USMLE/COMLEX 2 - Hypertension Pathophysiology
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 2 CK & COMLEX-USA Level 2 from the Blood Pressure Regulation and Hypertension tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
 2. Kidney's Role in Hypertension:
Below is information not explicitly contained within the tutorial but important for USMLE Step 2 CK & COMLEX Level 2.
2. Kidney's Role in Hypertension:
Below is information not explicitly contained within the tutorial but important for USMLE Step 2 CK & COMLEX Level 2.
- --
VITAL FOR USMLE/COMLEX 2
Blood Pressure Regulation - Clinical Significance
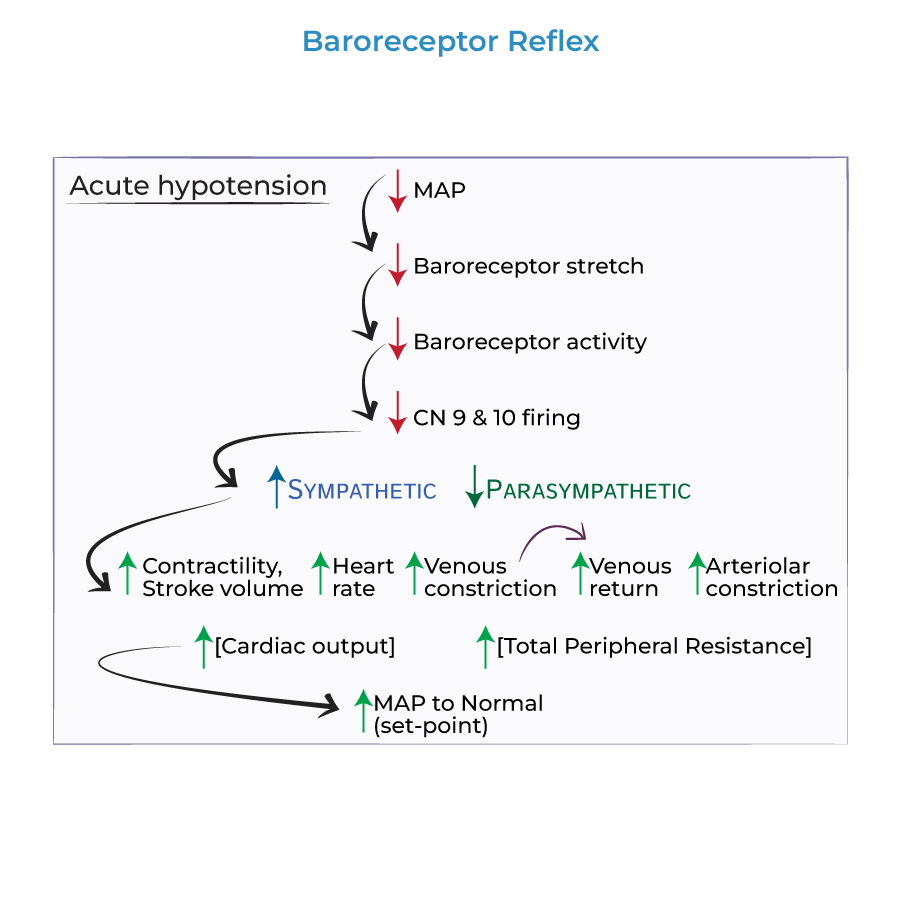
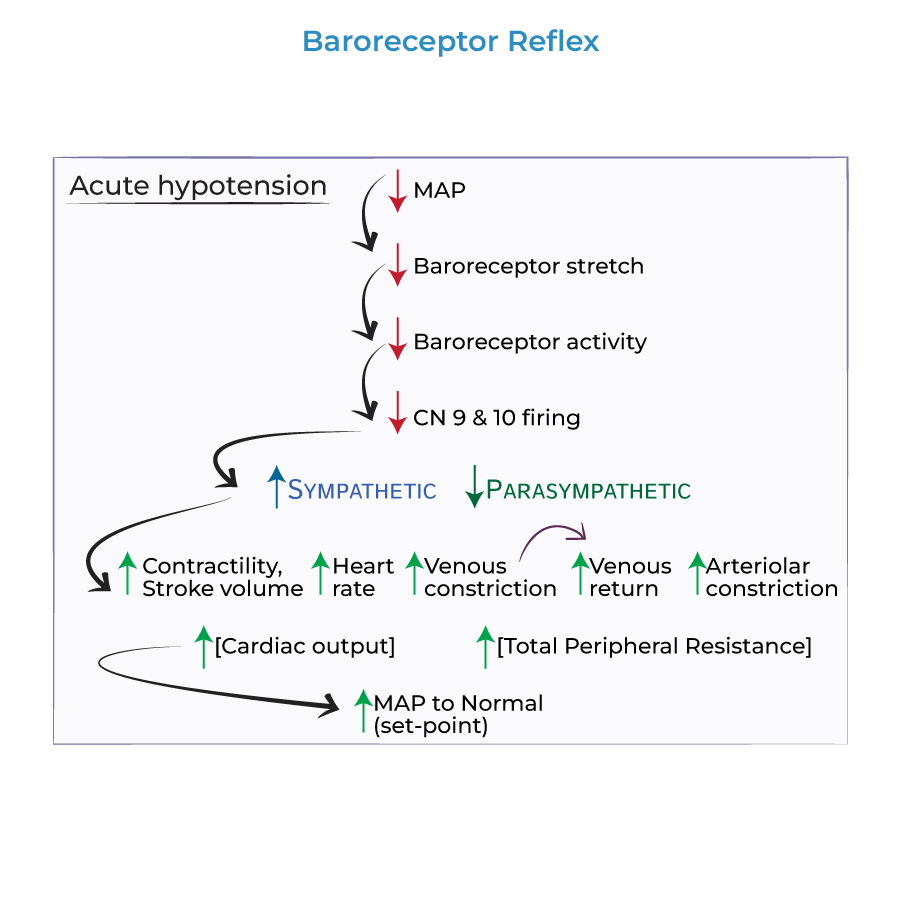
1. Mean arterial pressure is determined by cardiac output and total peripheral resistance.
2. Hypertension results from increased cardiac output and/or increased total peripheral resistance.
3. Cardiac output is the product of heart rate and stroke volume.
4. Stroke volume is determined by preload and contractility.
5. Blood volume contributes to preload via increased venous return.
Mediators of Blood Pressure in Clinical Context
1. Antidiuretic hormone (vasopressin):
- Vasoconstrictor
- Increases sodium and water retention
- Clinical relevance: implicated in volume-dependent hypertension
- Similar effects to ADH
- Clinical relevance: primary hyperaldosteronism as a cause of secondary hypertension
- Direct effects: vasoconstriction and increased sodium/water retention
- Indirect effects: stimulates release of norepinephrine, ADH, and aldosterone
- Clinical relevance: multiple antihypertensive drug classes target this system
- Increases heart rate, contractility, and vasoconstriction
- Clinical relevance: sympathetic hyperactivity in hypertension
Hypertensive Crisis Management
1. Hypertensive urgency: Blood pressure >180/120 mmHg without end-organ damage
2. Hypertensive emergency: Blood pressure >180/120 mmHg WITH end-organ damage
3. Clinical presentation: Severe headache, confusion, visual impairment, chest pain, dyspnea, nausea/vomiting, anxiety, seizures
4. Management approach: Different based on presence/absence of end-organ damage
- --
HIGH YIELD
Clinical Applications of BP Regulation Mechanisms
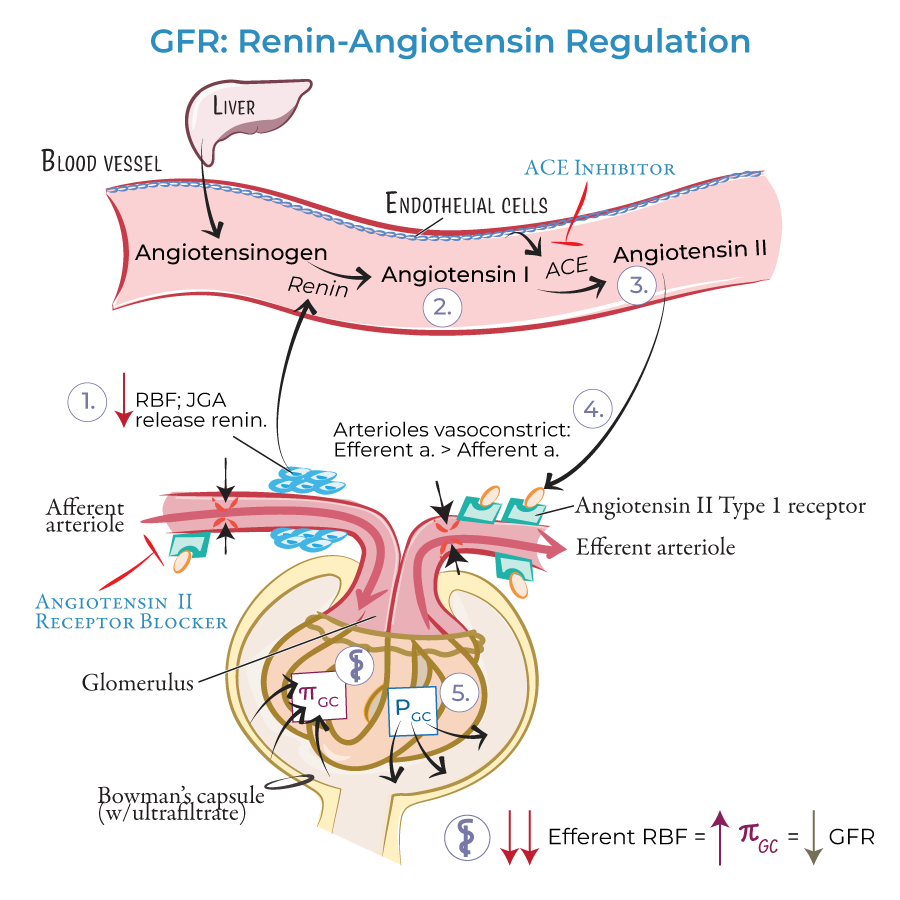
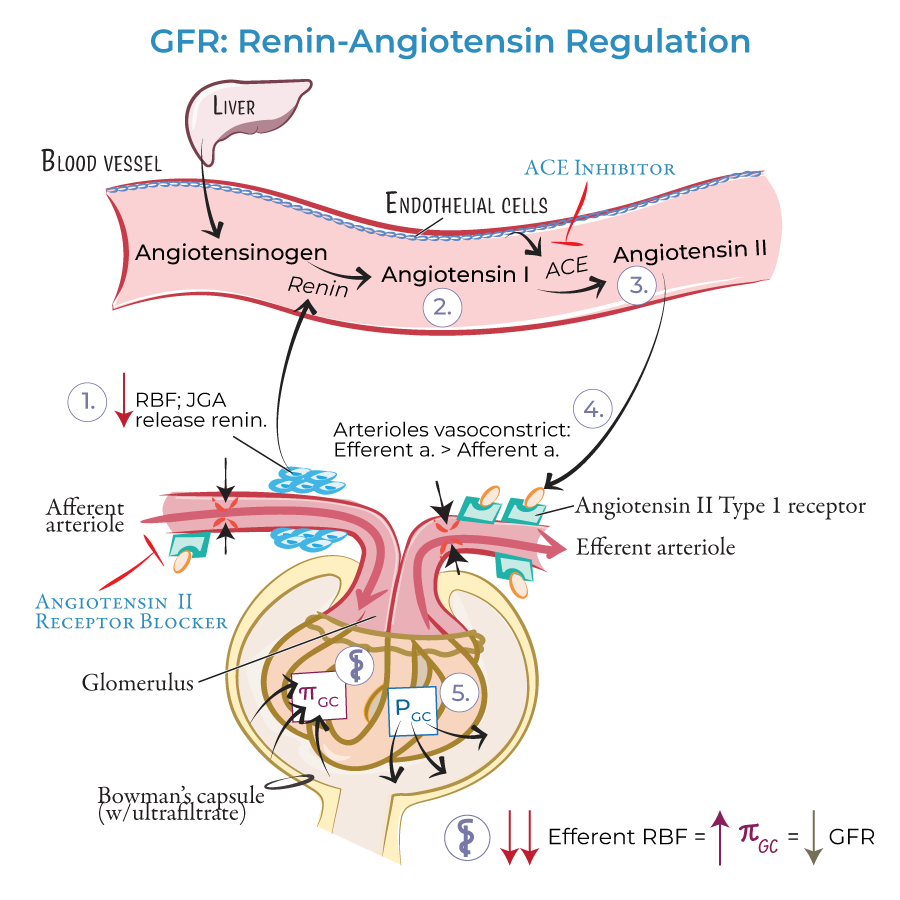
1. Renin-Angiotensin-Aldosterone System (RAAS):
- Clinical significance: Primary target for antihypertensive medications
- Angiotensin II breaks down bradykinin (vasodilator)
- Therapeutic implication: ACE inhibitors both reduce angiotensin II and increase bradykinin
 2. Kidney's Role in Hypertension:
2. Kidney's Role in Hypertension:
- Sodium and water retention affects blood volume
- Clinical application: Salt-sensitive patients require dietary sodium restriction
- Therapeutic implication: Diuretics effective in volume-dependent hypertension
- Hypertension produces damage leading to vascular changes
- Clinical significance: Elevated endothelin and reduced nitric oxide
- Therapeutic implication: Long-standing hypertension may be more resistant to treatment
- Clinical relevance: Patients with salt-sensitive hypertension develop elevated BP with high sodium intake
- Therapeutic implication: Dietary modifications crucial for these patients
Secondary Hypertension Evaluation
1. Aldosterone-secreting tumors:
- Mechanism: Increased blood volume and preload
- Clinical presentation: Hypertension with hypokalemia
- Diagnostic approach: Plasma aldosterone to renin ratio
- Multiple factors affect components of BP regulation
- Clinical application: Family history and lifestyle assessment essential in workup
- Therapeutic implication: Lifestyle modifications as foundation of treatment
- --
Beyond the Tutorial
Clinical Management Considerations
1. Antihypertensive medication classes:
- ACE inhibitors: Target angiotensin II formation
- ARBs: Block angiotensin II receptor
- Diuretics: Reduce blood volume
- Calcium channel blockers: Induce vasodilation
- Beta-blockers: Reduce heart rate and contractility
- Pregnancy: Preeclampsia risk assessment and management
- Elderly: Risk of orthostatic hypotension with treatment
- Diabetes: Tighter BP goals and medication preferences
- Left ventricular hypertrophy
- Stroke
- Chronic kidney disease
- Aortic dissection
Case-Based Applications
1. Patient with salt-sensitive hypertension:
- Presentation: BP fluctuations with dietary sodium changes
- Approach: Low-sodium diet, diuretic therapy
- Initial assessment: Evaluate for end-organ damage
- Immediate approach: Gradual BP reduction to prevent cerebral hypoperfusion
- Medication selection based on presenting complication
