Interstitial Lung Diseases for USMLE Step 1
Start your One-Week Free Trial
Already subscribed? Log in »
Interstitial Lung Diseases for the USMLE Step 1 Exam
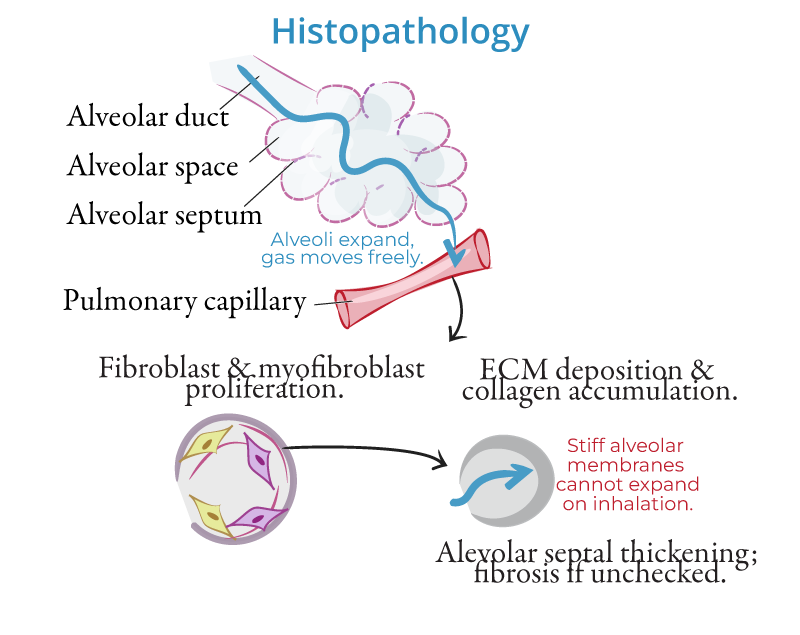
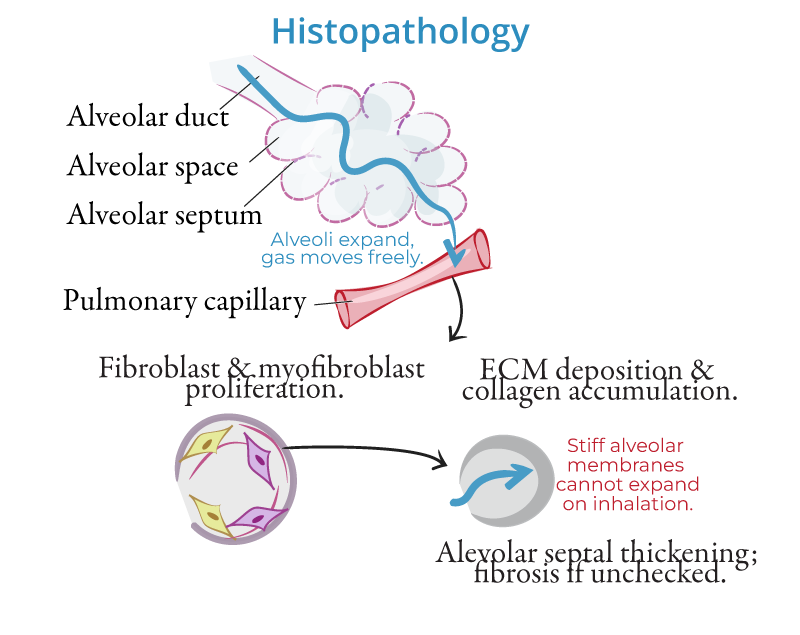
Pathophysiology
- Chronic Inflammation and Fibrosis:
- Interstitial lung diseases (ILDs) involve inflammation and fibrosis of the lung interstitium, the tissue between the alveoli. The process is often initiated by injury from toxins, drugs, or autoimmune mechanisms, leading to repeated cycles of inflammation and abnormal wound healing, resulting in fibrosis. This fibrosis thickens the alveolar walls, restricting gas exchange and causing progressive respiratory impairment.
- Mechanisms of Damage:
- In many ILDs, repeated injury to the alveoli triggers an aberrant repair response. Fibroblasts and myofibroblasts are activated, producing excessive collagen and extracellular matrix, leading to scarring. Inflammatory mediators, such as cytokines (IL-1, TNF-α), play a critical role in sustaining inflammation and promoting fibrosis.
Etiologies
- Idiopathic Pulmonary Fibrosis (IPF):
- The most common and aggressive form of ILD, characterized by progressive fibrosis with no known cause. It typically affects older adults and is associated with a poor prognosis. The hallmark histologic pattern is usual interstitial pneumonia (UIP).
- Pneumoconioses:
- Caused by inhalation of inorganic dusts that lead to chronic lung injury. Common types include:
- Asbestosis: Associated with asbestos exposure, often seen in construction and shipyard workers.
- Silicosis: Results from inhaling silica dust, commonly affecting miners and stone workers.
- Coal Workers' Pneumoconiosis: Also known as "black lung," caused by coal dust exposure.
- Hypersensitivity Pneumonitis (HP):
- An immune-mediated condition triggered by inhalation of organic antigens, such as bird droppings (bird fancier's lung) or moldy hay (farmer's lung). It leads to granulomatous inflammation and, with chronic exposure, fibrosis.
- Sarcoidosis:
- A multisystem granulomatous disorder that frequently affects the lungs. The exact cause is unknown, but it results in the formation of noncaseating granulomas in the lung parenchyma, which can eventually lead to fibrosis in chronic cases.
- Connective Tissue Diseases:
- ILD can occur as a complication of autoimmune disorders, including:
- Rheumatoid arthritis (RA): Can cause interstitial lung involvement.
- Systemic sclerosis (scleroderma): Leads to widespread fibrosis, including in the lungs.
- Polymyositis/Dermatomyositis: These inflammatory myopathies can lead to interstitial lung disease.
- Drug-Induced ILD:
- Certain medications can induce lung injury, including:
- Amiodarone: A common antiarrhythmic drug that can cause pulmonary fibrosis.
- Bleomycin: A chemotherapy agent known for causing pulmonary toxicity.
Clinical Features
- Dyspnea:
- Progressive shortness of breath, especially during exertion, is the most common symptom in ILD.
- Dry Cough:
- A persistent, nonproductive cough often accompanies dyspnea and worsens as the disease progresses.
- Crackles:
- Fine, Velcro-like inspiratory crackles, particularly at the lung bases, are commonly heard on auscultation.
- Clubbing:
- Digital clubbing may be present in advanced stages of ILD, particularly in idiopathic pulmonary fibrosis (IPF).
- Extrapulmonary Features:
- In connective tissue disease-associated ILD, patients may present with systemic symptoms like joint pain, skin changes, or muscle weakness (e.g., in rheumatoid arthritis or scleroderma).
Diagnosis
- High-Resolution CT (HRCT):
- The gold standard imaging tool for diagnosing ILD. Findings include:
- Ground-glass opacities: Indicating active inflammation.
- Honeycombing: Indicative of advanced fibrosis, especially in IPF.
- Reticular opacities: Representing fibrosis in the interstitial space.
- Pulmonary Function Tests (PFTs):
- Reveal a restrictive pattern, with decreased total lung capacity (TLC) and forced vital capacity (FVC). Diffusion capacity for carbon monoxide (DLCO) is reduced, reflecting impaired gas exchange.
- Biopsy:
- A lung biopsy may be required in cases where the diagnosis is unclear or in patients with atypical presentations. Biopsy helps to differentiate between various subtypes of ILD, such as UIP in IPF or granulomatous inflammation in sarcoidosis.
- Serologic Testing:
- Blood tests may help identify autoimmune causes of ILD, such as rheumatoid factor (RF), antinuclear antibodies (ANA), and anti-cyclic citrullinated peptide (anti-CCP) in connective tissue disease-associated ILD.
Management
General Approach
- Smoking Cessation:
- Smoking exacerbates lung damage and is particularly harmful in patients with ILD, such as those with asbestosis or IPF.
- Avoidance of Triggers:
- In hypersensitivity pneumonitis, avoiding exposure to known antigens (e.g., birds, mold) is essential to prevent disease progression.
- Oxygen Therapy:
- Patients with advanced disease and hypoxemia benefit from supplemental oxygen, particularly during exertion and sleep.
Pharmacologic Therapy
- Idiopathic Pulmonary Fibrosis (IPF):
- Antifibrotic agents such as pirfenidone and nintedanib have been shown to slow the progression of fibrosis in IPF but do not reverse the disease.
- Corticosteroids and Immunosuppressants:
- Corticosteroids (e.g., prednisone) are the mainstay of treatment in inflammatory ILDs, such as sarcoidosis or hypersensitivity pneumonitis. In more severe cases, immunosuppressants like methotrexate, azathioprine, or mycophenolate may be added.
- Antibiotics:
- In cases of organizing pneumonia or chronic infections contributing to ILD, long-term antibiotics like doxycycline or macrolides may be used.
Surgical Therapy
- Lung Transplantation:
- Reserved for patients with end-stage ILD who fail to respond to medical therapy. Lung transplantation offers a survival benefit in carefully selected patients with advanced disease.
Supportive Care
- Pulmonary Rehabilitation:
- Exercise training and education help improve exercise tolerance and quality of life in patients with ILD.
- Vaccinations:
- Influenza and pneumococcal vaccines are recommended to reduce the risk of respiratory infections, which can exacerbate ILD.
Key Points
- Interstitial lung diseases (ILDs) are a group of disorders involving chronic inflammation and fibrosis of the lung interstitium, leading to impaired gas exchange and restrictive lung disease.
- Common causes of ILD include idiopathic pulmonary fibrosis (IPF), pneumoconioses (asbestosis, silicosis), hypersensitivity pneumonitis, sarcoidosis, and connective tissue diseases.
- HRCT is the diagnostic gold standard, with key findings such as ground-glass opacities and honeycombing, while pulmonary function tests reveal a restrictive pattern.
- Treatment depends on the cause and includes antifibrotic agents for IPF, corticosteroids for inflammatory ILDs, and lung transplantation for advanced cases.
- Early detection and management are critical to slowing disease progression and improving quality of life in patients with ILD.
