USMLE/COMLEX 2 - Endocarditis
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 2 & COMLEX-USA Level 2 from the Endocarditis tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
 Additional information not explicitly contained in the tutorial but important for USMLE & COMLEX 2:
Additional information not explicitly contained in the tutorial but important for USMLE & COMLEX 2:
- --
VITAL FOR USMLE/COMLEX 2
Clinical Presentation
1. Acute endocarditis can present with fever, chills, and other flu-like symptoms.
Complications
1. Vegetations can invade and destroy underlying tissues or break free and become emboli.
2. Endocarditis is associated with stroke, organ failure, and sepsis due to emboli lodging in blood vessels and spreading pathogens systemically.
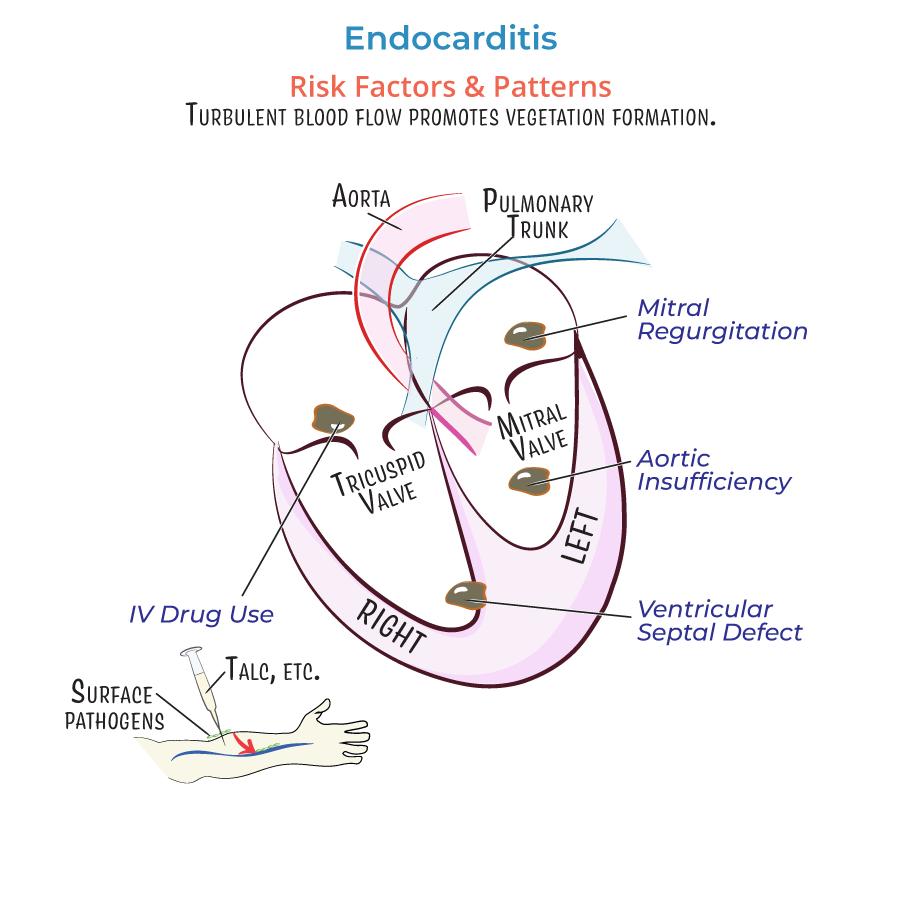
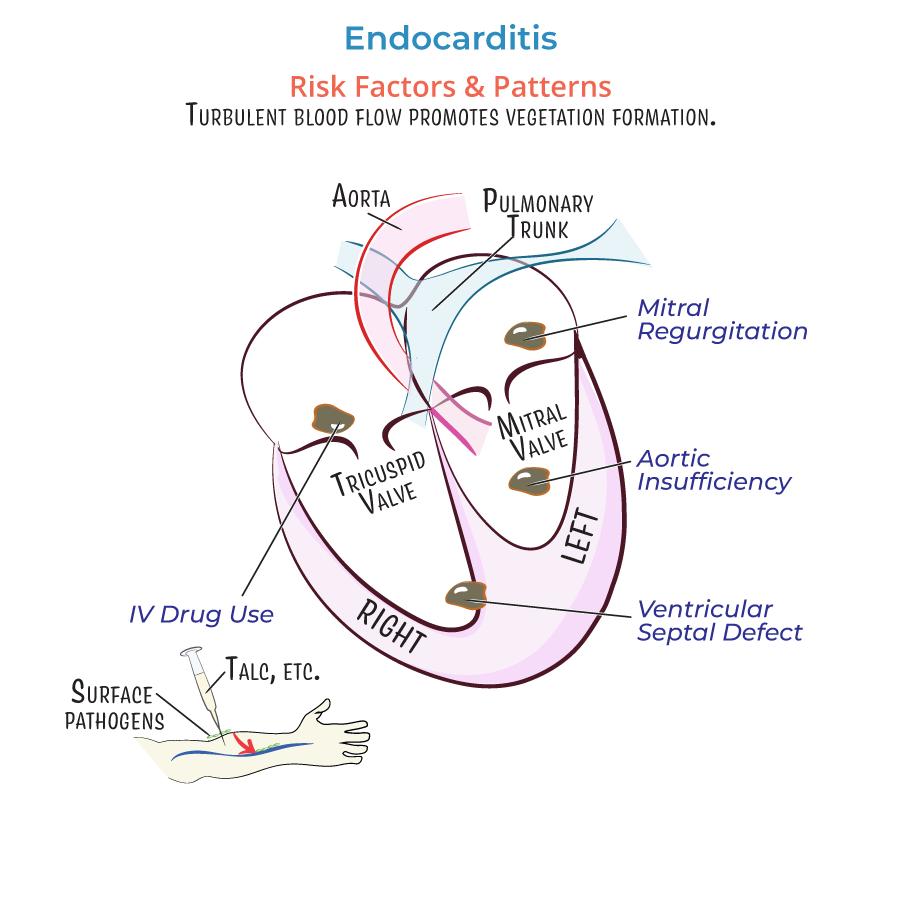
Risk Factors and Patient Populations
1. Valvular damage: Vegetations are more likely to form where damage already exists.
2. Catheter-induced abrasion or prosthetic devices can cause initial inflammation.
3. Intravenous drug use: Major cause of right-sided valvular endocarditis due to particulate matter (talc) or skin pathogens introduced into bloodstream.
4. Prosthetic valves: More susceptible to infection as bacteria and debris adhere to prosthetic materials.
Pathogen Patterns
1. Infective endocarditis: Most commonly caused by gram-positive bacteria:
- Staphylococcus aureus (most common)
- Viridans group Streptococci
- Enterococci
- Coagulase-negative Staphylococci
- --
HIGH YIELD
Pattern Recognition by Valve and Condition
1. Mitral valve regurgitation: Produces lesions and vegetations on the atrial leaflet surface.
2. Aortic insufficiency: Produces vegetations on the ventricular side.
3. Ventricular septal defects: Right-sided vegetations near the orifice.
4. Rheumatic heart disease: Small vegetations located near edge of leaflet.
5. Libman-Sacks endocarditis (associated with SLE):
- Small and medium-sized vegetations on both sides of leaflets
- Less inflammation means vegetations are loosely attached
- Increased risk of embolism due to loosely attached vegetations
Special Populations and Considerations
1. IV drug users:
- Right-sided valvular endocarditis
- Introduction of particulate matter, skin pathogens, or oral flora (if saliva used on needles)
- Higher infection risk at prosthetic annular ring-tissue junction
- Invasive vegetations can form and deform valvular leaflets
- Often requires surgical valve replacement
- Coxiella burnetii
- Brucella species
- Tropheryma whipplei
Fungal Endocarditis
1. Most commonly caused by Candida species (particularly C. albicans) and Aspergillus species.
- --
Beyond the Tutorial
Diagnostic Approach
1. Modified Duke criteria: Primary diagnostic framework using major and minor criteria
2. Blood cultures: At least three sets from different venipuncture sites
3. Echocardiography: TEE has higher sensitivity than TTE, especially for prosthetic valves
4. Laboratory findings: Elevated ESR, CRP, anemia, hematuria, and rheumatoid factor
Treatment Principles
1. Antimicrobial therapy:
- 4-6 weeks of IV antibiotics for native valve endocarditis
- 6+ weeks for prosthetic valve endocarditis
- Empiric therapy should target likely organisms while awaiting culture results
- Moderate to severe heart failure
- Uncontrolled infection
- Prevention of embolic events
- Large vegetations (>10mm)
- Abscess formation
Prevention and Prophylaxis
1. Prophylaxis guidelines: Limited to highest risk patients for specific procedures
2. High-risk conditions: Prosthetic valves, previous endocarditis, congenital heart disease, cardiac transplant with valvulopathy
3. Management of IV drug users: Addiction treatment as important as treating the infection
