Hemophilia for the USMLE Step 1
Start your One-Week Free Trial
Already subscribed? Log in »
Hemophilia for the USMLE Step 1 Exam
- Definition:
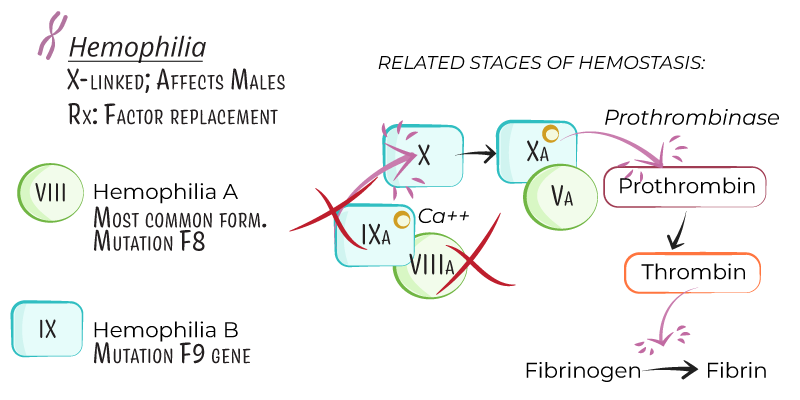
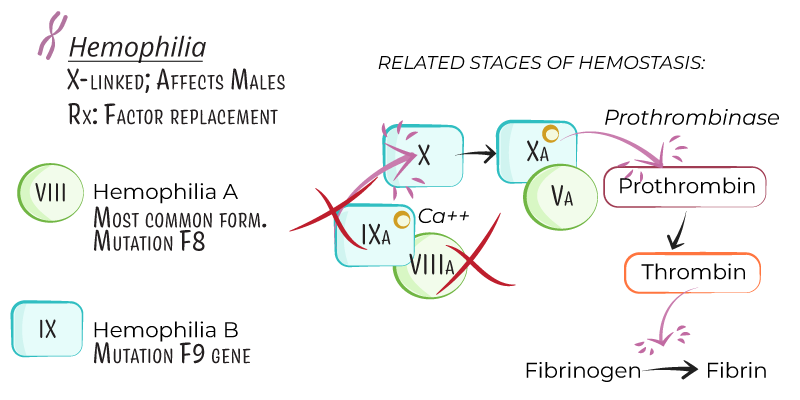
- Hemophilia is an X-linked recessive bleeding disorder due to a deficiency of specific clotting factors, which leads to impaired blood clotting and prolonged bleeding.
- Primarily affects males, with females as carriers, although some females may exhibit mild symptoms due to skewed X-chromosome inactivation.
- Types:
- Hemophilia A: Factor VIII deficiency, accounting for approximately 80% of cases.
- Hemophilia B (Christmas Disease): Factor IX deficiency, representing around 20% of cases.
Genetics and Pathophysiology
- Inheritance:
- Both hemophilia A and B are X-linked recessive, affecting mostly males.
- Carrier females have a 50% chance of passing the gene to sons (affected) and daughters (carriers).
- Pathogenesis:
- Factor VIII (hemophilia A) and factor IX (hemophilia B) are part of the intrinsic coagulation pathway and are necessary for activation of factor X, leading to thrombin generation and fibrin clot formation.
- Deficiency of these factors disrupts the intrinsic pathway, prolonging bleeding time and impairing clot stability.
- Severity:
- Severe: Factor activity <1% of normal, associated with spontaneous bleeding episodes.
- Moderate: Factor activity 1–5% of normal, with bleeding after minor trauma.
- Mild: Factor activity 5–40% of normal, with bleeding typically only after significant trauma or surgery.
Clinical Presentation
- Common Bleeding Sites:
- Hemarthrosis: Recurrent bleeding into joints (knees, elbows, ankles) is a hallmark of severe hemophilia, leading to joint deformity if untreated.
- Muscle Bleeding: Bleeding into deep muscles, such as thigh or iliopsoas, which may cause compartment syndrome if not managed.
- Mucosal Bleeding: Bleeding from gums or nasal trauma, though less common than in von Willebrand disease.
- Intracranial Hemorrhage: Rare but can occur after minor trauma, making head injuries a particular concern.
- Post-Traumatic or Post-Surgical Bleeding:
- Extended bleeding after minor procedures or trauma, especially in mild and moderate hemophilia, may delay diagnosis.
Diagnosis
- Laboratory Tests:
- Complete Blood Count (CBC): Typically normal but may show anemia if significant bleeding has occurred.
- Prothrombin Time (PT): Normal, as PT measures the extrinsic pathway unaffected by factor VIII or IX deficiencies.
- Activated Partial Thromboplastin Time (aPTT): Prolonged due to defects in the intrinsic pathway.
- Specific Factor Assays: Factor VIII and IX levels confirm the diagnosis and determine the severity of hemophilia.
- Genetic Testing:
- Useful for identifying carriers and for prenatal diagnosis, particularly in families with a known history of hemophilia.
Treatment
- Factor Replacement Therapy:
- Factor VIII Concentrate (Hemophilia A) and Factor IX Concentrate (Hemophilia B):
- On-Demand: Administered during active bleeding episodes.
- Prophylactic: Regular infusions to prevent bleeding, particularly in severe hemophilia, helping to prevent joint damage.
- Dosing: Based on body weight, severity, and specific bleeding episode or surgical need.
- Extended Half-Life (EHL) Products:
- Recombinant factor products with extended half-lives are available, allowing for less frequent dosing in prophylactic treatment.
- Bypassing Agents for Inhibitors:
- Recombinant Factor VIIa (rFVIIa) and Activated Prothrombin Complex Concentrate (aPCC): Used in patients who develop inhibitors (antibodies) against factor VIII or IX.
- Emicizumab:
- Mechanism: A bispecific antibody mimicking factor VIII function, allowing effective clot formation in hemophilia A patients, even with inhibitors.
- Administration: Subcutaneous injection, typically given weekly or biweekly.
- Adjunct Therapies:
- Antifibrinolytics (e.g., tranexamic acid, aminocaproic acid): Helpful in mucosal bleeding and dental procedures.
- Pain Management: Prefer acetaminophen over NSAIDs to avoid platelet inhibition.
Key Points
- Hemophilia is an X-linked recessive disorder due to deficiencies in factor VIII (hemophilia A) or factor IX (hemophilia B), primarily affecting males.
- Classification by severity (severe, moderate, mild) depends on factor activity level, with severe hemophilia often presenting with spontaneous joint and muscle bleeds.
- Diagnosis includes prolonged aPTT, specific factor assays, and genetic testing for carrier identification.
- Treatment involves on-demand or prophylactic factor replacement therapy, bypassing agents for inhibitor patients, and emicizumab in hemophilia A.
- Complications include joint deformities from recurrent hemarthrosis, the development of inhibitors to factor therapy, and increased risk of bleeding in trauma or surgical procedures.
