USMLE/COMLEX 1 - Small Vessel Vasculitis
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 1 & COMLEX-USA Level 1 from the Small Vessel Vasculitis tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
 5. Eosinophilic granulomatosis with polyangiitis (EGPA) (formerly Churg-Strauss):
5. Eosinophilic granulomatosis with polyangiitis (EGPA) (formerly Churg-Strauss):
 6. Microscopic polyangiitis (MPA):
6. Microscopic polyangiitis (MPA):
- --
VITAL FOR USMLE/COMLEX 1
General Concepts of Small Vessel Vasculitis
1. Small vessel vasculitides involve arterioles, venules, capillaries, leading to inflammation, ischemia, and organ damage.
2. General systemic symptoms: fever, arthralgia, fatigue, weight loss, with cutaneous manifestations like palpable purpura.
3. Treatment for most vasculitides involves high-dose corticosteroids and often immunosuppressants.
ANCA-Associated Vasculitides
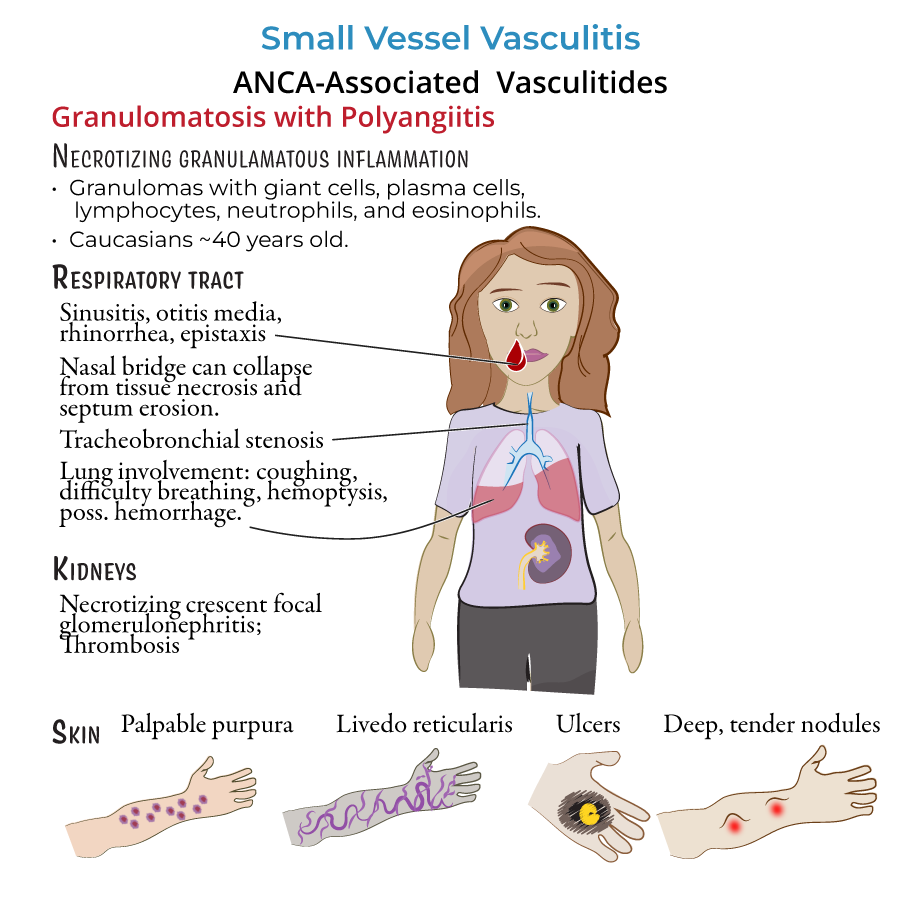
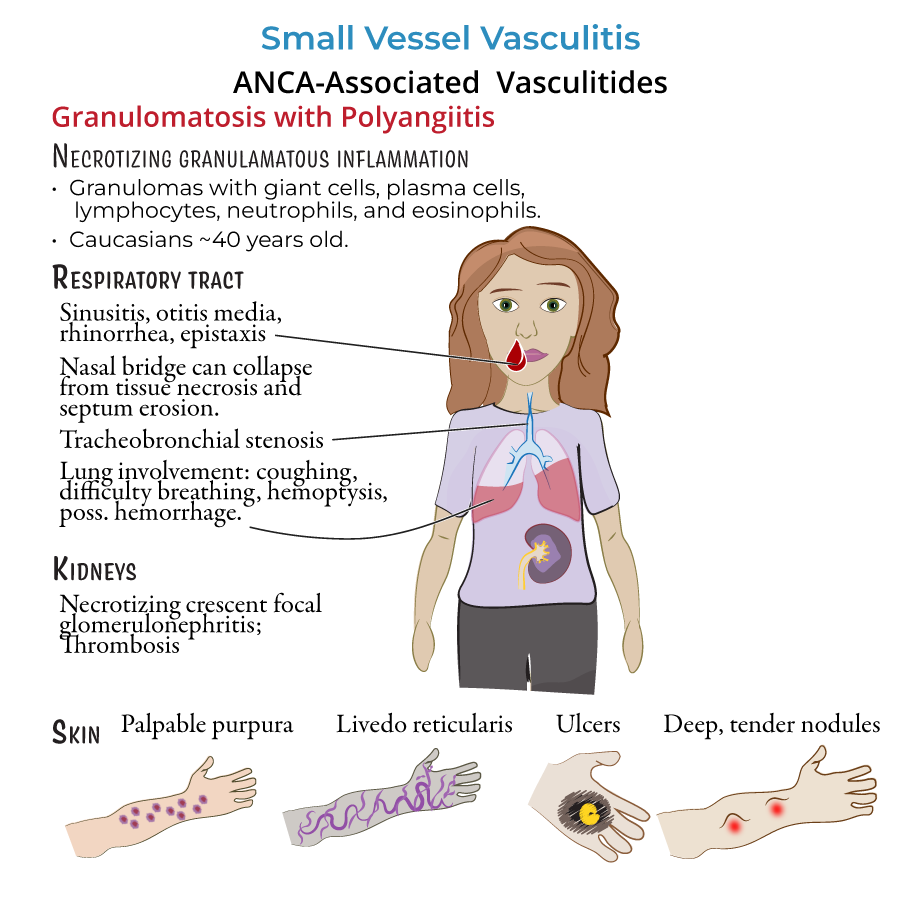
4. Granulomatosis with polyangiitis (GPA) (formerly Wegener's):
- Necrotizing granulomatous inflammation.
- Affects respiratory tract (sinusitis, otitis media, hemoptysis) and kidneys (necrotizing glomerulonephritis).
- Destruction of nasal septum can lead to saddle-nose deformity.
- Skin manifestations include palpable purpura, nodules, ulcers.
- Primarily affects Caucasians, average onset around 40 years.
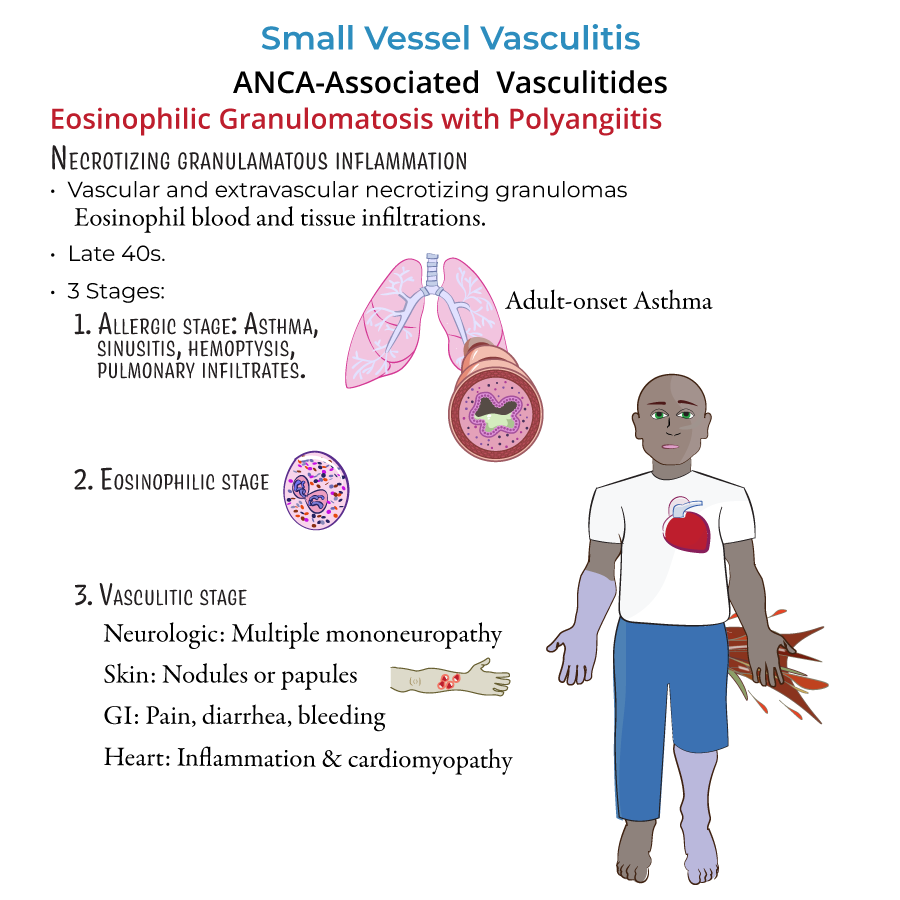
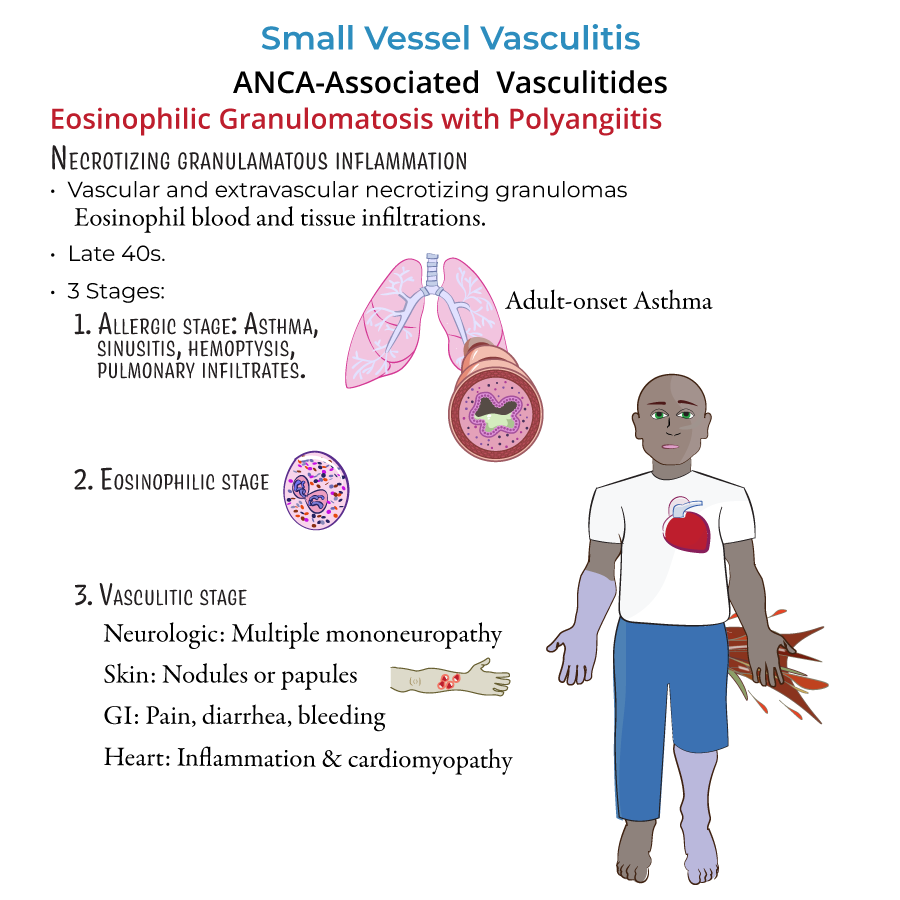
 5. Eosinophilic granulomatosis with polyangiitis (EGPA) (formerly Churg-Strauss):
5. Eosinophilic granulomatosis with polyangiitis (EGPA) (formerly Churg-Strauss):
- Necrotizing granulomas with eosinophils.
- Clinical stages:
- Allergic stage: adult-onset asthma, sinusitis.
- Eosinophilic stage: blood/tissue eosinophilia.
- Vasculitic stage: mononeuritis multiplex, skin papules, GI bleeding, cardiomyopathy.
- Cardiac involvement is a major cause of morbidity and mortality.
- Kidney involvement is less common than in GPA.
 6. Microscopic polyangiitis (MPA):
6. Microscopic polyangiitis (MPA):
- Necrotizing vasculitis without granulomas.
- Commonly presents with glomerulonephritis and palpable purpura.
- Lung involvement possible but less frequent; when present, alveolar hemorrhage and fibrosis are serious.
- Typically develops in patients aged 50–60 years.
Non-ANCA-Associated Small Vessel Vasculitides
7. Immunoglobulin A-associated vasculitis (IgA vasculitis / Henoch-Schönlein purpura):
- IgA immune complex deposition.
- Presents with palpable purpura, arthralgias, abdominal pain, and renal involvement (IgA nephropathy).
- Common in children (self-limited), but chronic in adults.
- Caused by cryoglobulins precipitating at cold temperatures.
- Symptoms: fatigue, palpable purpura, arthralgias, glomerulonephritis, peripheral neuropathy.
- Type I: associated with B-cell lymphoproliferative disorders.
- Types II and III: associated with Hepatitis C infection.
- --
HIGH YIELD
Granulomatosis with Polyangiitis (GPA) and EGPA
1. GPA can cause tracheal stenosis and airway obstruction.
2. GPA and MPA are associated with ANCA positivity:
- GPA typically has c-ANCA (PR3-ANCA).
- MPA typically has p-ANCA (MPO-ANCA).
Cryoglobulinemia and Hepatitis C
5. Mixed cryoglobulinemia can cause glomerulonephritis and neurologic symptoms.
6. Diagnosis often includes low complement levels, especially low C4.
IgA Vasculitis (Henoch-Schönlein Purpura)
7. GI symptoms often include colicky abdominal pain and melena or hematochezia (blood in stool).
8. Kidney biopsy shows mesangial IgA deposits.
Additional Organ Involvement
9. Cutaneous signs across vasculitides often include palpable purpura (non-blanching).
10. Cardiomyopathy is a major cause of death in EGPA due to eosinophilic infiltration.
- --
Beyond the Tutorial
GPA, EGPA, MPA Laboratory Associations
1. GPA: Positive for c-ANCA (anti-proteinase 3).
2. MPA: Positive for p-ANCA (anti-myeloperoxidase).
3. EGPA: Often p-ANCA positive, elevated eosinophils in blood.
Classic Associations and Patterns
4. In GPA, chest imaging may show nodular infiltrates, cavitary lung lesions, or alveolar hemorrhage.
5. Cryoglobulinemia should be suspected in patients with hepatitis C and a triad of purpura, arthralgias, and glomerulonephritis.
6. In IgA vasculitis, symptoms usually follow an upper respiratory infection.
Treatment Overview
7. Most small vessel vasculitides are treated initially with high-dose corticosteroids.
8. Severe organ involvement may require cyclophosphamide or rituximab.
9. In cryoglobulinemia associated with hepatitis C, antiviral therapy is essential along with immunosuppression in severe cases.
