USMLE/COMLEX 2 - Diabetes Mellitus Pathophysiology
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 2 & COMLEX-USA Level 2 from the Diabetes Mellitus - Pathophysiology tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
- --
VITAL FOR USMLE/COMLEX 2
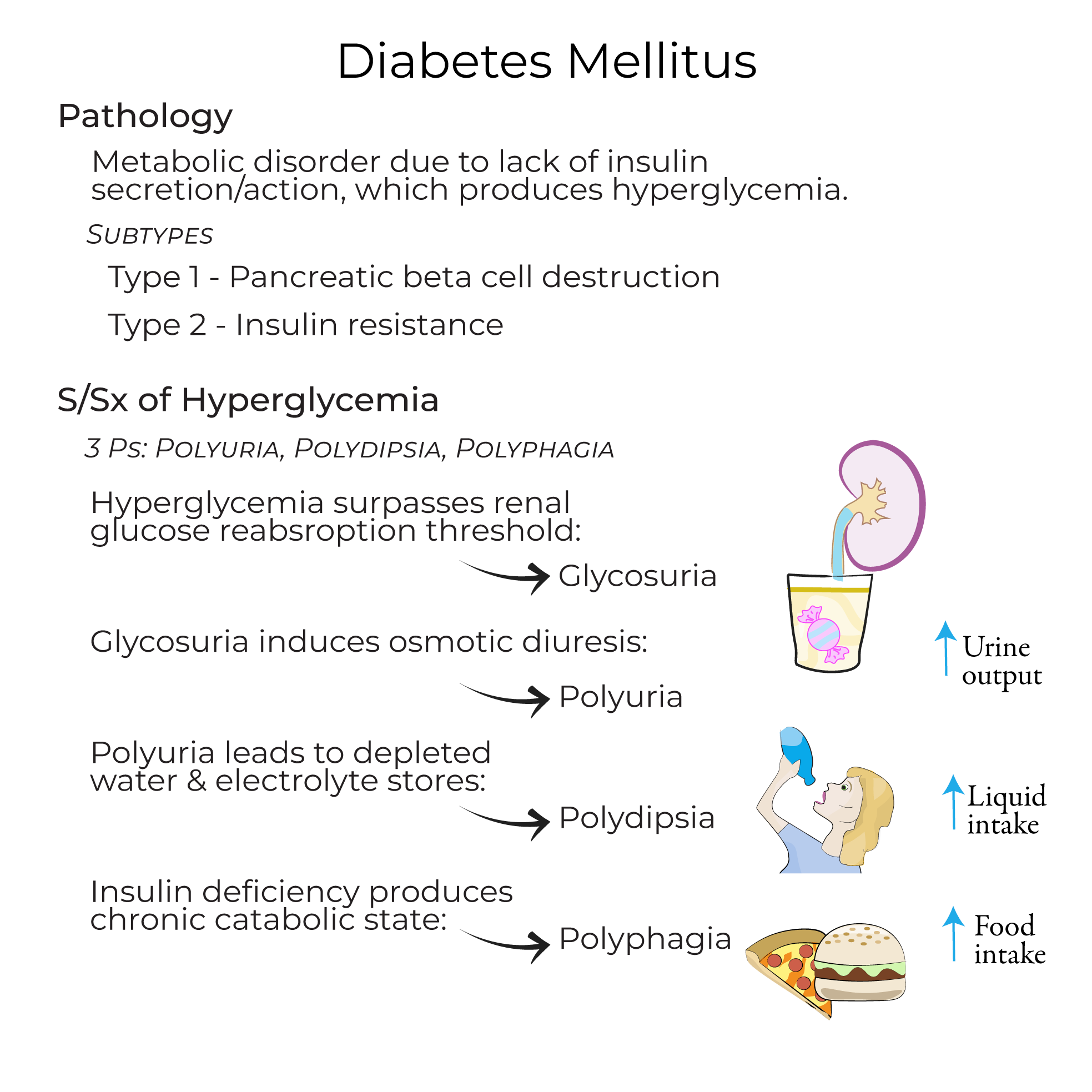
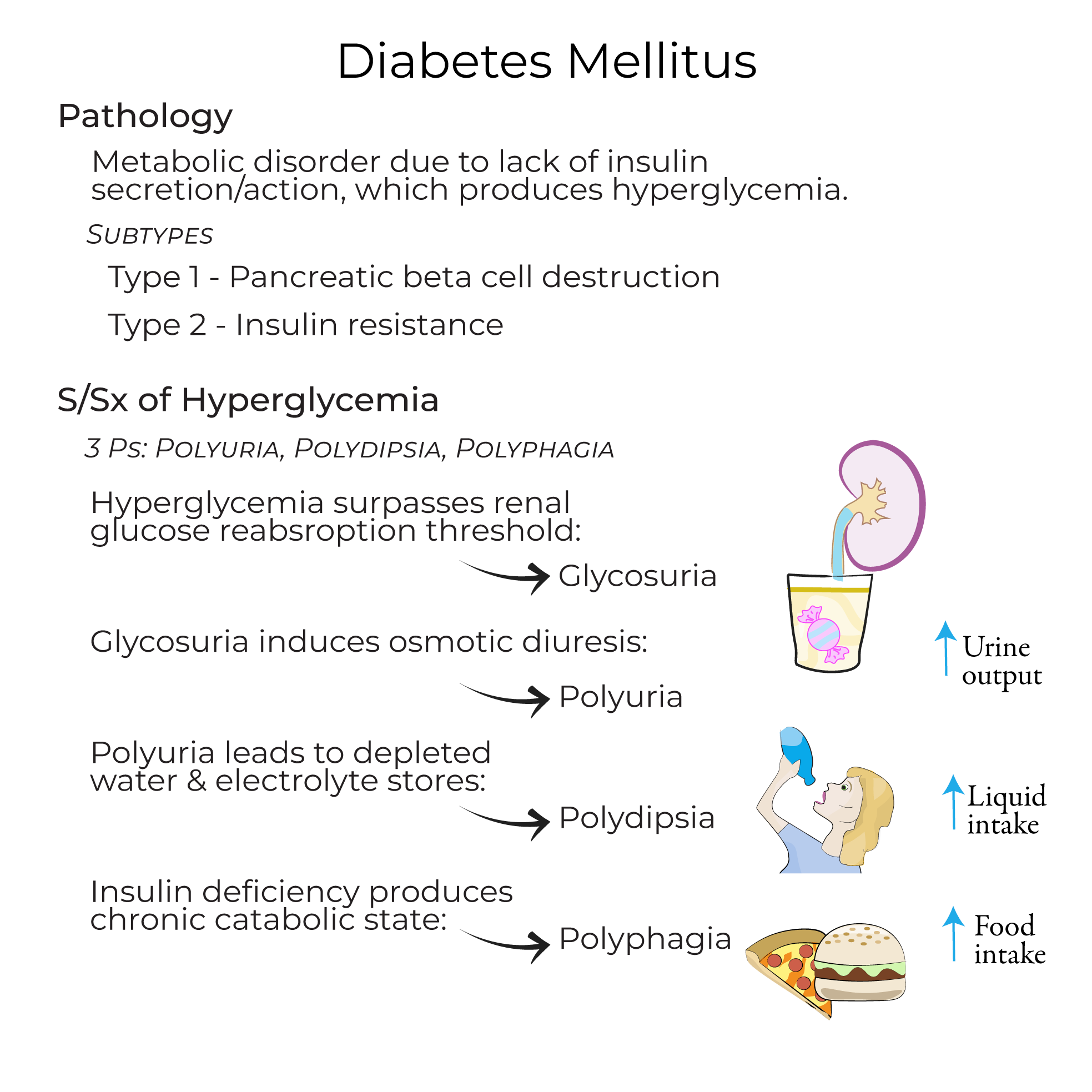
Diabetes Mellitus - Diagnosis and Clinical Overview
1. Diagnostic criteria: Random plasma glucose level of 200+ mg/dL or a fasting plasma glucose level of 126+ mg/dL.
2. Clinical impact: Chronic hyperglycemia produces dysfunction and damage of multiple organs, including the heart, kidneys, eyes, and peripheral nervous system.
3. Classical presentation: The "3 P's" - polyuria, polydipsia, and polyphagia - resulting from glycosuria, osmotic diuresis, and catabolic state, respectively.
4. Classification: Type 1, Type 2, Monogenic diabetes (including MODY), Secondary diabetes, and Gestational diabetes.
Type 1 Diabetes - Clinical Approach
1. Recognition: Type 1 accounts for 5-10% of all diabetes mellitus cases.
2. Autoimmune markers: Presence of islet autoantibodies including those targeting insulin, GAD65, ZnT8, and IA2.
3. Clinical course: Often presents in childhood with progressive reduction in insulin levels; may be misdiagnosed as Type 2 in adults.
4. Management: Requires exogenous insulin administration due to absolute insulin deficiency.
5. Complications: Susceptible to diabetic ketoacidosis when undertreated.
Type 2 Diabetes - Clinical Approach
1. Epidemiology: Represents 90-95% of all diabetes cases.
2. Risk factor assessment: Associated with obesity, central fat distribution, sedentarism, stress, and inflammation.
3. Clinical presentation: Many patients are asymptomatic with diagnosis occurring after routine blood testing.
4. Management approach: Stepwise treatment including diet and exercise, Metformin, insulin, GLP-1 receptor agonists, or SGLT2-inhibitors.
5. Acute complication: More prone to Hyperosmolar Hyperglycemic Syndrome (HHS), which has a mortality rate of up to 20%.
Prediabetes - Clinical Significance
1. Definition and screening: Condition where glucose levels are elevated but not high enough to be classified as diabetes.
2. Epidemiology: The CDC reports that 1 in 3 Americans is pre-diabetic.
3. Clinical implications: Pre-diabetic patients are at high risk for Type 2 diabetes and cardiovascular complications.
4. Management strategy: Preventive steps include increasing physical activity and losing weight.
- --
HIGH YIELD
Diabetes - Acute Complications
1. Diabetic Ketoacidosis (DKA):
- Clinical manifestations: Nausea and vomiting, fatigue, "fruity" odor, and Kussmal breathing
- Pathophysiology: Reflects the acidic state of the body, can lead to coma
- Management protocol: Fluids, electrolytes, and insulin to normalize blood glucose
- Pathophysiology: Occurs when a patient with polyuria also has deficient water intake leading to severe dehydration
- Risk factors: More common in patients unable to drink on their own (e.g., after stroke)
- Treatment approach: Requires saline, insulin, and electrolytes
Diabetes - Chronic Complications
1. Vascular Disease:
- Pathogenesis: Results from chronic hyperglycemia
- Macrovascular manifestations: Heart failure, atherosclerosis (causing myocardial infarction or stroke)
- Microvascular manifestations: Kidney damage, visual impairment, and peripheral nerve dysfunction
- Pediatric concern: Impaired growth in children
- Infectious risk: Increased susceptibility to infection due to immune suppression
- Iatrogenic complication: Hypoglycemia due to missing meals, excessive exertion, or excessive insulin administration
- Hypoglycemia symptoms: Dizziness, sweating, palpitations, and tachycardia; treated with glucose
Type 1 Diabetes - Clinical Pearls
1. Terminology note: No longer referred to as "juvenile diabetes" to avoid misdiagnosis based on age.
2. Variability in presentation: Hyperglycemia may be transient in some cases, with variable insulin needs, particularly in adults.
3. Variant awareness: Idiopathic Type 1 diabetes exists, where autoimmune response is not involved, though very rare.
Type 2 Diabetes - Management Considerations
1. Exercise benefit: Increases the number of Glut-4 receptors in skeletal muscle, improving insulin sensitivity.
2. Insulin dynamics: Initial phase often shows elevated insulin levels in response to peripheral resistance; levels eventually fall as pancreatic cells can't sustain production.
3. Treatment individualization: Therapy must be tailored to the individual and achievable glycemic targets.
4. Medication considerations: Drugs can be costly and/or have contraindications that must be considered for each patient.
5. Treatment goal: Reach glycemic targets to avoid organ damage caused by hyperglycemia.
- --
Beyond the Tutorial
Diabetes Screening and Prevention
1. USPSTF screening recommendations: Current guidelines for diabetes screening in asymptomatic adults.
2. Diabetes Prevention Program (DPP): Evidence-based strategies for preventing progression from prediabetes to diabetes.
3. Risk calculators: Tools for estimating individual risk of developing diabetes.
Management Updates
1. Current guidelines: ADA/EASD consensus on glycemic targets and management algorithms.
2. Newer medications: Cardiovascular and renal outcomes data for SGLT2 inhibitors and GLP-1 receptor agonists.
3. Technology in diabetes: Role of continuous glucose monitoring and insulin pumps in optimizing management.
Complication Assessment and Management
1. Screening protocols: Evidence-based approaches to retinopathy, nephropathy, and neuropathy screening.
2. Cardiovascular risk reduction: Multifaceted approach including statins, antihypertensives, and antiplatelet therapy.
3. Diabetic foot care: Comprehensive assessment and management of the diabetic foot to prevent ulceration and amputation.
Special Populations
1. Geriatric diabetes: Considerations for glycemic targets and medication selection in elderly patients.
2. Diabetes in pregnancy: Management approaches for pregestational and gestational diabetes.
3. Inpatient diabetes management: Protocols for glycemic control in hospitalized patients.
