out ischemic heart disease
- Further investigation warranted in symptomatic patients with negative angiograms
- --
HIGH YIELD
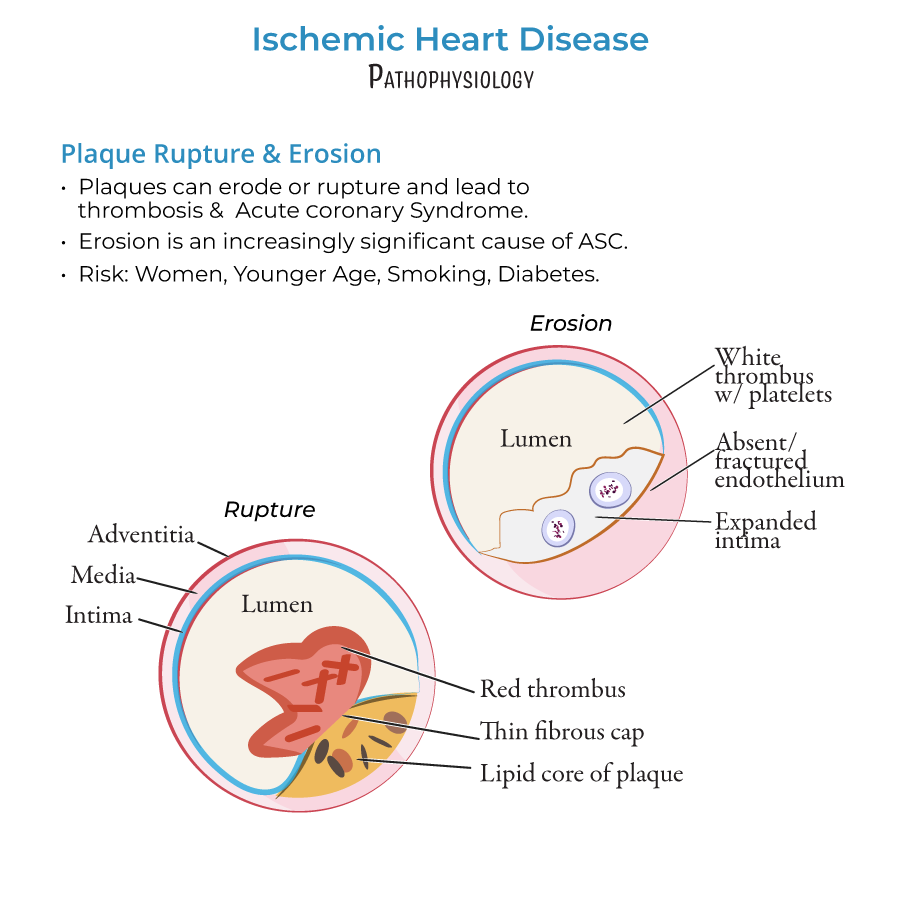
Mechanisms of Plaque Complications
1. Plaque rupture:
- Characteristics: Lipid cores, thin fibrous caps
- Result: Fibrin-rich "red thrombi"
- Trend: Decreasing in frequency due to better lipid management (statins)
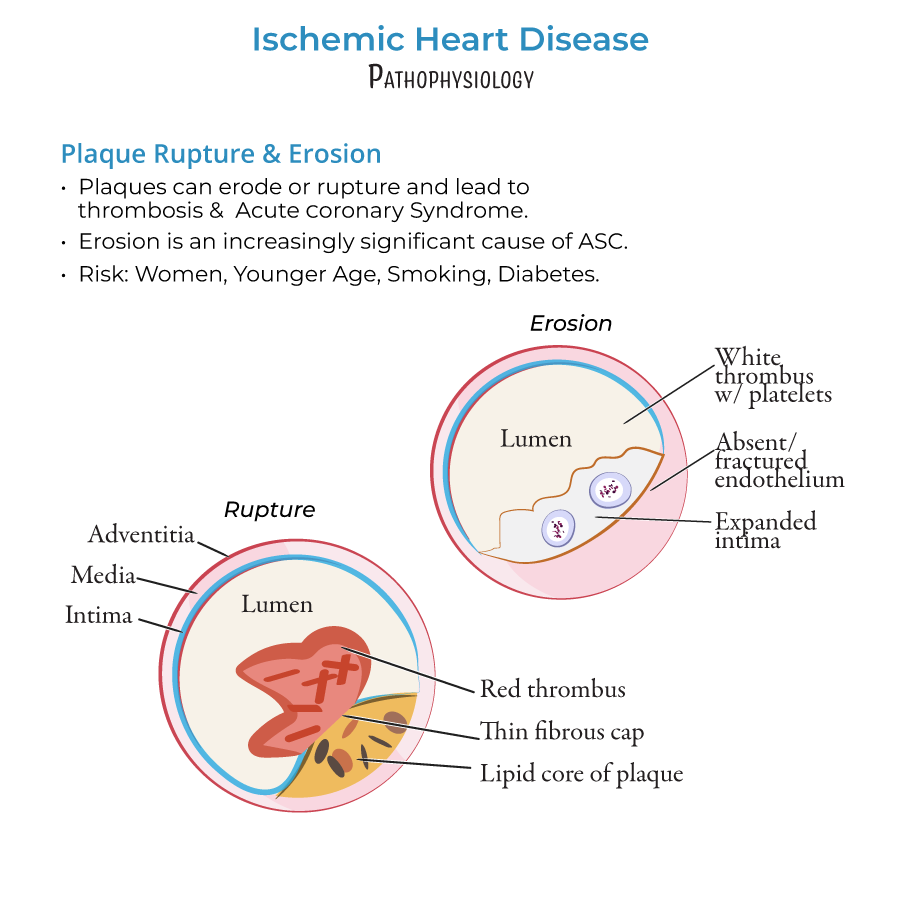 2. Plaque erosion:
2. Plaque erosion:
- Demographics: More common in women, young patients, smokers, diabetics
- Characteristics: Thick cap plaques with endothelial dysfunction/absence
- Result: Platelet-rich "white thrombi"
- Trend: Increasing clinical significance despite lipid-lowering therapies
Coronary Microvascular Dysfunction (CMD)
1. Epidemiology: Affects both sexes nearly equally (contrary to earlier studies)
2. Clinical significance: Elevated MACE risk, often missed in conventional assessment
3. Mechanisms:
- Structural: Arteriole remodeling affecting wall:lumen ratio
- Functional: Impaired vasodilation, often endothelial dysfunction
- Pattern of ischemia: Diffuse and patchy (vs. focal with epicardial obstruction)
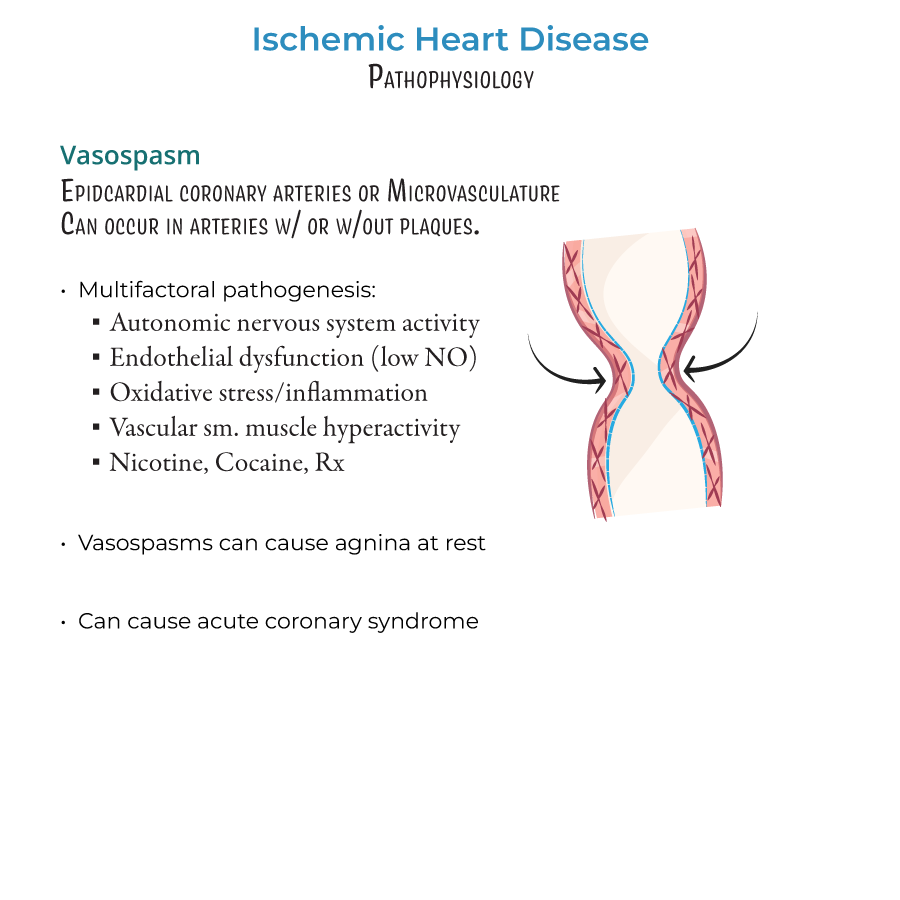
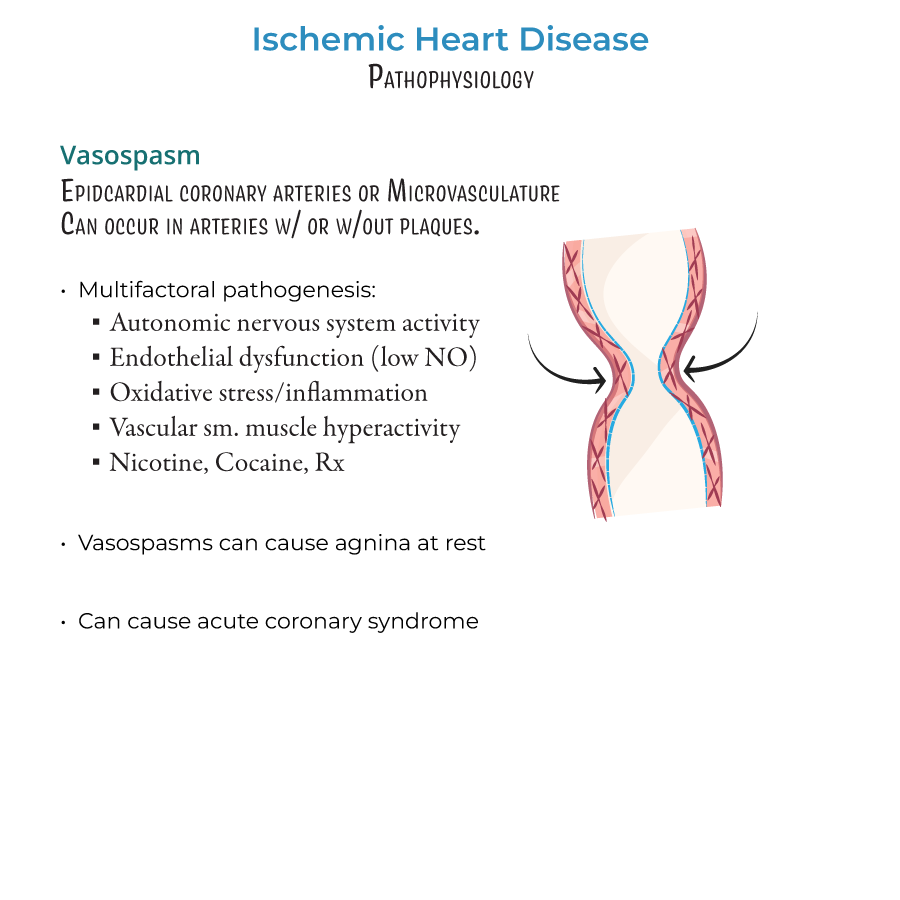
Vasospasm: Clinical Considerations
1. Location: Both epicardial and microvascular vessels
2. Context: Can occur with or without underlying stenosis
3. Triggers/mechanisms:
- Autonomic nervous system dysregulation
- Endothelial dysfunction (especially NO deficiency)
- Oxidative stress and inflammation
- Vascular smooth muscle hyperactivity
- Exogenous substances: nicotine, cocaine, vasoconstricting medications
Diagnostic Approach to Ischemic Syndromes
1. Clinical presentation patterns:
- Classic exertional symptoms: Consider obstructive CAD
- Atypical symptoms: Consider INOCA, CMD, vasospasm
- Rest symptoms: Consider vasospasm, unstable disease
- Normal angiogram does not rule out ischemia
- Further assessment needed for suspected microvascular or vasospastic disease
- --
Beyond the Tutorial
Detailed Clinical Presentation and Assessment
1. Symptom patterns:
- Typical angina: Substernal pressure/discomfort, exertional, relieved by rest/nitroglycerin
- Atypical presentations: More common in women, elderly, diabetics (fatigue, dyspnea, epigastric discomfort)
- Unstable patterns: Crescendo angina, new-onset severe angina, rest angina
- Equivalent symptoms: Exertional dyspnea, diaphoresis, nausea/vomiting, arm/jaw pain
- Often normal in stable disease
- May include S4, transient murmurs (papillary muscle dysfunction), signs of heart failure
- Xanthelasma, xanthomas suggest familial hyperlipidemia
- Assess for peripheral vascular disease
- ECG: ST-segment changes, T-wave inversions, Q waves
- Cardiac biomarkers: High-sensitivity troponin (serial measurements)
- Imaging: Echocardiography for wall motion abnormalities
- Risk stratification tools: TIMI, GRACE scores for ACS
Management Approaches
1. Acute interventions:
- MONA: Morphine, Oxygen (if hypoxic), Nitroglycerin, Aspirin
- Antiplatelet therapy: DAPT (aspirin + P2Y12 inhibitor)
- Anticoagulation: UFH, LMWH, fondaparinux
- Early invasive strategy vs. conservative approach based on risk
- Secondary prevention: Optimal medical therapy (OMT)
- Antiplatelet therapy duration based on intervention/risk
- Lipid management: High-intensity statins, consider PCSK9 inhibitors
- ACE inhibitors/ARBs for LV dysfunction
- Beta-blockers: Especially post-MI or with heart failure
- Lifestyle modifications: Smoking cessation, exercise, Mediterranean diet
- Vasospastic angina: CCBs, nitrates; avoid beta-blockers
- Microvascular angina: Beta-blockers, CCBs, ranolazine, ACE inhibitors
- Women: More aggressive risk factor modification, lower thresholds for advanced testing
- Diabetes: More aggressive lipid targets, consider SGLT2 inhibitors/GLP-1 RAs with CV benefit
Newer Diagnostic Approaches
1. Beyond angiography:
- Coronary flow reserve (CFR) assessment
- Intracoronary acetylcholine testing for vasospasm
- CT fractional flow reserve (CT-FFR)
- PET myocardial perfusion imaging
- Cardiac MRI for microvascular disease
- High-sensitivity CRP
- Cardiac microRNAs
- Markers of endothelial dysfunction
