USMLE/COMLEX 2 - Gastritis & Peptic Ulcer Disease
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 2 & COMLEX-USA Level 2 from the Gastritis & Peptic Ulcer Disease tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
 Below is information not explicitly contained within the tutorial but important for USMLE & COMLEX 2.
Below is information not explicitly contained within the tutorial but important for USMLE & COMLEX 2.
- --
VITAL FOR USMLE/COMLEX 2
Clinical Presentation
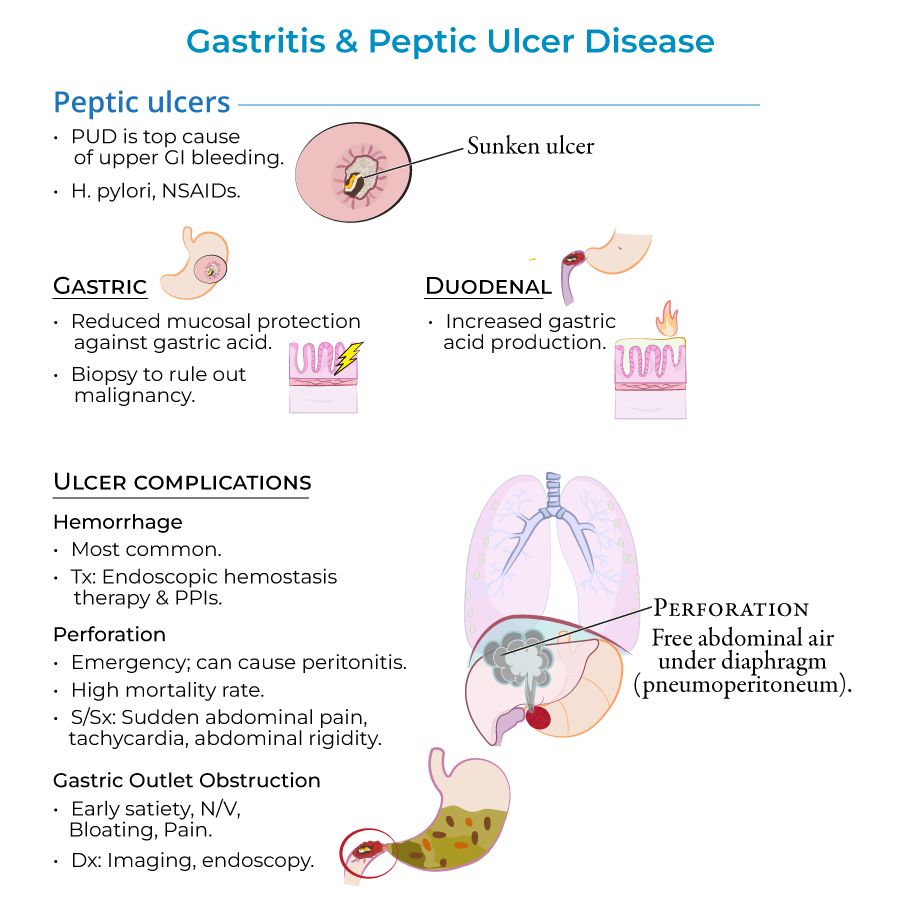
1. Signs and symptoms include epigastric pain, GI bleeding, and nausea or vomiting; many patients are asymptomatic, especially in early phases.
2. Gastric ulcer pain typically increases upon eating, leading patients to avoid food and lose weight.
3. Duodenal ulcer pain is often relieved by eating and may be associated with weight gain, though these patterns are not always consistent.
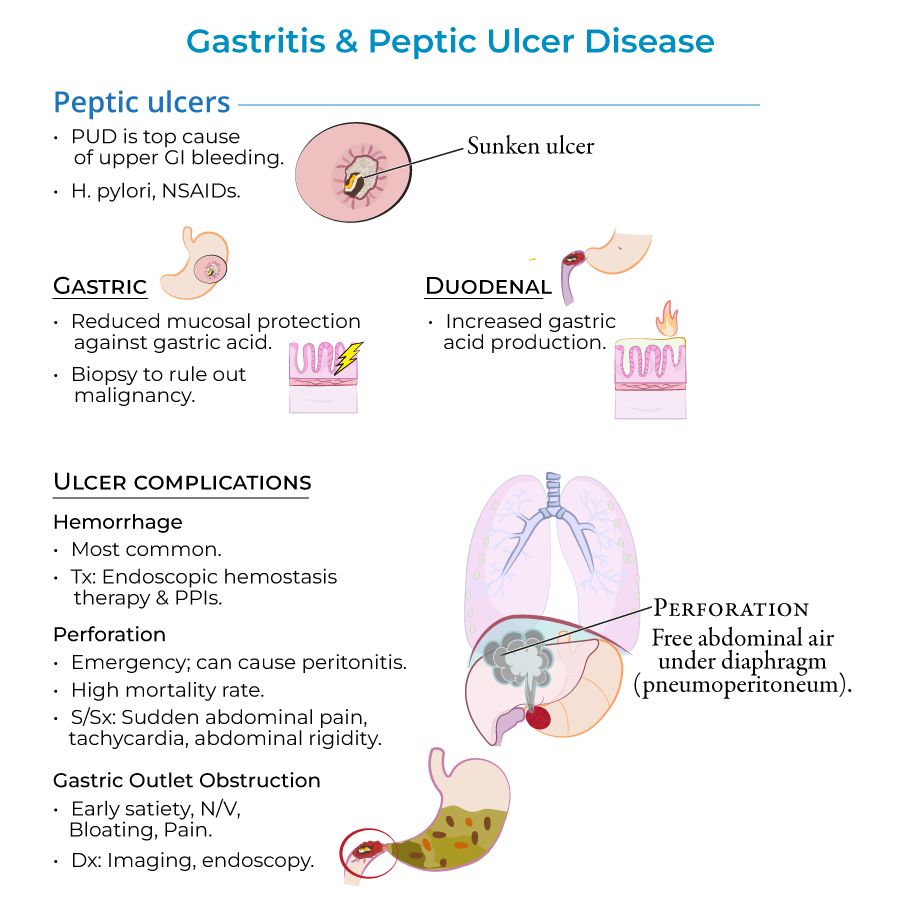
4. Peptic ulcer perforation presents with sudden abdominal pain, tachycardia, and abdominal rigidity.
5. Gastric outlet obstruction manifests with early satiety, nausea, vomiting, bloating, and pain.
Diagnostic Approach
1. Diagnosis relies on upper endoscopy to visualize lesions and biopsies to assess inflammation, H. pylori infection, and malignancy.
2. For patients younger than 60 years without alarming symptoms, focus on non-invasive H. pylori testing and PPI response.
3. Urea breath test and stool antigen tests are preferred non-invasive methods to detect active H. pylori infection.
4. H. pylori antibody serologies do not distinguish between active and inactive disease.
5. Patients older than 60 years or with alarming symptoms (weight loss, anemia, bloody stools, dysphagia) require upper endoscopy.
Management
1. Treatment involves proton pump inhibitors, NSAID discontinuation, and H. pylori eradication with antibiotics when present.
2. Follow-up testing is necessary to confirm H. pylori eradication and prevent relapse.
3. Hemorrhaging complications can be treated with endoscopic hemostasis therapies and proton pump inhibitors.
4. For gastric outlet obstruction, try treatment of the underlying peptic ulcer disease before attempting surgical solutions.
5. Non-ulcer dyspepsia is treated with proton pump inhibitors after ruling out cancer in those over 55 years old.
- --
HIGH YIELD
Etiology & Risk Factors
1. H. pylori is present in approximately 70% of gastric ulcer cases and 90% of duodenal ulcer cases.
2. NSAIDs, aspirin, and alcohol are common causes of acute gastritis, especially when alcohol and aspirin are combined.
3. NSAIDs block prostaglandin synthesis necessary for mucous production, while alcohol causes direct damage to the mucosal lining.
4. Cigarette smoking is an important risk factor for peptic ulcer disease.
5. Contrary to popular belief, psychological stress and spicy foods do not cause peptic ulcers.
Complications & Special Considerations
1. Peptic ulcers are the most common cause of upper GI bleeding, though most ulcers do not bleed.
2. Perforation has a high mortality rate (up to 30%) and requires emergency intervention.
3. Imaging of perforation will show free abdominal air under the diaphragm (pneumoperitoneum).
4. Gastric ulcers have a higher risk of malignancy (5-10%) compared to duodenal ulcers, making early detection crucial.
5. Stress ulcers develop in acute, severe illness: Curling ulcers from systemic burns causing hypovolemia, and Cushing ulcers from brain injury producing increased vagal stimulation.
Associated Conditions
1. Chronic gastritis often leads to atrophy, characterized by loss of gastric glands and folds with increased risk of malignancy.
2. H. pylori increases the risk of peptic ulcer disease, gastric cancer, and primary gastric MALT lymphomas.
3. Autoimmune gastritis involves T-cell mediated destruction of parietal cells and can lead to pernicious anemia.
4. Patients with autoimmune gastritis are likely to have other autoimmune disorders.
5. Zollinger-Ellison syndrome is a rare cause of gastric ulcers due to gastrinoma.
- --
Beyond the Tutorial
Advanced Management
1. PPI prophylaxis is recommended for high-risk patients on chronic NSAID therapy (elderly, history of PUD, concurrent steroid or anticoagulant use).
2. First-line H. pylori treatment: 14-day triple therapy with PPI + clarithromycin + amoxicillin/metronidazole.
3. Rescue regimens for H. pylori include bismuth quadruple therapy, levofloxacin-based therapy, or rifabutin-based therapy.
4. Surgical options for refractory PUD: vagotomy, antrectomy, pyloroplasty, or gastrectomy depending on location and etiology.
5. Transcatheter arterial embolization may be used for patients with bleeding ulcers who fail endoscopic therapy and are poor surgical candidates.
Special Populations
1. Pregnancy: H. pylori testing typically deferred; amoxicillin and metronidazole are preferred if treatment necessary.
2. Pediatric patients: Higher rates of primary antibiotic resistance require careful treatment selection.
3. Immunocompromised patients: Higher risk of severe disease and complications from H. pylori infection.
4. Intensive care patients: Stress ulcer prophylaxis recommended, with evidence favoring PPIs over H2 blockers.
5. Elderly patients: Higher risk of drug interactions with PPIs and antibiotic therapies for H. pylori.
