USMLE/COMLEX 1 - Supraventricular & Ventricular Arrhythmias
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 1 & COMLEX-USA Level 1 from the Arrhythmias tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
- --
VITAL FOR USMLE/COMLEX 1
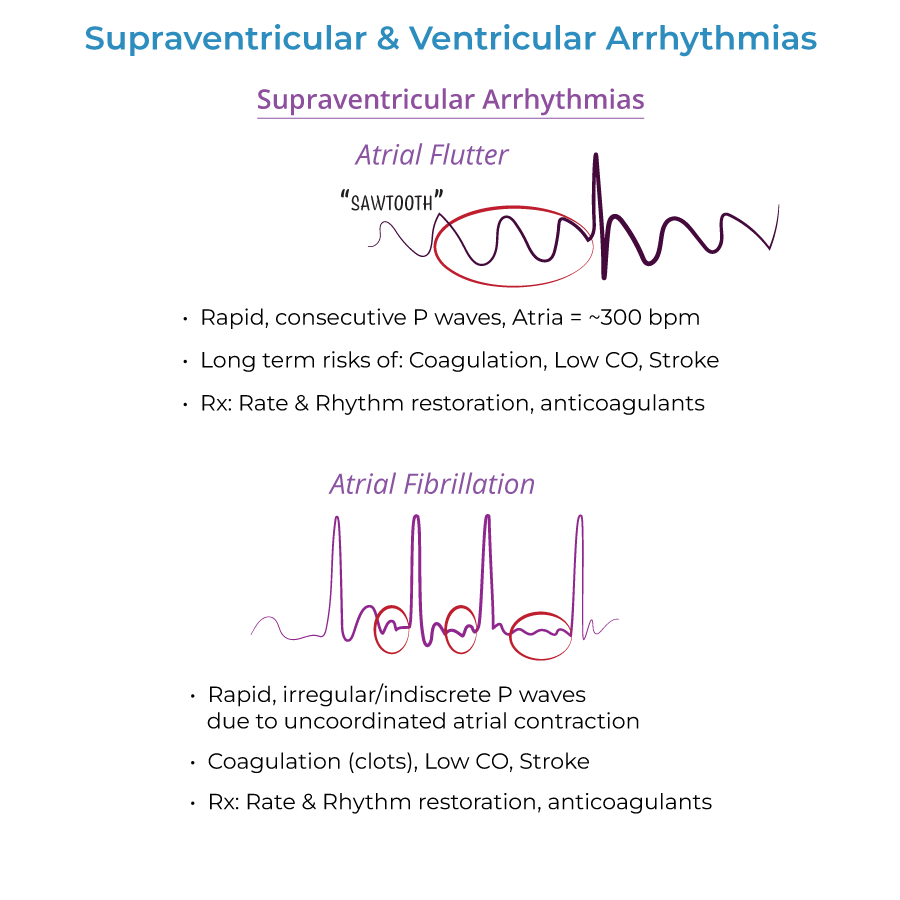
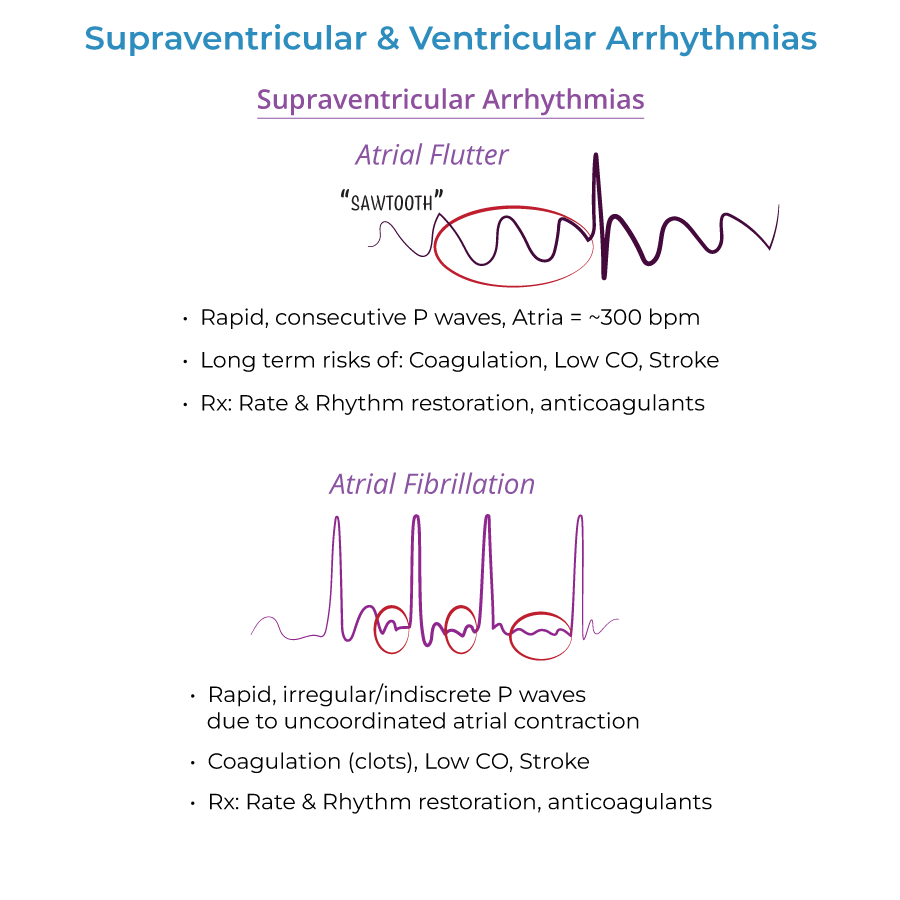
Atrial Flutter
1. ECG findings: Rapid, regular P waves give ECG "sawtooth" appearance.
2. Atrial rate: Atria beat ~300 beats/minute. Only ½ - 1/3 of the electrical impulses make it through the AV node.
3. Treatment options: Rate control with drugs: beta-blockers, calcium channel blockers (verapamil, diltiazem). Rhythm control with cardioversion, drugs (antiarrhythmics), possibly ablation.
Atrial Fibrillation
1. ECG characteristics: Rapid, irregular and indiscrete P waves on ECG.
2. Cardiac dysfunction: Atria do not contract in coordinated fashion, but send fast and irregular signals to ventricles.
3. Treatment approach: Rate control with beta blockers and nondihydropyridine calcium channel blockers. Anticoagulation before cardioversion therapy to prevent thromboembolism.
4. Clinical concerns: Stroke, systemic emboli. Must rule out Wolff-Parkinson-White Syndrome before prescribing AV-node blocking drugs.
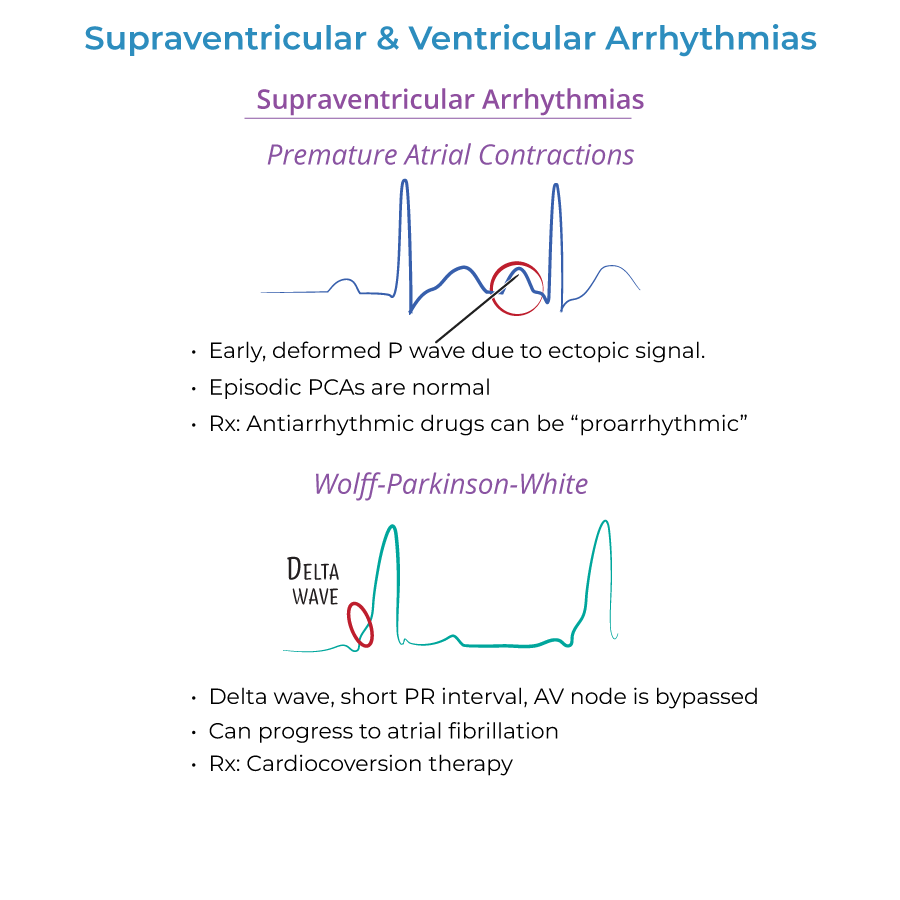
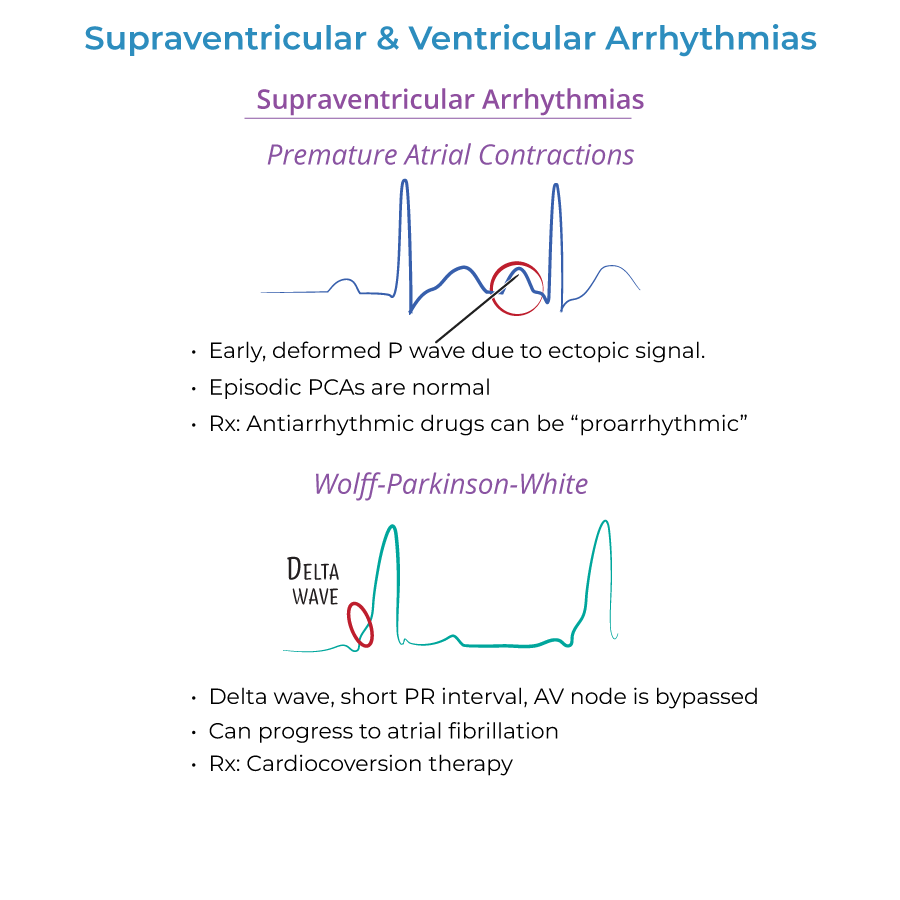
Wolff-Parkinson-White Syndrome
1. ECG findings: Short PR interval and positive delta wave at beginning of broad QRS complex.
2. Pathophysiology: Occurs as result of AV node bypass, called bundle of Kent.
3. Treatment warning: Beware digoxin/nondihydropyridine calcium channel blockers in WPW patients, as they may trigger ventricular fibrillation (fatal).
Ventricular Tachycardia
1. Definition: 3+ consecutive beats 120+ beats/minute; abnormal ventricular automacy.
2. Torsades de Pointes: Special case of ventricular tachycardia, associated with Long QT Syndrome.
3. ECG in Torsades: Rapid, irregular QRS complexes "spiral" around baseline, as ventricular rate varies from cycle to cycle.
- --
HIGH YIELD
Atrial Arrhythmias
1. Atrial Flutter symptoms: May cause palpitations, reduced CO, difficulty breathing, weakness, chest discomfort, syncope.
2. Atrial Fibrillation symptoms: May experience lack of energy, fast irregular pulse, difficulty breathing, palpitations, chest discomfort, dizziness.
3. Risk factors for Atrial Flutter/Fibrillation: Commonly occurs with other cardiac conditions, binge alcohol consumption, diabetes, hyperthyroidism, obesity, lung disease.
4. Premature beats: Early atrial or ventricular contractions visible on ECG. Caused by ectopic pacemaker activity.
Ventricular Arrhythmias
1. Symptoms of Ventricular Tachycardia: If sustained, causes palpitations, difficulty breathing, chest pain, dizziness, fainting, death.
2. Treatment of Ventricular Tachycardia: Cardioversion, antiarrhythmic drugs, defibrillator implant.
3. Torsades de Pointes treatment: Magnesium.
4. Torsades triggers: Electrolyte imbalances (hypocalcemia, hypokalemia); Medications (antiarrhythmics, tricyclic antidepressants, anti-histamines when taken with erythromycin).
Long QT Syndrome
1. Description: Long QT interval on ECG, reflects defective ion channels.
2. Risk factors: Often inherited, but can be acquired (electrolyte imbalances, medications).
3. Inherited forms: Romano-Ward Syndrome (Types 1-3) and Jervell and Lange-Nielsen Syndrome (associated with congenital deafness).
Cardiac Arrest Rhythms
1. Asystole: Often described as "Flat-lining" on ECG. Cessation of electrical and mechanical cardiac activity.
2. Pulseless Electrical Activity: Cardiac electrical activity is present, but no pulse due to inactivity of cardiac muscle.
3. Ventricular Fibrillation: Uncoordinated ventricular activity leading to loss of consciousness and death without immediate intervention.
4. Ventricular Fibrillation treatment: CPR & Defibrillation.
- --
Beyond the Tutorial
Differential Diagnosis
1. Distinguishing Atrial Flutter from Fibrillation: Atrial flutter has regular, organized sawtooth P waves while fibrillation has irregular, chaotic P waves.
2. Tachycardia differential: Important to distinguish supraventricular tachycardias from ventricular tachycardias, as treatment approaches differ significantly.
Pharmacology Considerations
1. Rate vs. Rhythm control: Understanding when to prioritize controlling rate versus attempting to restore normal sinus rhythm.
2. Anticoagulation timing: When to initiate anticoagulation relative to cardioversion to prevent thromboembolic events.
3. QT-prolonging medications: Many drug classes can prolong QT interval, including antipsychotics, antibiotics, and antiarrhythmics.
Pathophysiology
1. Triggered activity: Delayed afterdepolarizations and early afterdepolarizations as mechanisms for arrhythmogenesis.
2. Reentry circuits: Understanding anatomical and functional reentry as mechanisms for sustaining arrhythmias.
3. Autonomic influences: Role of sympathetic and parasympathetic tone in facilitating or preventing arrhythmias.
Diagnostic Testing
1. Beyond ECG: Role of Holter monitoring, event recorders, electrophysiology studies, and stress testing in arrhythmia evaluation.
2. Genetic testing: Indications for genetic testing in suspected inherited arrhythmia syndromes.
