USMLE/COMLEX 2 - Inflammatory Bowel Disease
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 2 & COMLEX-USA Level 2 from the Inflammatory Bowel Disease tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
- --
VITAL FOR USMLE/COMLEX 2
Inflammatory Bowel Disease (IBD)
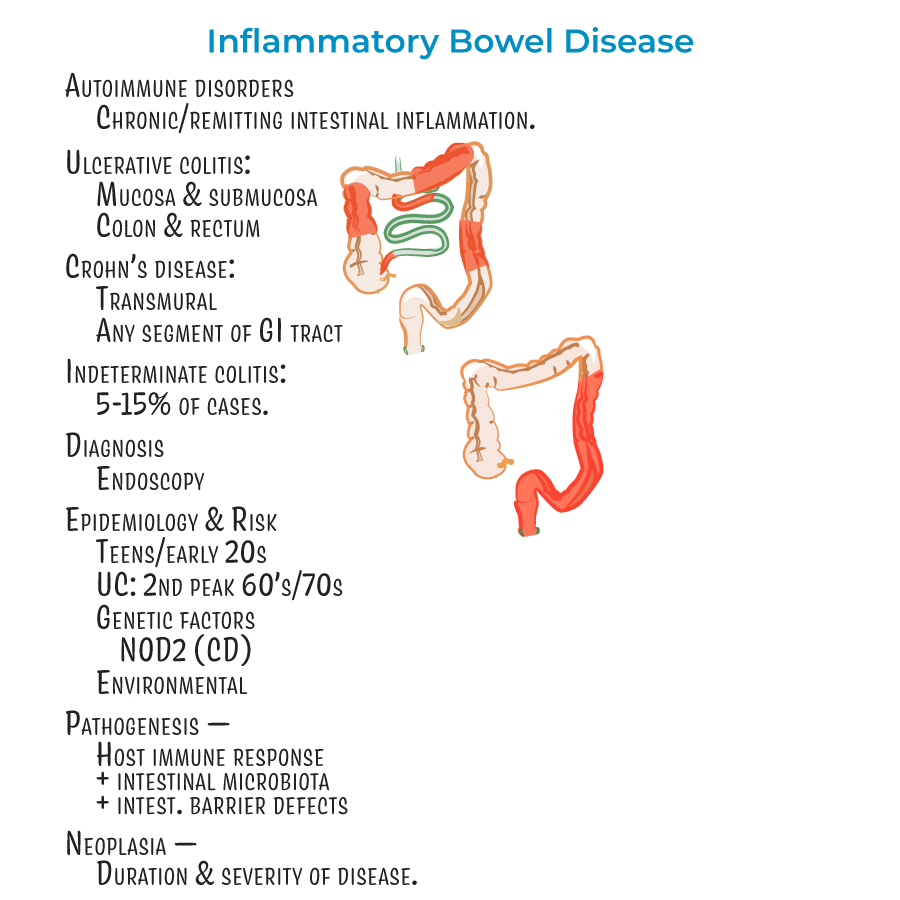
1. Autoimmune disorders characterized by chronic or remitting intestinal inflammation.
2. Diagnosis relies on endoscopy.
3. Most patients diagnosed in teens/early 20s; ulcerative colitis has a second "peak" in patients in their 60's or 70's.
4. Associated with neoplasia, influenced by duration and severity of disease.
5. Extraintestinal manifestations: Most common are skin lesions (in up to 40% of patients), uveitis, and arthritis.
6. Less common but potentially deadly complications: involvement of liver/gallbladder, lung, pancreas, and kidneys.
Crohn's Disease
1. Characterized by transmural inflammation (can reach all layers of GI tract).
2. Can affect any segment of GI tract, but most commonly involves ileum and colon.
3. "Skip lesions" - discontinuous pattern with normal areas between affected segments.
4. Rectum usually spared (unlike ulcerative colitis).
5. Clinical presentation: Abdominal cramping (often on the right side), diarrhea (potentially bloody), fever and malaise, weight loss, perianal lesions (25% of patients).
6. Complications: Problems related to fistulas, fissures, and obstructive strictures; dysplasia and adenocarcinoma; anemia from chronic blood loss.
7. Treatment: Avoid cigarette smoking (exacerbates inflammation), anti-inflammatories, immune suppressors, surgery when necessary.
Ulcerative Colitis
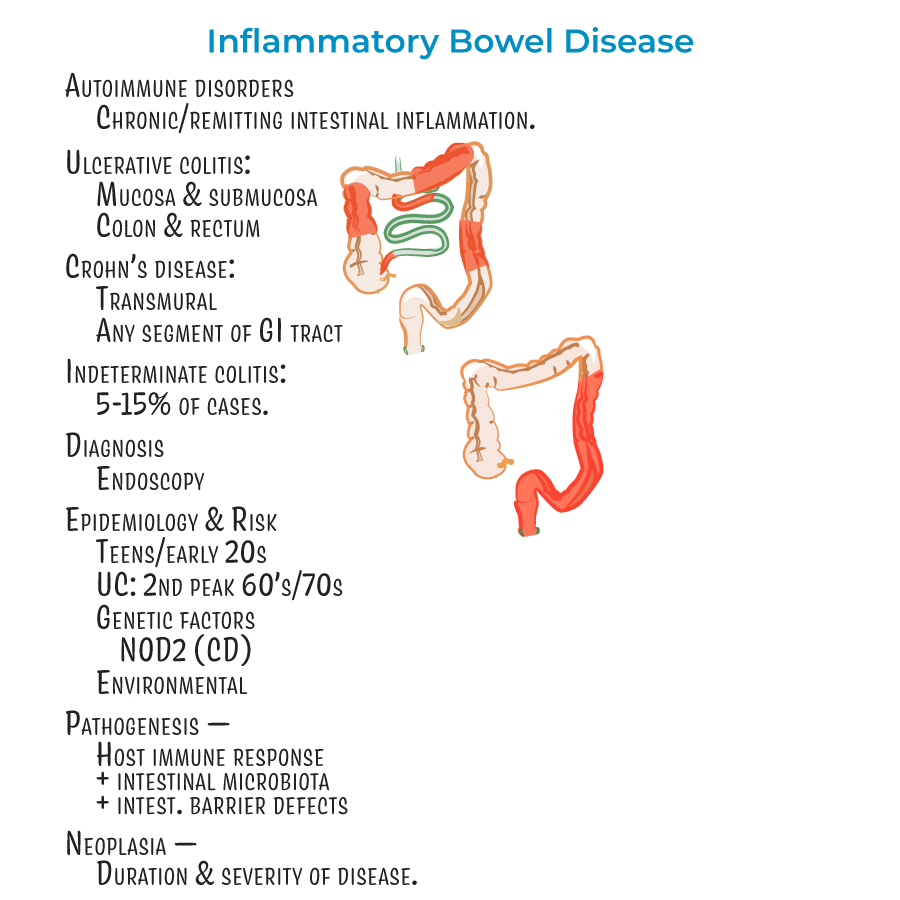
1. Inflammation of mucosal and submucosal layers only.
2. Restricted to the colon and rectum.
3. Characterized by continuous lesions (unlike Crohn's disease).
4. Clinical presentation: Bloody diarrhea with rectal bleeding, abdominal pain, fever, and weight loss.
5. Complications: Toxic ulceritis, toxic megacolon, intestinal perforation, dysplasia and adenocarcinoma (more likely with pancolitis).
6. Treatment: Anti-inflammatories, immune suppressors, and colectomy. Patients who smoke more likely to experience bouts upon quitting.
- --
HIGH YIELD
Inflammatory Bowel Disease
1. About 5-15% of cases are considered "indeterminant" colitis when distinction between UC and CD is difficult.
2. Environmental factors are important (diet, cigarette smoking, medications).
3. Result of detrimental interactions between host immune response, intestinal microbiota, and intestinal barrier defects.
4. Genetic factors play a role (e.g., mutations in NOD2 associated with Crohn's disease).
5. Different types of T-helper cells play major roles in each disease.
Crohn's Disease
1. Many studies suggest a female predominance.
2. Transmural inflammation with wall thickening and "creeping fat" that wraps around the GI tract.
3. Lesion progression:
- Aphthous erosions (early shallow whitish sores)
- Longitudinal "bear claw" ulcers (like rake dragged down GI lining)
- Cobblestone appearance (tissue crowded with ulcers)
- Fissures leading to fistulas (connecting to abdominal/pelvic cavity or other organs)
Ulcerative Colitis
1. Sunken, red/bloody ulcers with friable appearance.
2. Inflammation destroys submucosal vascular network.
3. Mucosa is bloody during active inflammation.
4. Remaining mucosa creates "pseudopolyps".
5. Histology: Branching and distension of intestinal crypts, crypt abscesses with neutrophils.
6. Inflammation is Th2 cell-mediated.
Differential Diagnosis
1. Key clinical differences:
- CD = transmural inflammation, skip lesions, any GI segment, rectum usually spared
- UC = mucosal/submucosal inflammation, continuous lesions, colon/rectum only
- --
Beyond the Tutorial
Clinical Evaluation
1. Initial workup: CBC, CRP, ESR, comprehensive metabolic panel, stool studies (culture, C. diff, parasites).
2. Fecal calprotectin: High sensitivity for intestinal inflammation, useful for monitoring disease activity.
3. Endoscopic scoring systems: Mayo score for UC, CDAI and SES-CD for Crohn's disease.
4. Cross-sectional imaging: CT enterography and MR enterography to evaluate small bowel involvement and complications.
Medical Management
1. Induction therapy: Corticosteroids, biologics, or combination therapy based on disease severity.
2. Maintenance therapy: 5-ASA compounds, immunomodulators, biologics tailored to disease phenotype.
3. Biologics classification:
- Anti-TNF agents (infliximab, adalimumab, certolizumab, golimumab)
- Anti-integrin agents (vedolizumab, natalizumab)
- Anti-IL-12/23 (ustekinumab)
- JAK inhibitors (tofacitinib)
Surgical Management
1. Indications for surgery in UC: Medically refractory disease, dysplasia/cancer, fulminant colitis, toxic megacolon.
2. Surgical options for UC: Total proctocolectomy with IPAA, total proctocolectomy with end ileostomy.
3. Indications for surgery in CD: Obstruction, perforation, abscess, fistula, medically refractory disease.
4. Surgical approaches in CD: Resection with anastomosis, strictureplasty, fistula repair, abscess drainage.
5. Post-operative recurrence prevention: Risk stratification and prophylaxis strategies.
Special Clinical Scenarios
1. Acute severe ulcerative colitis: IV steroids, timely rescue therapy decisions, objective criteria for colectomy.
2. Perianal Crohn's disease: Combined medical-surgical approach, seton placement, advancement flaps.
3. Pregnancy management: Most medications safe during pregnancy, active disease more harmful than treatment.
4. Primary sclerosing cholangitis with IBD: Increased colorectal cancer risk, need for annual surveillance.
5. IBD in pediatric patients: Growth failure, delayed puberty, bone health, transition to adult care.
Complications Management
1. Toxic megacolon: NPO, NG decompression, broad-spectrum antibiotics, IV steroids, surgical consultation.
2. Intestinal strictures: Endoscopic balloon dilation vs. surgical management.
3. Colorectal cancer surveillance: Chromoendoscopy, targeted biopsies, surveillance intervals.
4. Nutritional deficiencies: Screening and replacement protocols for iron, B12, folate, zinc, vitamin D.
5. Post-operative IPAA complications: Pouchitis diagnosis and treatment algorithm.
Emerging Concepts
1. Treat-to-target strategy: Mucosal healing as objective endpoint beyond symptom control.
2. Therapeutic drug monitoring: Proactive vs. reactive approaches, thresholds for dose optimization.
3. Precision medicine: Biomarkers to predict treatment response and guide therapy selection.
4. Combination therapy: Benefits vs. risks of combined immunosuppression strategies.
5. Novel therapies: Sphingosine-1-phosphate modulators, leukocyte trafficking inhibitors, microbiome-based therapies.
