USMLE/COMLEX 2 - Heart Murmurs
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 2 & COMLEX 2 from the Hypertension Overview tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
- --
VITAL FOR USMLE Step 2 & COMLEX 2
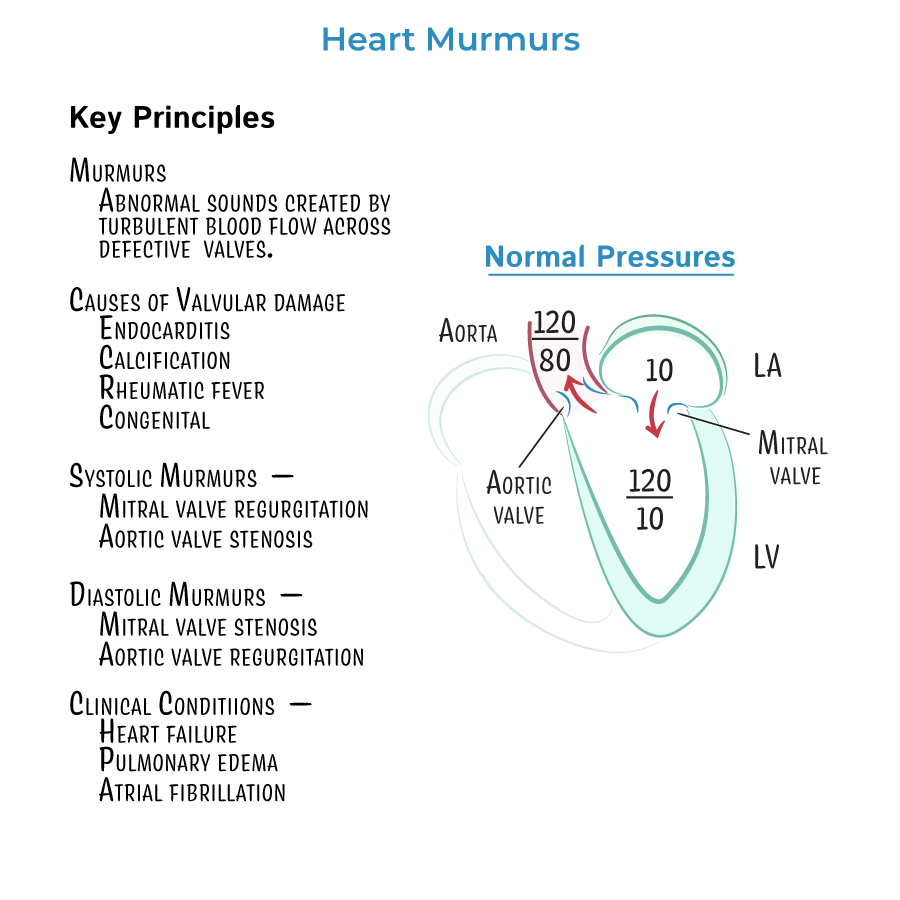
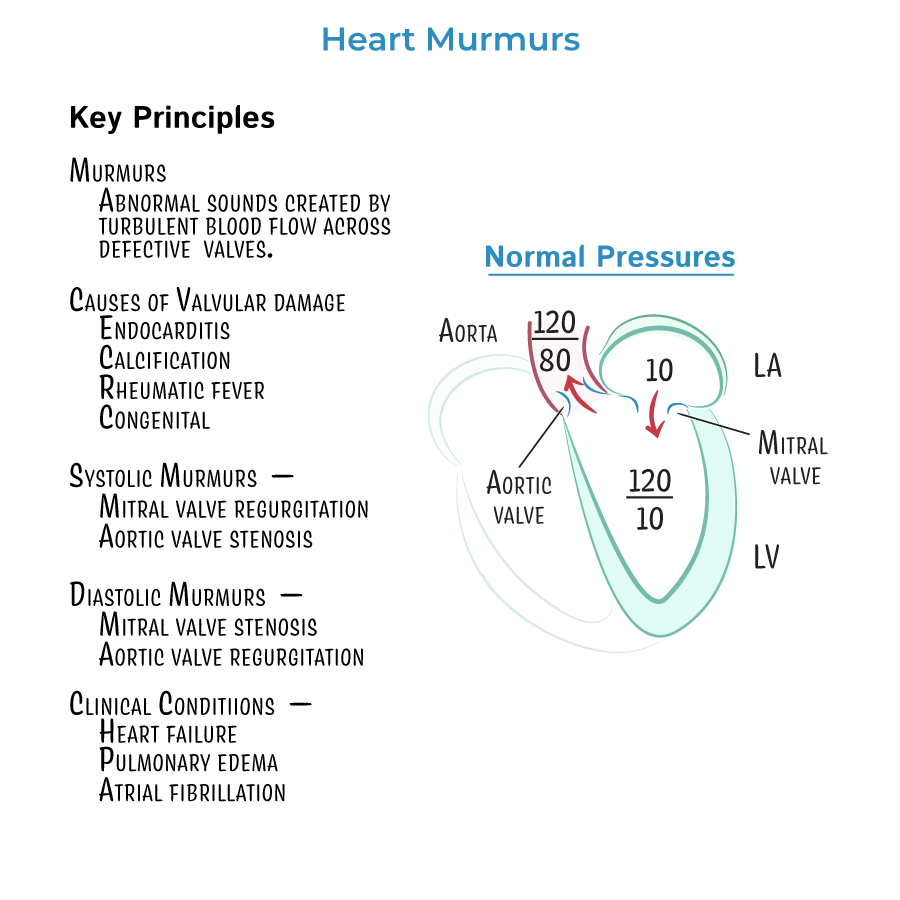
1. Heart Murmur Timing and Classification
- Systolic murmurs: Aortic stenosis, Mitral regurgitation, Mitral valve prolapse
- Diastolic murmurs: Aortic regurgitation, Mitral stenosis
- Continuous murmur: Patent ductus arteriosus
2. Aortic Stenosis (AS)
- Harsh, crescendo-decrescendo systolic murmur at right upper sternal border, radiates to carotids
- Symptoms: Syncope, Angina, Dyspnea (SAD)
- Classic finding: Delayed, diminished carotid upstroke (pulsus parvus et tardus)
- Best initial test: Echocardiogram
- Definitive management: Valve replacement when symptomatic or EF <50%
3. Mitral Regurgitation (MR)
- Holosystolic murmur at apex, radiates to axilla
- Causes: MVP, ischemic heart disease (papillary muscle rupture), endocarditis, rheumatic fever
- Symptoms: Dyspnea, fatigue, atrial fibrillation
- Management: ACE inhibitors, diuretics; surgery for severe symptomatic MR or LV dysfunction
4. Mitral Valve Prolapse (MVP)
- Mid-systolic click followed by late systolic murmur
- ↑ with Valsalva/standing, ↓ with squatting (due to reduced preload)
- Common in young women; may be benign or cause MR
- May require monitoring via echo
5. Aortic Regurgitation (AR)
- Early diastolic decrescendo murmur at left sternal border
- Features: Wide pulse pressure, bounding pulses (Corrigan’s sign), head bobbing
- Causes: Infective endocarditis, aortic root dilation (Marfan), bicuspid aortic valve
- Management: Vasodilators (ACEi), surgical valve replacement if severe
6. Mitral Stenosis (MS)
- Opening snap + diastolic rumble, best at apex in left lateral decubitus
- ↑ with exercise or pregnancy
- Most common cause: Rheumatic fever
- Complications: Atrial fibrillation, pulmonary HTN
- Management: Diuretics, rate control (if AF), valve intervention if symptomatic or pulmonary HTN
7. Murmur Response to Maneuvers
- Squatting/leg raise: ↑ preload → ↑ most murmurs (except MVP, HOCM)
- Valsalva/standing: ↓ preload → ↑ MVP, ↑ HOCM, ↓ most other murmurs
8. Clinical Vignette Patterns
- Elderly with exertional syncope and crescendo-decrescendo murmur → Aortic stenosis
- Young woman with mid-systolic click + murmur louder with Valsalva → MVP
- Migrant with pregnancy and murmur + LAE and dyspnea → Mitral stenosis
- Infective endocarditis + new murmur + pulmonary edema → Mitral or aortic regurgitation
9. Auscultation vs. Echo
- Auscultation is initial clue, but echocardiogram is confirmatory and defines severity
- TTE is typically sufficient; TEE if suspecting endocarditis or poor windows
10. Valvular Disease → Heart Failure
- All chronic regurgitant lesions (MR, AR) → Volume overload → Eccentric hypertrophy
- Stenotic lesions (AS, MS) → Pressure overload → Concentric hypertrophy or atrial dilation
- --
HIGH YIELD
11. Management of MR and AR
- Vasodilators (ACEi/ARB, nifedipine) reduce afterload in regurgitant lesions
- Surgical referral for severe, symptomatic disease or when LV dysfunction occurs
12. MS and Pregnancy
- Pregnancy increases plasma volume → worsens MS symptoms
- Avoid volume overload; beta blockers to slow HR and prolong diastole
13. Prosthetic Valve Indications
- Severe symptoms (NYHA Class III–IV)
- EF < 50% in asymptomatic AR or MR
- Severe stenosis with symptoms or valve area <1.0 cm² (AS, MS)
14. Endocarditis Risk
- Highest in patients with prosthetic valves, prior endocarditis, or congenital defects
- Mitral regurgitation and aortic regurgitation are common sites
15. Murmur Differentiation Tip
- Systolic ejection murmur with radiation to carotids = AS
- Holosystolic murmur radiating to axilla = MR
- Decrescendo early diastolic murmur = AR
- Opening snap + mid-diastolic rumble = MS
- Mid-systolic click = MVP
- --
Beyond the Tutorial
16. Multisystem Clues
- Marfan + murmur + head bobbing → AR
- Young hypertensive female + murmur + BP discrepancy → Coarctation of aorta
- IV drug user + fever + new murmur → Tricuspid regurgitation from endocarditis
17. Echo Frequency
- MR/AR/MVP: follow with echo every 6–12 months if severe
- Mild cases: every 3–5 years
- Use TEE if endocarditis, prosthetic valve suspicion, or poor TTE quality
18. Antibiotic Prophylaxis
- Only for high-risk patients undergoing dental procedures:
- Prosthetic valves
- Prior infective endocarditis
- Certain congenital heart diseases
