USMLE/COMLEX 2 - Atherosclerosis
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 2 & COMLEX-USA Level 2 from the Atherosclerosis Tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
- --
VITAL FOR USMLE/COMLEX 2
Clinical Presentation and Consequences
1. Atherosclerosis underlies major vascular diseases, including coronary artery disease (CAD), myocardial infarction, ischemic stroke, peripheral arterial disease (PAD), and aortic aneurysm/dissection.
2. Stable angina, acute coronary syndromes (ACS), TIA/stroke, claudication, and erectile dysfunction are common clinical manifestations.
3. Plaque rupture and thrombosis cause acute coronary events such as NSTEMI or STEMI, and embolic strokes.
4. PAD presents as intermittent claudication, diminished peripheral pulses, and can progress to critical limb ischemia.
Risk Factors and Screening
5. Major modifiable risk factors: hyperlipidemia (especially high LDL), hypertension, smoking, diabetes mellitus, and sedentary lifestyle.
6. Non-modifiable risk factors: age, male sex, family history of premature cardiovascular disease.
7. Screening includes:
- Fasting lipid panel (or non-fasting for general screening)
- Hemoglobin A1c for diabetes
- Blood pressure measurement
- CRP and coronary calcium scoring may be used selectively in intermediate-risk patients
Diagnosis and First-Line Treatment
8. Diagnosis is clinical, supported by lipid panels, risk stratification tools (e.g., ASCVD Risk Calculator), and non-invasive tests (e.g., ABI, stress tests).
9. Statins are the first-line therapy for primary and secondary prevention.
10. High-intensity statins (atorvastatin 40–80 mg or rosuvastatin 20–40 mg) are used in patients with:
- Clinical ASCVD
- LDL ≥190 mg/dL
- Age 40–75 with diabetes and LDL 70–189 mg/dL
- 10-year ASCVD risk ≥7.5%
- --
HIGH YIELD
Pathophysiology and Disease Progression
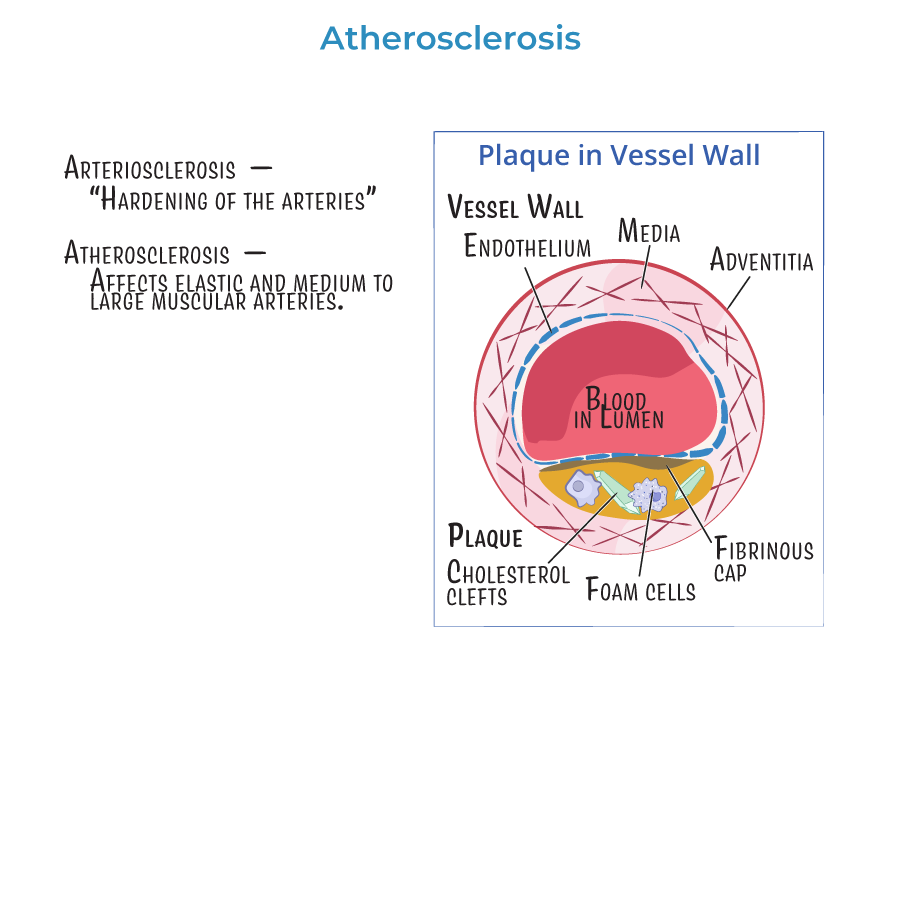
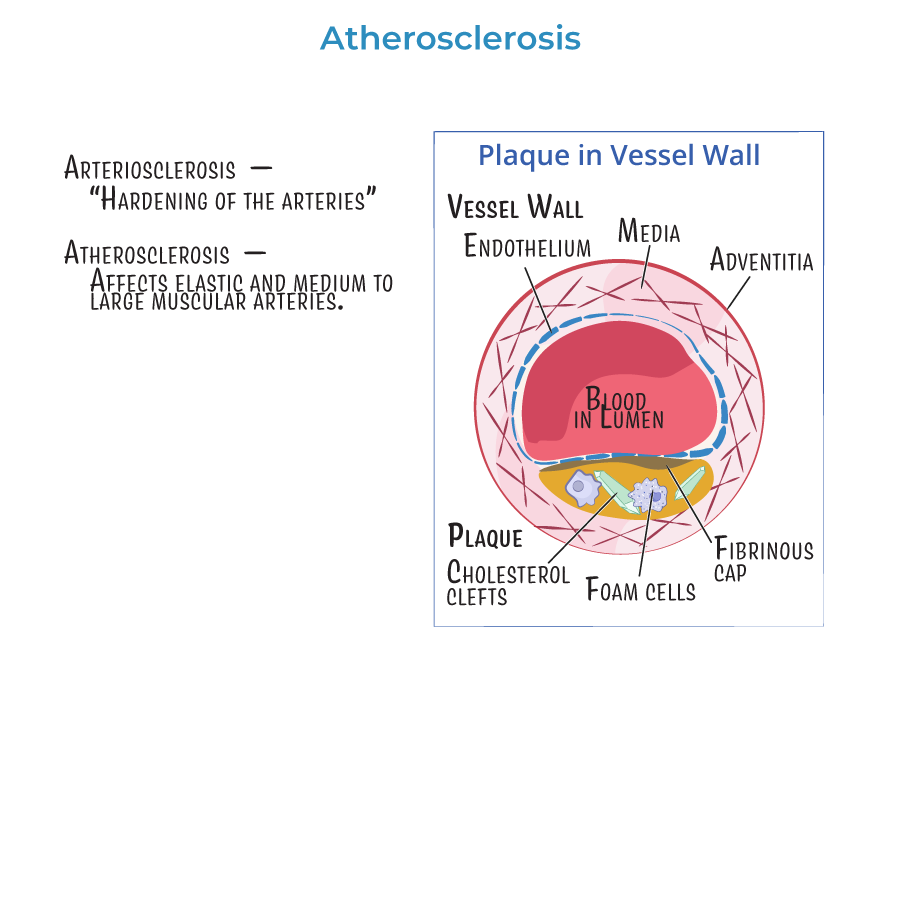
1. Atherosclerosis is triggered by endothelial injury followed by lipid deposition, macrophage activation, and chronic inflammation.
2. Fatty streaks are early lesions composed of lipid-laden macrophages; fibrous plaques are later, clinically significant stages.
3. Plaque stability depends on fibrous cap thickness and inflammatory cell activity.
4. Thin-capped plaques are more likely to rupture and thrombose, leading to acute events.
5. Foam cells, cholesterol clefts, and collagen deposition are classic histologic features.
Additional Diagnostic Considerations
6. Ankle-Brachial Index (ABI) is used to diagnose PAD (ABI <0.90 is diagnostic).
7. Coronary artery calcium (CAC) score via non-contrast CT may guide statin decisions in low-to-intermediate risk patients.
8. Carotid ultrasound can assess plaque burden in patients with stroke or high risk.
9. Doppler ultrasound and CTA/MRA can assess aortic or peripheral aneurysms.
Risk Assessment and Preventive Care
10. ASCVD 10-year risk calculator guides statin use and intensity in adults 40–75 years old.
11. Smoking cessation, blood pressure control, weight loss, and dietary counseling are essential components of long-term care.
12. Anti-platelet therapy (e.g., aspirin) is used for secondary prevention in established ASCVD.
13. Glycemic control in diabetic patients is critical to reduce atherosclerotic progression.
Medication Mechanisms
14. Statins inhibit HMG-CoA reductase, lowering cholesterol synthesis and stabilizing plaques.
15. PCSK9 inhibitors, ezetimibe, or fibrates may be added for further LDL lowering or in statin-intolerant patients.
- --
Beyond the Tutorial
Case-Based Considerations
1. In a patient with chest pain and multiple risk factors, atherosclerotic plaque rupture should be considered before ischemia from other causes.
2. Evaluate PAD in diabetic patients with foot ulcers or delayed healing using ABI and vascular imaging.
3. Erectile dysfunction may be an early sign of systemic atherosclerosis and cardiovascular disease.
4. In patients with stroke and no clear source, evaluate for carotid atherosclerosis as a potential etiology.
Clinical Scenarios
5. A patient with LDL 210 mg/dL should receive high-intensity statin therapy, regardless of 10-year risk score.
6. A 52-year-old diabetic with LDL 100 mg/dL and ASCVD risk of 12% should also start high-intensity statin.
7. A 45-year-old nonsmoking male with LDL 130 and ASCVD risk <5% may need only lifestyle changes unless other risks are present.
Follow-Up and Monitoring
8. Repeat lipid panel 4–12 weeks after starting statin, then every 6–12 months.
9. Monitor for statin side effects such as myopathy, transaminitis, and new-onset diabetes (low overall risk).
10. Evaluate response to therapy and adherence before adding other agents.
