USMLE/COMLEX 1 - Valvular Disease
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 1 & COMLEX-USA Level 1 from the Valvular Disease tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
1. Valvular Dysfunction Types
 3. Bicuspid Aortic Valve
1. Semilunar Valve Components
3. Bicuspid Aortic Valve
1. Semilunar Valve Components
 2. Pathophysiology of Valve Degeneration
1. Rheumatic Fever and Heart Disease
2. Pathophysiology of Valve Degeneration
1. Rheumatic Fever and Heart Disease
- --
VITAL FOR USMLE/COMLEX 1
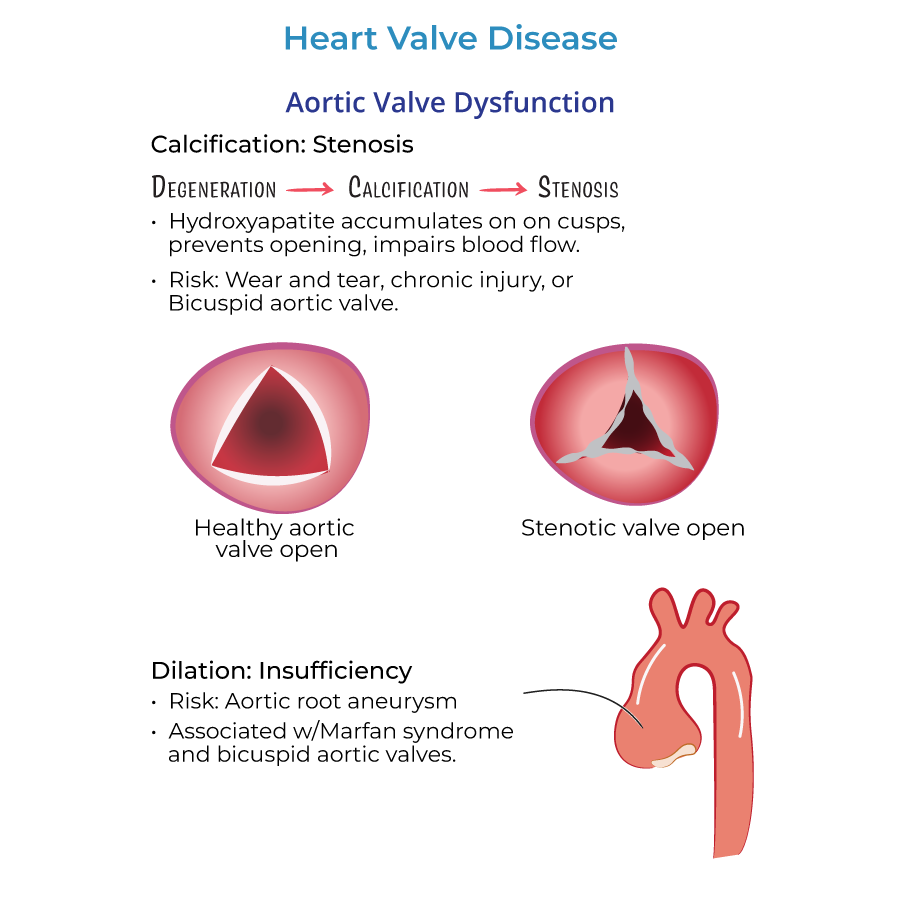
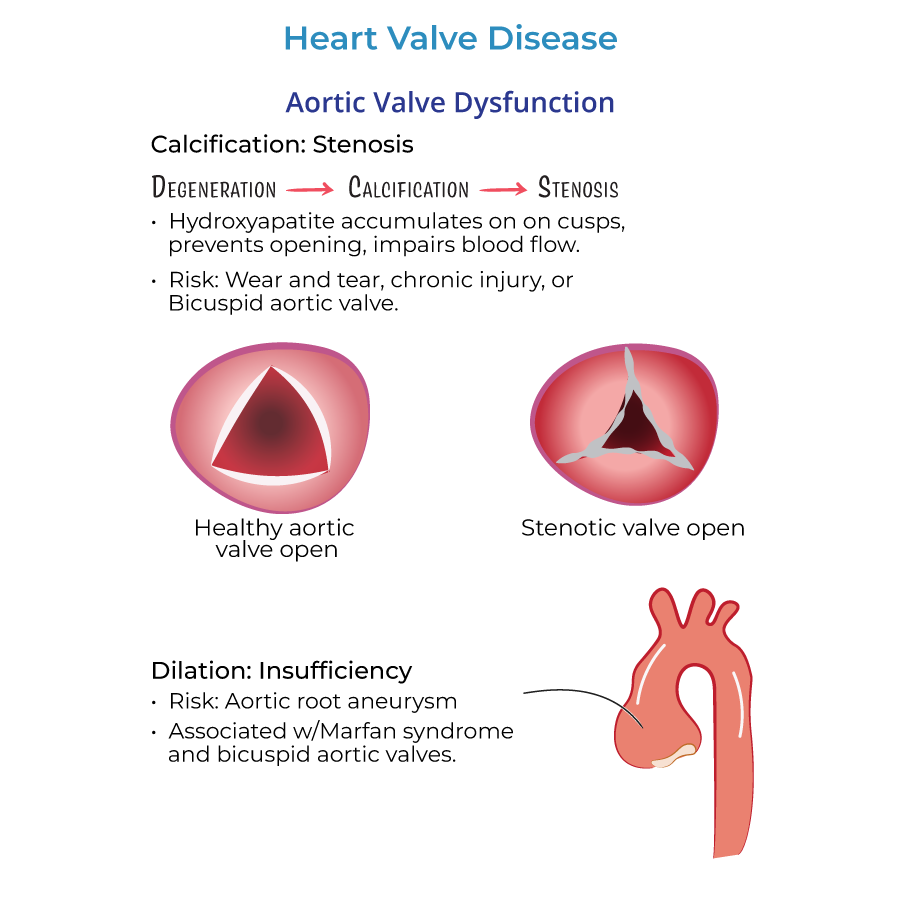
- Stenosis = obstruction of valve orifice.
- Insufficiency/Regurgitation = incomplete closure of valve, leading to backward blood flow.
- Most common valvular disorder in developed countries.
- Caused by calcific degeneration due to hydroxyapatite deposition.
- Risk factors: bicuspid aortic valve, age-related wear, hyperlipidemia, hypertension, atherosclerosis.
- Involves osteoblast-like cells; similar to bone formation.
 3. Bicuspid Aortic Valve
3. Bicuspid Aortic Valve
- Congenital defect in \~1% of the population.
- Increased risk of aortic stenosis due to greater mechanical stress.
- Associated with Turner syndrome and aortic aneurysms.
- Often due to aortic root dilation (e.g., from Marfan syndrome or hypertension).
- Leads to volume overload of the left ventricle and widened pulse pressure.
- May be asymptomatic for years but can lead to left ventricular dilation and heart failure.
- Most common valvular abnormality in the U.S.
- Often due to myxomatous degeneration of leaflets.
- Causes midsystolic click followed by a late systolic murmur.
- Complications: endocarditis, arrhythmias, stroke due to embolism.
- Strongly associated with rheumatic heart disease.
- Histology: vegetations along the free edge, fusion of chordae tendineae.
- Classic "button hole" or "fish mouth" appearance.
- Results in left atrial dilation and predisposes to atrial fibrillation and thromboembolism.
- Mechanical valves: durable but require lifelong anticoagulation (e.g., warfarin).
- Bioprosthetic valves: less thrombogenic but prone to deterioration.
- Risk of infective endocarditis elevated in both; antibiotic prophylaxis indicated for high-risk procedures.
- Crucial for AV valve function.
- Damage can cause functional regurgitation without primary valve disease (e.g., after MI involving papillary muscles).
- A connective tissue disorder causing dilation of the aortic root and increasing risk for aortic regurgitation, dissection, and rupture.
- Involves inflammation/infection of heart valves.
- Most common on left-sided valves (mitral > aortic).
- Predisposed by damaged valves, prosthetic valves, and dental procedures (hence need for prophylactic antibiotics).
- Occur in up to 60% of patients within 10 years.
- Include leakage, thromboembolism, and infective endocarditis.
- Typically affects annular ring, not leaflets.
- Leads to arrhythmias, stroke, and increased endocarditis risk.
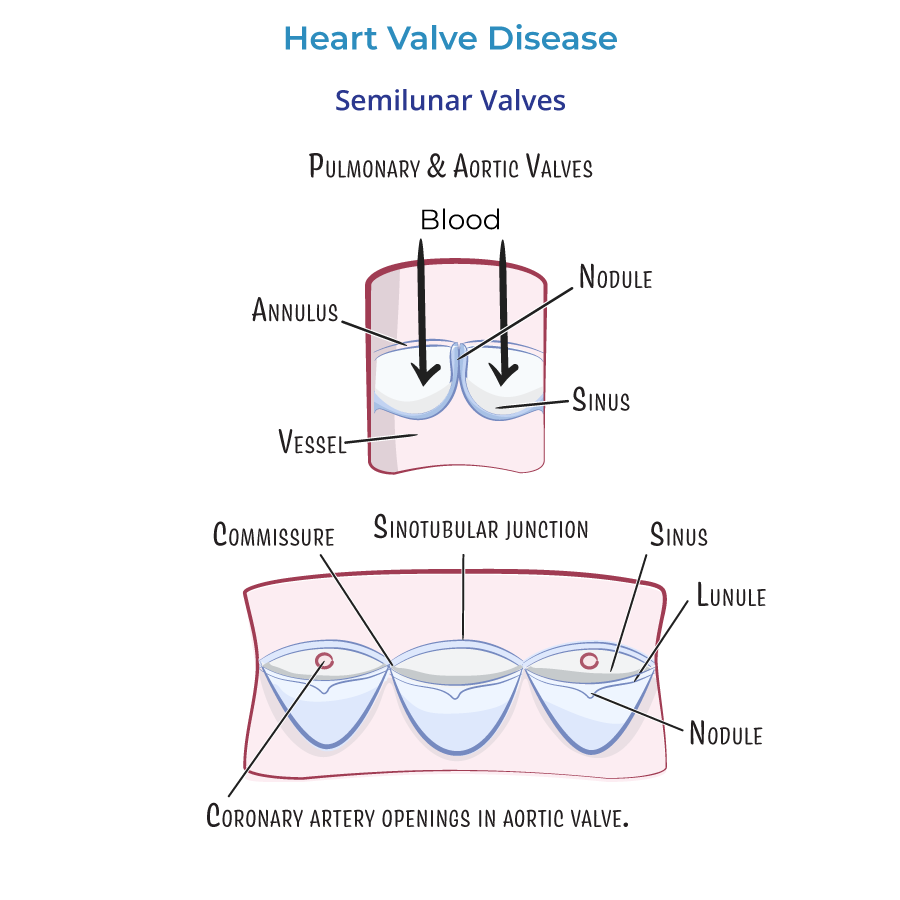
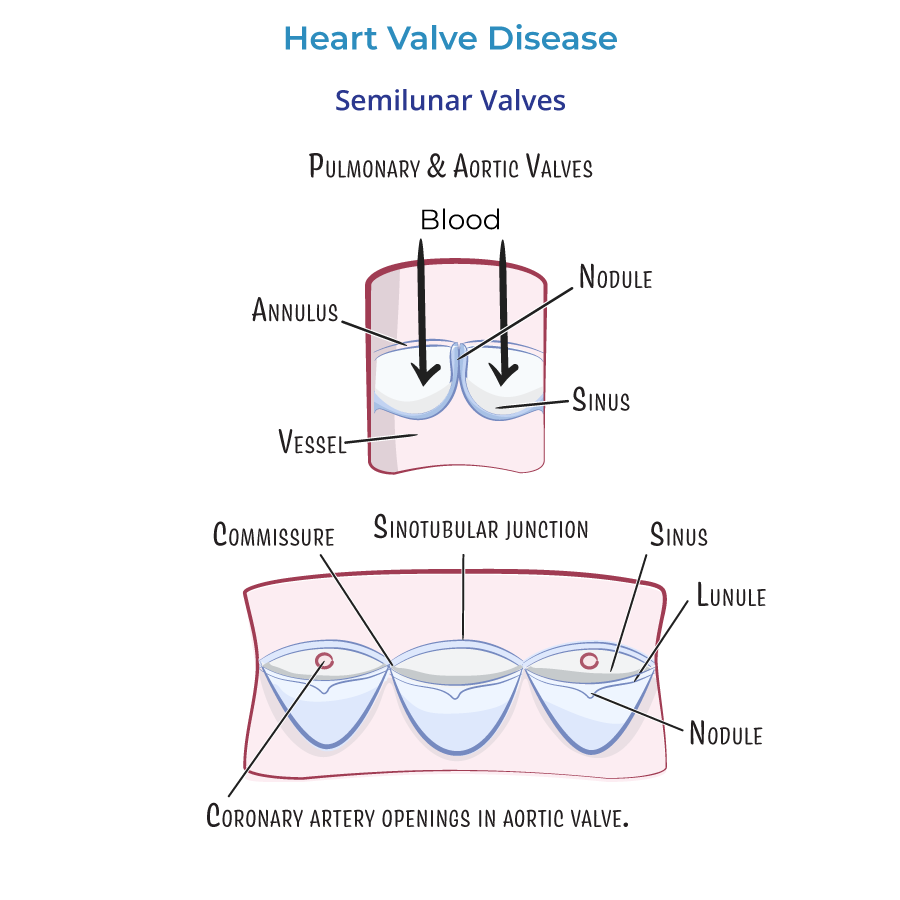
- Aortic valve has right coronary, left coronary, and posterior non-coronary leaflets.
- Coronary arteries arise from aortic sinuses near these leaflets.
- Mitral valve: anterior and posterior cusps.
- Tricuspid valve: anterior, posterior, and septal leaflets.
- Anchored by chordae tendineae to papillary muscles.
- Fibrous ring anchoring valve to myocardium.
- Pathology here affects valve competence and is a key site for calcification.
- --
HIGH YIELD
- Lunule = thin edge of leaflet.
- Nodule of Arantius = thickened center of lunule for tight closure.
- Commissures = leaflet attachments.
- Sinotubular junction = transition from aortic sinus to ascending aorta.
 2. Pathophysiology of Valve Degeneration
2. Pathophysiology of Valve Degeneration
- Resembles bone formation due to osteoblast-like cells.
- Influenced by mechanical stress and inflammatory factors.
- Mitral annular calcification can impair the AV node or bundle of His, causing arrhythmias.
- Rupture or dysfunction of chordae tendineae or papillary muscles (e.g., in MI) leads to acute regurgitation.
- Secondary to chamber dilation or wall stress (e.g., in heart failure) rather than primary valve disease.
- Originate at aortic sinuses: right and left coronary arteries exit just above corresponding aortic valve cusps.
- Named according to coronary artery relationship: right coronary, left coronary, posterior (non-coronary).
- Extensions of the ventricular myocardium, important for maintaining valve closure during systole.
- Indicated in patients with prosthetic valves or prior history of endocarditis undergoing high-risk procedures.
- Mutation in fibrillin-1 gene.
- Affects connective tissue of cardiovascular system (aorta, valves), eyes (lens dislocation), and skeleton.
- --
Beyond the Tutorial
- Caused by immune cross-reactivity (type II hypersensitivity) post-Group A strep pharyngitis.
- Jones criteria: Joints, Carditis, Nodules, Erythema marginatum, Sydenham chorea.
- Late sequela: mitral stenosis.
- S3: Associated with volume overload (e.g., in regurgitation, heart failure).
- S4: Associated with stiff ventricles (e.g., hypertrophy, ischemia).
- Aortic stenosis: crescendo-decrescendo systolic murmur, radiates to carotids.
- Mitral regurgitation: holosystolic murmur at apex, radiates to axilla.
- Aortic regurgitation: early diastolic murmur, wide pulse pressure.
- Mitral stenosis: diastolic rumble, opening snap.
- Key imaging modality to assess valve structure and function.
- Doppler used to estimate severity of stenosis/regurgitation.
- Standing/valsalva: decreases preload, accentuates MVP and HOCM murmurs.
- Squatting: increases preload/afterload, reduces MVP murmur.
- Mechanical: longer durability, but early thrombosis risk.
- Bioprosthetic: deteriorate over time, often within 10–15 years.
