USMLE/COMLEX 1 - Thyroid Gland Pathophysiology
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 1 & COMLEX-USA Level 1 from the Thyroid Pathophysiology tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
 Below is information not explicitly contained within the tutorial but important for USMLE & COMLEX 1.
Below is information not explicitly contained within the tutorial but important for USMLE & COMLEX 1.
- --
VITAL FOR USMLE/COMLEX 1
Thyroid Hormone Basics
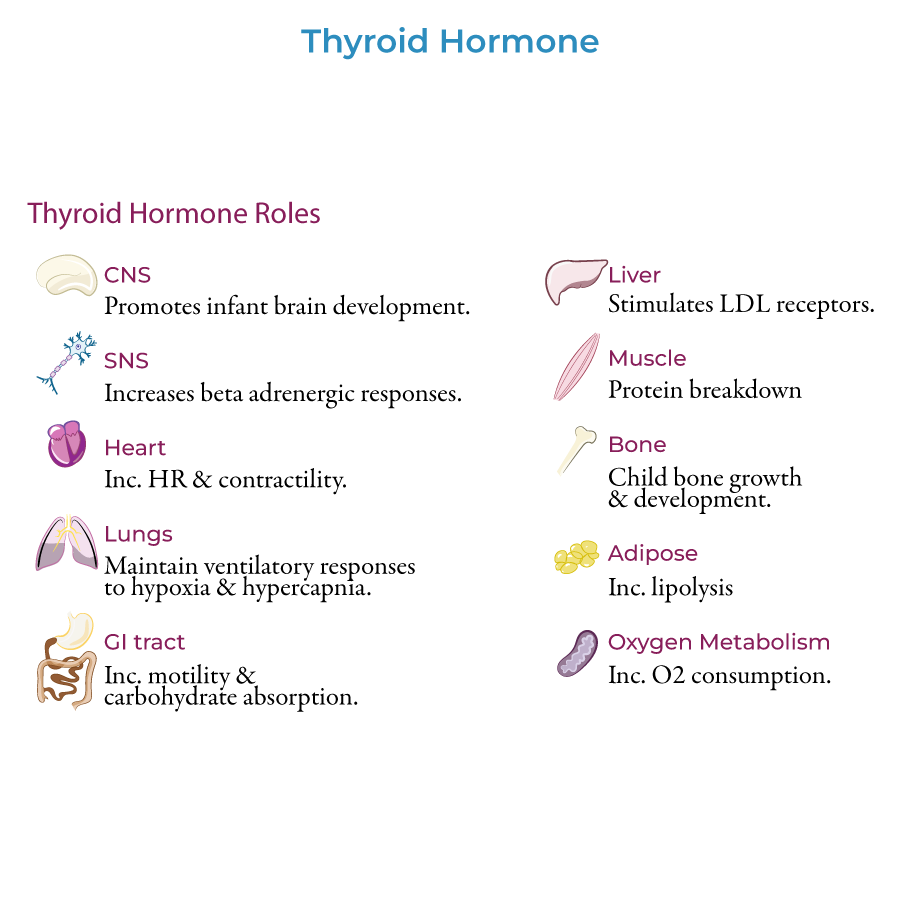
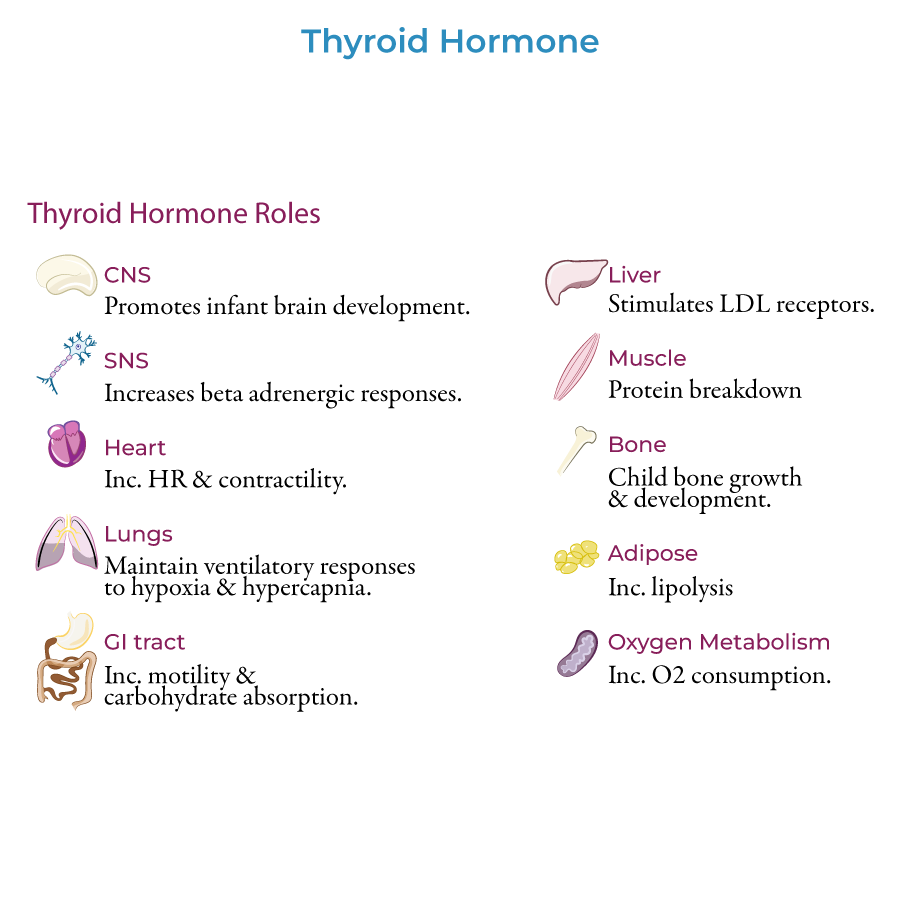
1. Thyroid hormones T3 and T4 are responsible for: CNS development in infants, bone growth and maturation in children, and proper functioning in multiple organ systems in adults.
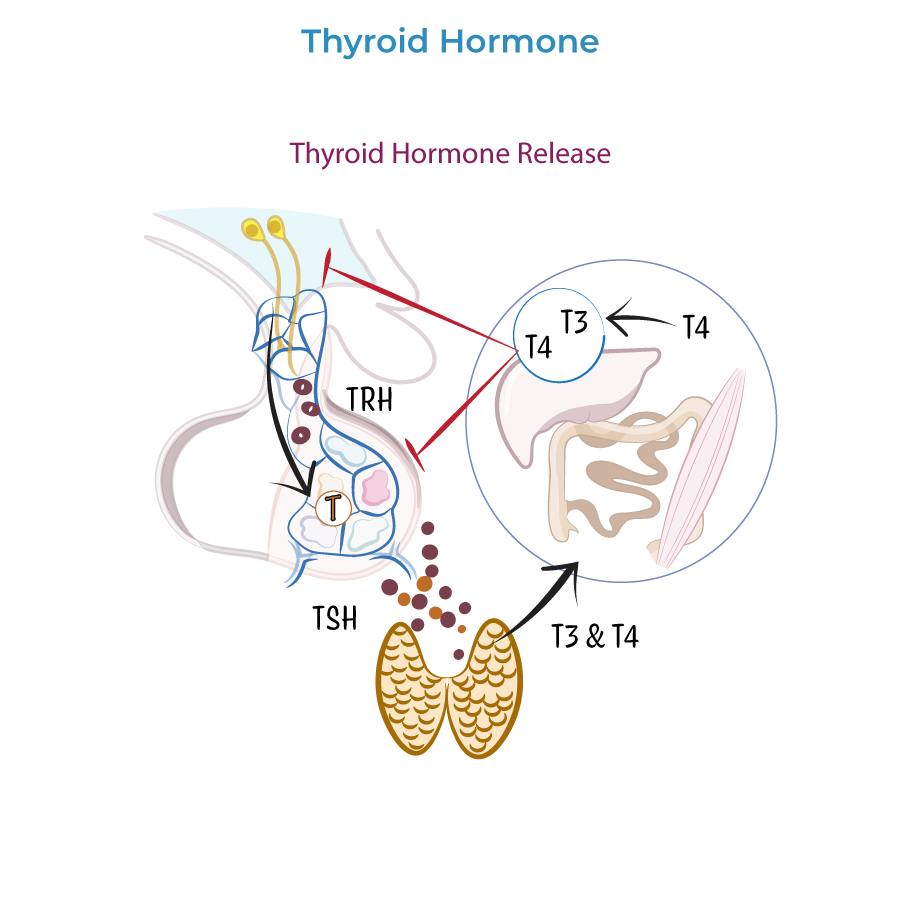
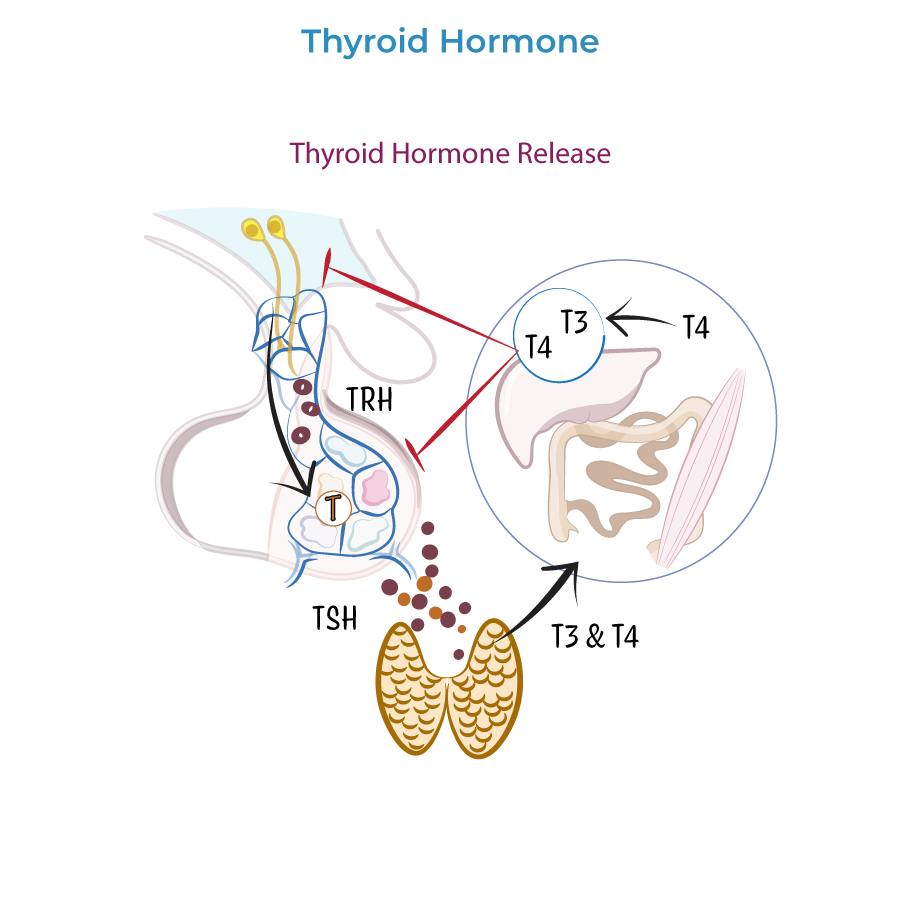
2. Hypothalamic-Pituitary-Thyroid axis: TRH from hypothalamus → TSH from anterior pituitary → T3 and T4 from thyroid.
3. Negative feedback: Thyroid hormones inhibit further secretion of TRH and TSH.
4. T3 is more biologically active than T4; peripheral tissues deiodinate T4 to T3.
5. Wolff-Chaikoff effect: Excessive iodine exposure inhibits iodine organification, avoiding thyroid hormone overproduction.
Hyperthyroidism (Thyrotoxicity)
1. Elevated T3 and T4 with low TSH (in primary hyperthyroidism).
2. Low LDL due to increased LDL receptors in the liver.
3. Most common cause in the US is Graves disease.
4. Characteristic findings: tachycardia, palpitations, systolic hypertension, weight loss despite increased appetite.
5. Ocular manifestations: exophthalmos (proptosis), lid retraction.
Hypothyroidism (Myxedema)
1. Low T3 and T4 with high TSH (in primary hypothyroidism).
2. Hypercholesterolemia due to reduced LDL receptor activity.
3. Most common cause in the US is Hashimoto thyroiditis.
4. Characteristic findings: bradycardia, reduced cardiac output, weight gain, cold intolerance.
5. Myxedema: nonpitting edema and puffy facies due to water retention.
Goiter
1. Definition: an enlarged thyroid gland.
2. Can be benign or a sign of underlying thyroid disease.
3. In some countries, lack of iodine is the primary cause, but rare in countries with iodine supplementation.
- --
HIGH YIELD
Thyroid Gland Functions
1. Cardiovascular effects: chronotropic and inotropic effects on heart (heart rate and contractility).
2. Metabolic effects: stimulate LDL receptors in liver, promote lipolysis in adipose tissue, and protein breakdown in muscle.
3. GI effects: promote GI motility and carbohydrate absorption.
4. Sympathetic nervous system: increases beta adrenergic receptor numbers and sensitivity.
5. Oxygen consumption: promotes oxygen consumption in many tissue types.
Hyperthyroidism Manifestations
1. Neuropsychiatric: hyperactivity, restlessness, anxiety, insomnia, increased reflexes, fine motor tremors.
2. Cardiovascular: tachycardia, palpitations, dyspnea, chest pain, systolic hypertension.
3. Musculoskeletal: proximal weakness with normal creatine kinase, accelerated bone growth and tissue turnover, risk for osteoporosis.
4. GI: increased bowel movements, possibly diarrhea, increased appetite.
5. Skin/Hair: warm moist skin, fine hair, vasodilation.
6. Reproductive: irregular or reduced menstrual flow, gynecomastia, lower libido, possibly reduced fertility.
7. Metabolic: heat intolerance, increased sweating, elevated basal metabolic rate, weight loss.
Hypothyroidism Manifestations
1. Neuropsychiatric: hypoactivity, fatigue, weakness, depressed mood, slow reflexes.
2. Cardiovascular: bradycardia, reduced cardiac output, dyspnea on exertion, risk for hypoventilation.
3. Musculoskeletal: proximal weakness with myalgia, elevated creatine kinase, impaired bone formation and growth in children.
4. GI: constipation, reduced appetite.
5. Skin/Hair: cool dry skin, coarse brittle hair, alopecia, brittle nails, nonpitting edema, puffy facies.
6. Reproductive: irregular menstruation, lower libido, reduced fertility.
7. Metabolic: cold intolerance, reduced sweating, lower basal metabolic rate, weight gain, possibly hyponatremia.
- --
Beyond the Tutorial
Thyroid Function Tests
1. TSH is the most sensitive test for thyroid disorders.
2. Free T4 levels are more reliable than total T4 due to binding protein variations.
3. TRH stimulation test can help diagnose secondary hypothyroidism.
Specific Thyroid Disorders
1. Graves' disease: antibodies against TSH receptor (stimulating); association with HLA-DR3.
2. Hashimoto's thyroiditis: autoimmune disorder with anti-thyroid peroxidase (anti-TPO) antibodies.
3. Subacute thyroiditis: viral etiology, painful thyroid with transient hyperthyroidism followed by hypothyroidism.
4. Silent thyroiditis: postpartum thyroiditis is the most common form.
Treatment Considerations
1. Hyperthyroidism: beta-blockers for symptomatic relief, thionamides (PTU, methimazole), radioactive iodine ablation, surgery.
2. Hypothyroidism: levothyroxine (T4) replacement, with careful dosing in elderly and heart disease patients.
3. Thyroid storm: emergency condition requiring aggressive treatment with beta-blockers, thionamides, iodine solutions, and corticosteroids.
4. Myxedema coma: life-threatening complication of severe hypothyroidism requiring immediate T4 and possibly T3 therapy.
