USMLE/COMLEX 2 - Abdominal Pain
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 2 & COMLEX-USA Level 2 from the Abdominal Pain tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
- --
VITAL FOR USMLE/COMLEX 2
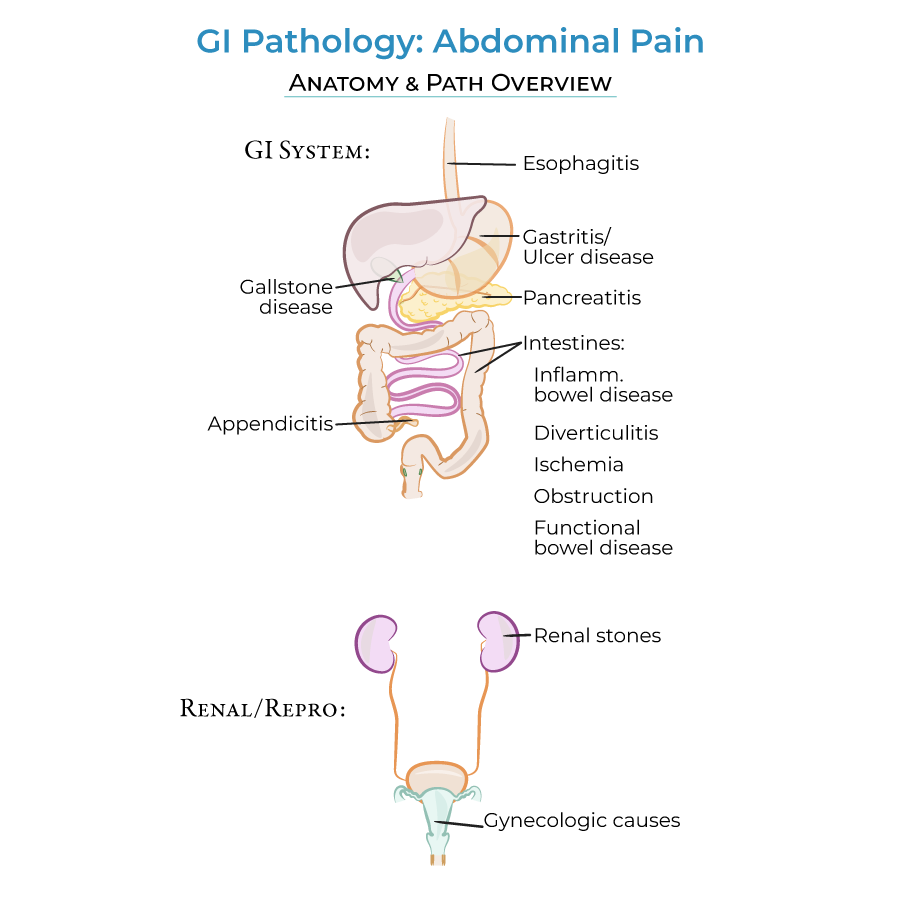
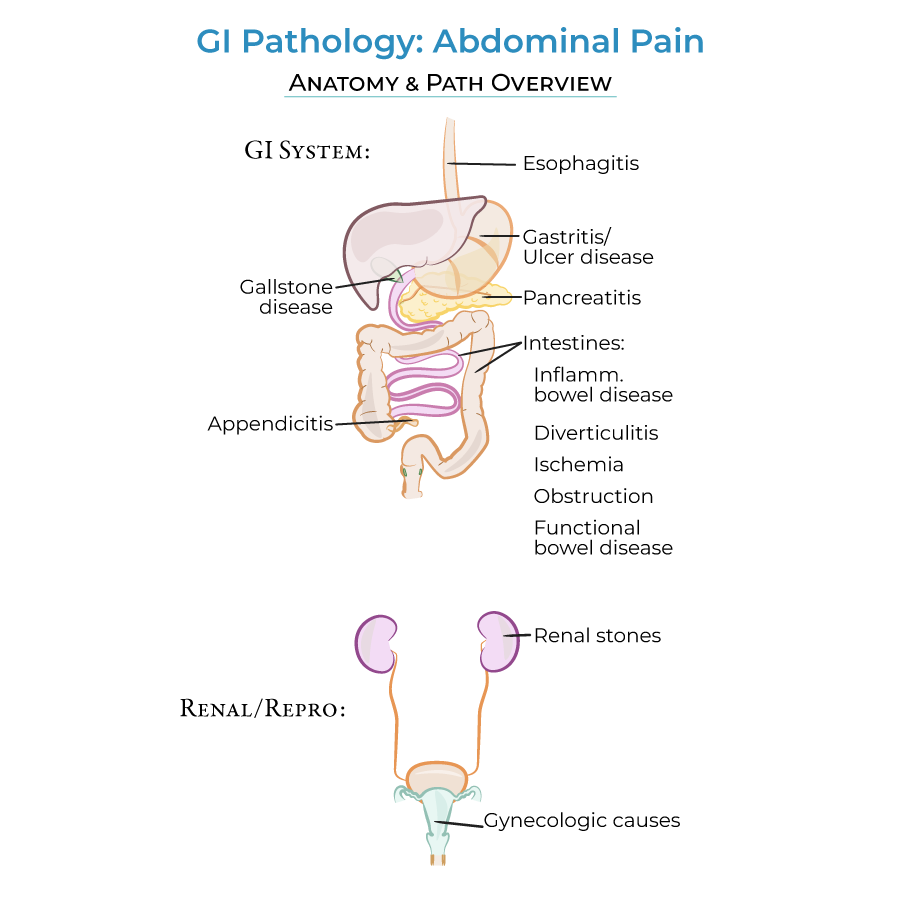
GI Causes of Abdominal Pain
1. Esophagitis: From document: Esophagitis can cause upper abdominal pain; inflammation of the esophagus is most often caused by acid reflux, medications, and eosinophilic esophagitis.
2. Gastritis and stomach ulcers: From document: Gastritis and stomach ulcers are caused by H. pylori infection, drugs, stress, and, in the case of gastritis, autoimmune dysfunction.
3. GI strictures and obstruction: From document: GI strictures and obstruction are caused by hernias, adhesions, volvulus, tumors, inflammatory narrowing, foreign bodies, and fecal impaction.
4. Diverticulitis: From document: Diverticulitis occurs when there is inflammation (often with bacterial infection) in diverticula, which are pouch-like outcroppings of the intestinal wall.
5. Intestinal ischemia: From document: Intestinal ischemia can be the result of systemic hypotension, atherosclerosis, blood clots, and constricting fibrosis or strictures that inhibit blood flow.
6. Inflammatory bowel disease: From document: Inflammatory bowel disease comprises the chronic/remitting autoimmune disorders Crohn's disease and ulcerative colitis.
7. Functional bowel disorders: From document: Functional bowel disorders (FBDs) are characterized by disordered brain-gut interactions. The most common FBD is Irritable bowel syndrome.
Accessory Organ and Non-GI Causes
1. Pancreatitis: From document: Pancreatitis is the result of bile duct stones, alcohol abuse, and/or cigarette smoking.
2. Gallstone disease: From document: Gallstone disease causes pain in the right upper abdominal quadrant; we can remember this, because the gallstones get stuck in the biliary system, which is towards the right side of the abdomen.
3. Appendicitis: From document: Appendicitis often presents early on with pain in the peri-navel area that later moves to the right lower abdominal quadrant (where we find the appendix).
4. Kidney stones: From document: Kidney stones cause "flank" pain – pain in the side of the torso; pain can travel to the groin area, too.
5. Gynecological causes: From document: Gynecological causes include: ruptured ovarian cysts, pelvic inflammatory disease, ectopic pregnancy, and endometriosis – essentially, anything that causes inflammation and swelling of the uterus or ovaries can cause lower abdominal and back pain.
- --
HIGH YIELD
GI Causes of Abdominal Pain
1. Esophagitis: From document: Treatments include proton pump inhibitors to reduce acid production by the stomach.
2. Gastritis and stomach ulcers: From document: Inflammation can travel up and down the esophagus to and from the stomach. Treatments include proton pump inhibitors, antacids, H2 blockers, and prostaglandins.
3. GI strictures and obstruction: From document: In our diagram, we show scar tissue adhesions that formed after abdominal surgery; adhesions bind and restrict the intestinal tract, which obscures movement of materials.
4. Intestinal ischemia: From document: Ischemia is more common in the intestines than in the stomach or esophagus. Surgery and/or medications to restore blood flow are prescribed.
5. Inflammatory bowel disease: From document: Patients often experience diarrhea in addition to abdominal cramping and other symptoms. In ulcerative colitis, the diarrhea is frequently bloody. Anti-inflammatories and immune suppressors are often prescribed.
6. Functional bowel disorders: From document: Etiologies are uncertain, but are thought to include infection and/or psychosocial causes.
Accessory Organ and Non-GI Causes
1. Pancreatitis: From document: Early/acute pancreatitis is characterized by elevated serum amylase and lipase levels. Late/chronic pancreatitis can result in loss of endocrine and exocrine functions (i.e., patients have diabetes mellitus, etc.). Pancreatitis causes epigastric pain that radiates towards the back.
2. Gallstone disease: From document: Gallstone disease causes pain in the right upper abdominal quadrant; we can remember this, because the gallstones get stuck in the biliary system, which is towards the right side of the abdomen.
3. Appendicitis: From document: Appendicitis often presents early on with pain in the peri-navel area that later moves to the right lower abdominal quadrant (where we find the appendix).
4. Abdominal quadrants: From document: Abdominal quadrants - Understanding the relationship between pain location and underlying organ systems is essential for diagnosis.
- --
Beyond the Tutorial
Clinical Assessment and Diagnosis
1. History taking for abdominal pain: Key questions that differentiate urgent from non-urgent causes.
2. Physical examination techniques: Specialized maneuvers to elicit specific signs (e.g., Murphy's sign, McBurney's point tenderness, psoas sign).
3. Laboratory workup: Stepwise approach to ordering and interpreting relevant labs.
4. Advanced imaging: Indications for and limitations of ultrasound, CT, MRI, MRCP, and ERCP.
5. Approach to special populations: Pregnant patients, elderly, immunocompromised.
Management Principles
1. Triage and initial stabilization: Decision trees for abdominal pain in emergency settings.
2. Medical versus surgical management: Evidence-based algorithms for common conditions.
3. Pain management strategies: Appropriate analgesic selection without masking physical findings.
4. Post-intervention monitoring: Key parameters to follow during treatment course.
5. Disposition planning: Criteria for admission versus outpatient management.
Complications and Follow-up
1. Red flags for deterioration: Signs requiring urgent reassessment.
2. Recurrence prevention: Condition-specific strategies to prevent relapse.
3. Long-term sequelae: Managing chronic complications of acute abdominal conditions.
4. Consultation timing: When to involve specialists (gastroenterology, surgery, gynecology).
5. Patient education: Essential discharge teaching points by condition.
