USMLE/COMLEX 2 - Cardiomyopathies
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 2 & COMLEX-USA Level 2 from the Cardiomyopathies tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.

 Below is information not explicitly contained within the tutorial but important for USMLE & COMLEX 2.
Below is information not explicitly contained within the tutorial but important for USMLE & COMLEX 2.
- --
Vital for USMLE/COMLEX 2
Dilated Cardiomyopathy (DCM)
1. Presents with biventricular heart failure: dyspnea, orthopnea, PND, edema, fatigue.
2. Most common form of cardiomyopathy; often due to idiopathic, ischemic, or toxic causes (alcohol, doxorubicin).
3. Echocardiogram shows dilated LV with reduced EF (<40%) and hypokinesis.
4. S3 heart sound is often present due to volume overload.
5. Treatment follows standard HFrEF (heart failure with reduced EF) protocols:
- ACE inhibitors or ARBs
- Beta-blockers (carvedilol, metoprolol succinate, bisoprolol)
- Loop diuretics (symptom relief)
- Spironolactone, SGLT2 inhibitors, hydralazine/nitrates as indicated

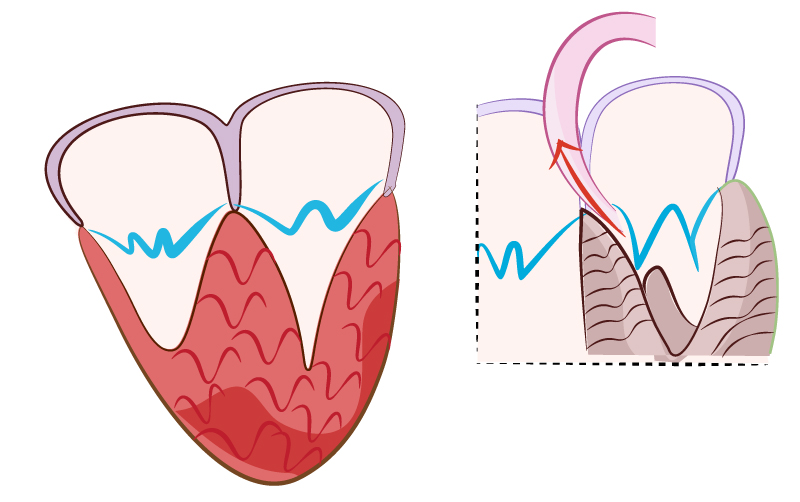
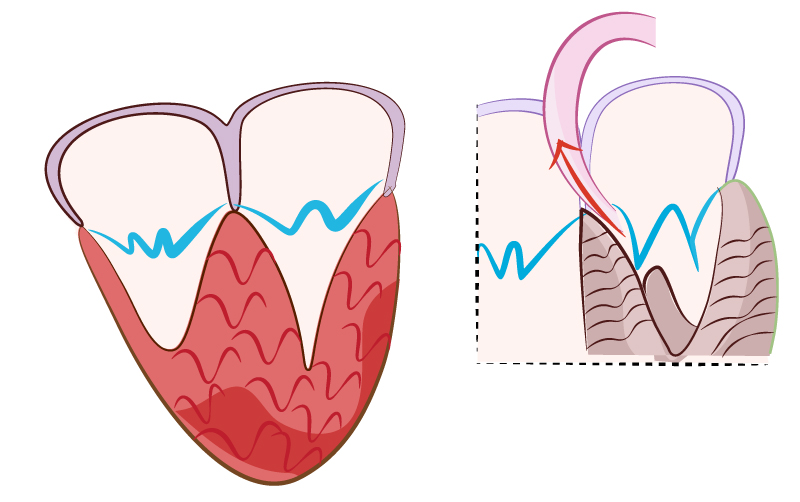
Hypertrophic Cardiomyopathy (HCM / HOCM)
1. Presents in young adults with exertional syncope, dyspnea, or chest pain.
2. Systolic ejection murmur best heard at the left lower sternal border, louder with Valsalva or standing.
3. Caused by autosomal dominant sarcomere gene mutations.
4. Diagnosis: Echocardiogram shows asymmetric septal hypertrophy with possible systolic anterior motion (SAM) of mitral valve.
5. First-line treatment is beta-blockers (or verapamil if contraindicated) to increase diastolic filling time.
6. Avoid preload-reducing agents (e.g., diuretics, nitrates, vasodilators).
7. ICD placement for high-risk features (family history of sudden death, unexplained syncope, severe LVH >30 mm, VT on Holter).
8. Patients should avoid competitive sports and dehydration.
Restrictive Cardiomyopathy (RCM)
1. Presents with right-sided heart failure symptoms: peripheral edema, hepatomegaly, ascites.
2. LV function and EF are typically preserved; diastolic dysfunction is key.
3. Causes include amyloidosis, hemochromatosis, sarcoidosis, radiation, and fibrosis.
4. ECG may show low-voltage QRS (especially in amyloidosis).
5. Echocardiogram shows normal-sized ventricles with biatrial enlargement and diastolic dysfunction.
6. In amyloidosis, confirm diagnosis with abdominal fat pad biopsy or cardiac MRI.
7. Treatment is cause-specific; consider diuretics cautiously (preload dependent).
Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC)
1. Presents with ventricular arrhythmias, palpitations, syncope, and sudden cardiac death.
2. Common in young adults, especially athletes.
3. Diagnosis via MRI, ECG (epsilon waves), and family history.
4. Managed with activity restriction, ICD placement, and antiarrhythmics.
High Yield
Dilated Cardiomyopathy (DCM)
1. Can be secondary to myocarditis (e.g., viral, post-COVID, autoimmune).
2. Alcoholic cardiomyopathy may reverse with abstinence.
3. DCM due to chemotherapy (e.g., doxorubicin) is dose-related and cumulative.
4. Consider peripartum cardiomyopathy in postpartum women with new-onset heart failure.
5. Chagas disease is an endemic cause of DCM in Latin America.
Hypertrophic Cardiomyopathy (HCM / HOCM)
1. Murmur intensity changes with preload/afterload maneuvers is a classic physical exam test item.
2. Positive family history should prompt evaluation of first-degree relatives.
3. Patients with HCM and arrhythmias or risk factors should be evaluated for ICD candidacy.
4. Apical variant HCM (Yamaguchi type) more common in some Asian populations.
Restrictive Cardiomyopathy (RCM)
1. May mimic constrictive pericarditis, but pericarditis has pericardial knock and pericardial thickening on imaging.
2. Consider hemochromatosis with signs of liver disease and diabetes.
3. Consider sarcoidosis in patients with systemic granulomatous disease or AV block.
Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC)
1. May present with T wave inversions in V1–V3 and epsilon waves.
2. Often diagnosed using the Task Force Criteria: family history, ECG, MRI, biopsy, and arrhythmia findings.
Beyond the Tutorial
Dilated Cardiomyopathy
1. LV thrombus is a known complication; anticoagulation may be indicated in high-risk patients.
2. In end-stage DCM, consider advanced therapies like LVAD or transplant.
Hypertrophic Cardiomyopathy
1. Sudden death in athletes is most often due to HCM; screening athletes is controversial but high-yield.
2. Phenylephrine (increased afterload) may be used acutely to reduce obstruction during hypotensive crises.
Restrictive Cardiomyopathy
1. In amyloidosis, a speckled or granular myocardium may be seen on echo.
2. Cardiac MRI helps distinguish infiltrative from non-infiltrative cardiomyopathy.
General Clinical Integration
1. On Step 2, distinguishing among cardiomyopathies is often done using clinical vignettes involving exercise intolerance, murmurs, heart sounds, and echocardiogram findings.
2. Know the initial step, most accurate test, and next best step in management for each condition.
