Asthma for USMLE Step 1
Start your One-Week Free Trial
Already subscribed? Log in »
Asthma for the USMLE Step 1 Exam
Pathophysiology
- Chronic Inflammation:
- Asthma is a chronic inflammatory disorder of the airways involving eosinophils, mast cells, and T-helper 2 (Th2) cells. Inflammatory mediators such as histamine, leukotrienes, and prostaglandins contribute to airway edema and mucus production.
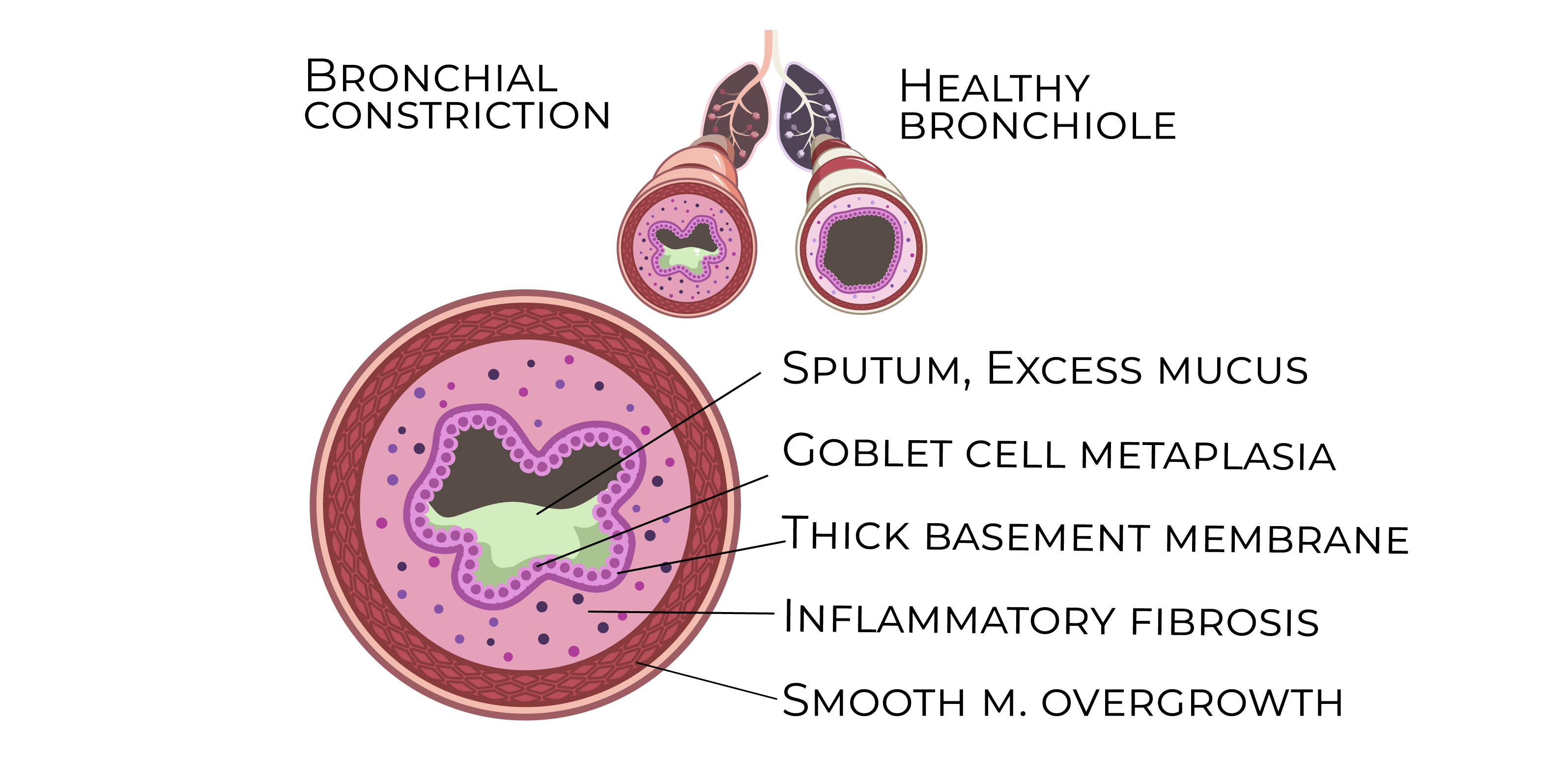
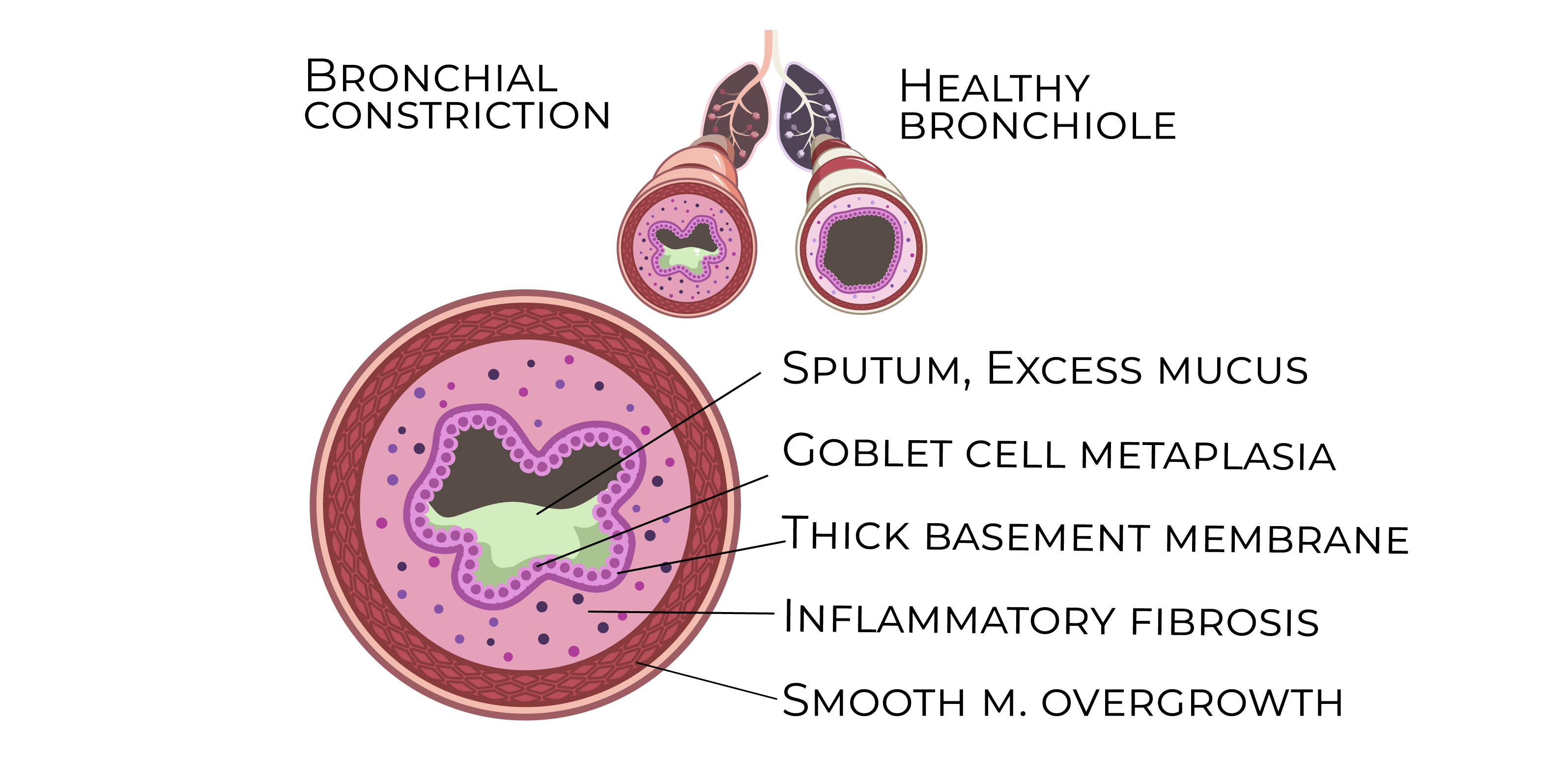
- This leads to bronchoconstriction, airway hyperresponsiveness, and structural changes in chronic cases.
- Airway Hyperresponsiveness:
- Airway smooth muscles overreact to stimuli like allergens, infections, exercise, or cold air, resulting in reversible bronchoconstriction.
- Airway Remodeling:
- Over time, chronic inflammation causes thickening of the airway wall, smooth muscle hypertrophy, goblet cell hyperplasia, and subepithelial fibrosis. This leads to more fixed airflow limitation in severe or poorly managed cases.
- Immunologic Mechanisms:
- Asthma often involves a Th2-mediated immune response. Allergens stimulate the production of IgE, which binds to mast cells and triggers degranulation, releasing inflammatory mediators such as histamine.
Risk Factors
- Genetics:
- A family history of asthma or other atopic diseases (e.g., eczema, allergic rhinitis) increases the risk.
- Environmental Triggers:
- Common asthma triggers include allergens (pollen, dust mites, mold, animal dander), respiratory infections (especially viral), air pollution, tobacco smoke, and cold air.
- Atopy:
- Atopic individuals are more likely to develop asthma due to a predisposition to produce IgE in response to common allergens.
Clinical Features
- Wheezing:
- Expiratory wheezing is the classic symptom of asthma, often triggered by exercise, allergens, or respiratory infections.
- Dyspnea:
- Shortness of breath that is typically episodic, occurring more frequently at night or in the early morning.
- Cough:
- A dry, nonproductive cough may be a prominent symptom, especially at night.
- Chest Tightness:
- Patients often describe a sensation of chest tightness, particularly during exacerbations or after exposure to triggers.
- Exacerbations:
- Acute worsening of symptoms, often triggered by respiratory infections, allergens, or physical activity.
Diagnosis
- Spirometry:
- The main diagnostic tool showing:
- Decreased FEV1 and FEV1/FVC ratio: Indicates obstructive airway disease.
- Reversibility of obstruction: An increase in FEV1 by at least 12% and 200 mL after bronchodilator use confirms the diagnosis.
- Methacholine Challenge Test:
- For patients with normal spirometry but suspected asthma, this test induces bronchoconstriction. A significant reduction in FEV1 confirms airway hyperreactivity.
- Peak Expiratory Flow (PEF):
- PEF measurements help monitor asthma control and detect early signs of worsening.
Management
- Stepwise Approach:
- Intermittent Asthma (Step 1):
- Short-acting beta-agonists (SABAs) like albuterol are used as needed for symptom relief.
- Mild Persistent Asthma (Step 2):
- Low-dose inhaled corticosteroids (ICS) are the first-line therapy for maintenance.
- Moderate Persistent Asthma (Step 3):
- Combination therapy with low-dose ICS + long-acting beta-agonists (LABAs) is preferred.
- Severe Asthma (Step 4 and above):
- High-dose ICS + LABA may be required. Additional therapies like tiotropium or biologics (e.g., omalizumab) can be used in severe cases.
- Acute Exacerbation Management:
- SABAs: First-line therapy for relief of bronchospasm.
- Systemic Corticosteroids: Oral prednisone is used to reduce inflammation during moderate-to-severe exacerbations.
- Oxygen: Administered to maintain SpO2 >90% in patients with severe exacerbations.
Complications
- Status Asthmaticus:
- A severe, life-threatening exacerbation that does not respond to standard treatment, often requiring intensive care and mechanical ventilation.
- Airway Remodeling:
- Repeated poorly controlled inflammation may lead to permanent changes in airway structure, causing fixed airflow limitation.
- Pneumothorax:
- Rare but can occur in severe exacerbations, especially with excessive use of bronchodilators.
Key Points
- Asthma is a chronic inflammatory disorder involving airway hyperresponsiveness and bronchoconstriction, often triggered by allergens, respiratory infections, or exercise.
- Diagnosis is confirmed by spirometry, showing reversible airflow obstruction (FEV1/FVC ratio improvement with bronchodilator use).
- Management is based on a stepwise approach, starting with SABAs for intermittent asthma and escalating to ICS, LABAs, and biologics for persistent disease.
- Acute exacerbations are treated with SABAs, systemic corticosteroids, and oxygen in severe cases.
- Complications include status asthmaticus and airway remodeling, which can lead to permanent airflow limitation if not controlled.
