USMLE/COMLEX 1 - Pulmonary Embolism and Deep Vein Thrombosis
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 1 & COMLEX-USA Level 1 from the Pulmonary Embolism & Deep Vein Thrombosis tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
 Below is information not explicitly contained within the tutorial but important for USMLE & COMLEX 1.
Below is information not explicitly contained within the tutorial but important for USMLE & COMLEX 1.
- --
VITAL FOR USMLE/COMLEX 1
Pathophysiology of Venous Thromboembolism
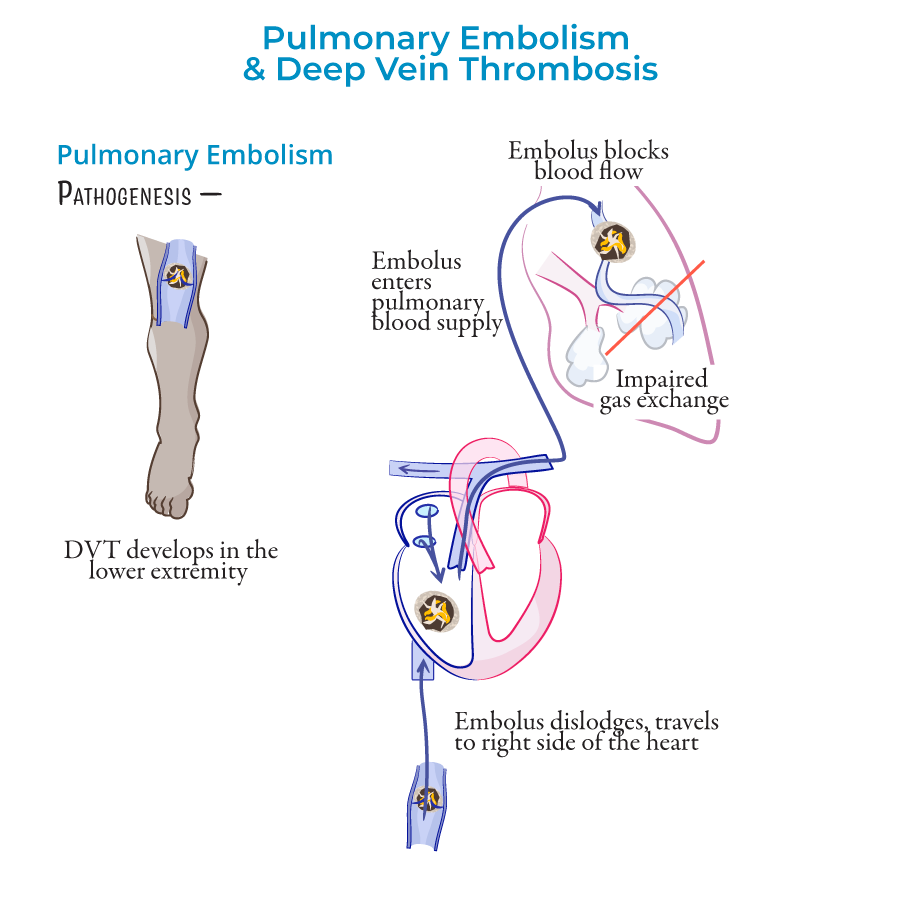
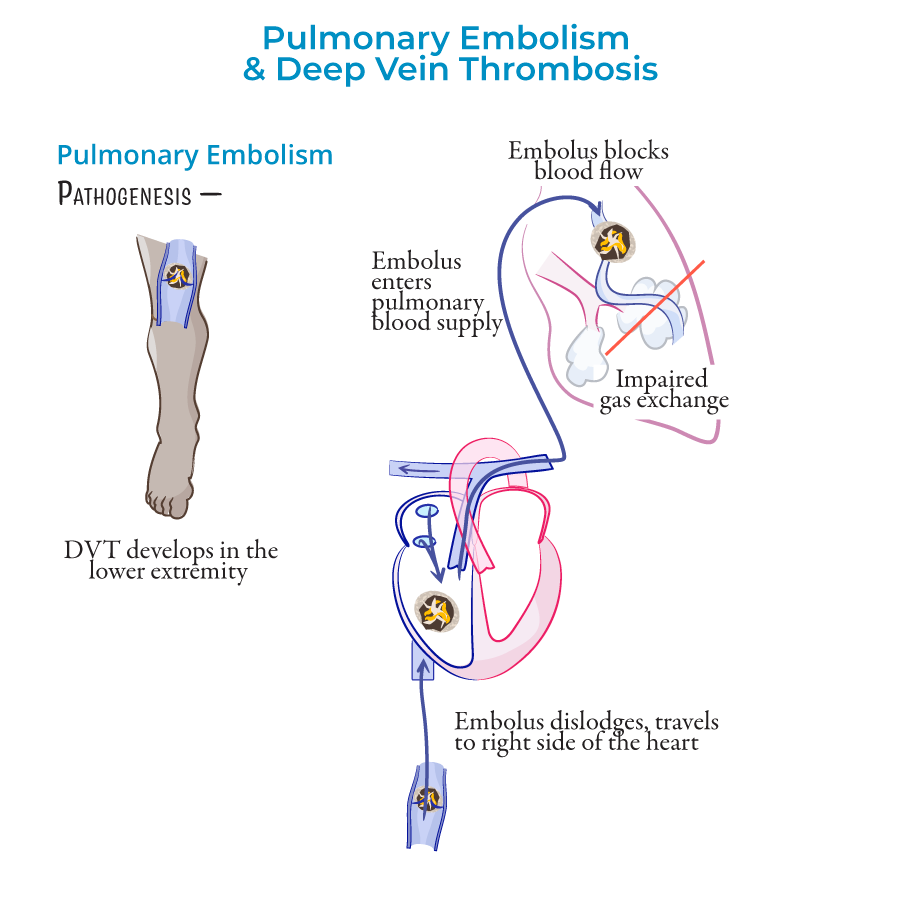
1. Definition: Pulmonary embolism (PE) occurs when pulmonary arteries are obstructed, most commonly by emboli from deep veins of thighs/pelvis.
2. Venous thromboembolism (VTE): Combined term for deep vein thrombosis (DVT) and pulmonary embolism.
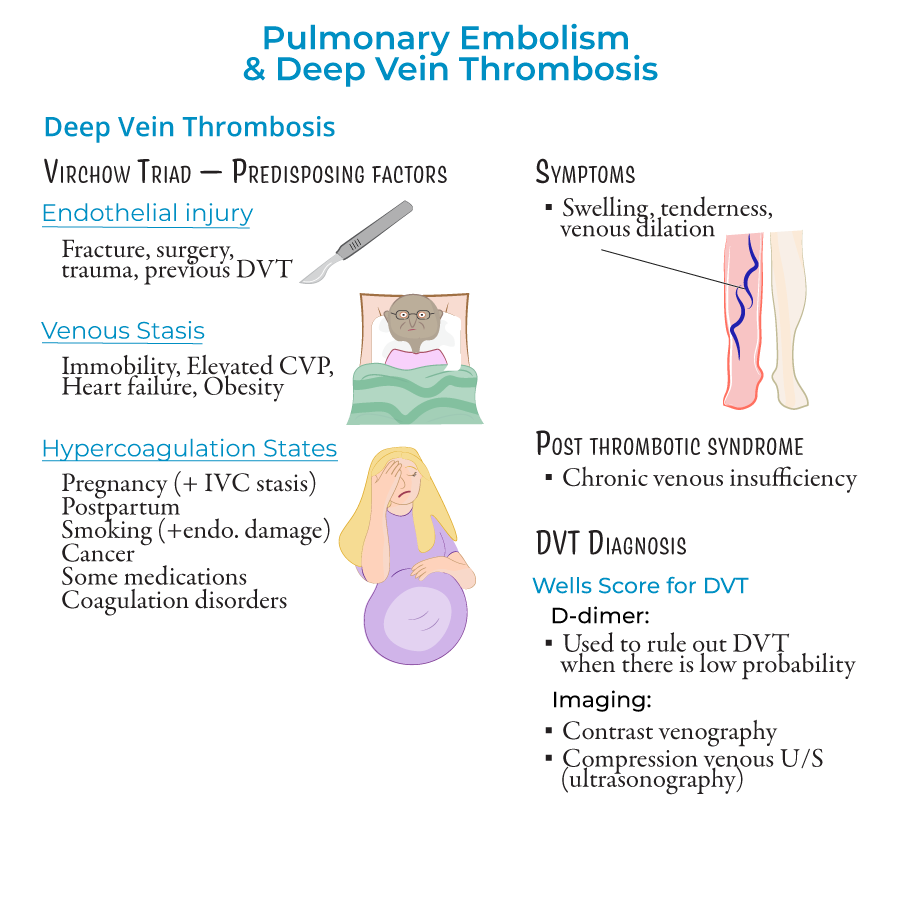
3. Virchow's Triad: Three factors predisposing to thrombosis:
- Endothelial injury: Due to fracture, surgery, trauma, or previous DVT; triggers clotting cascade
- Venous stasis: Caused by immobility, elevated central venous pressure, heart failure, obesity
- Hypercoagulable states: Pregnancy, postpartum period, smoking, cancer, hormonal contraceptives/therapies, coagulation disorders (Factor V Leiden)
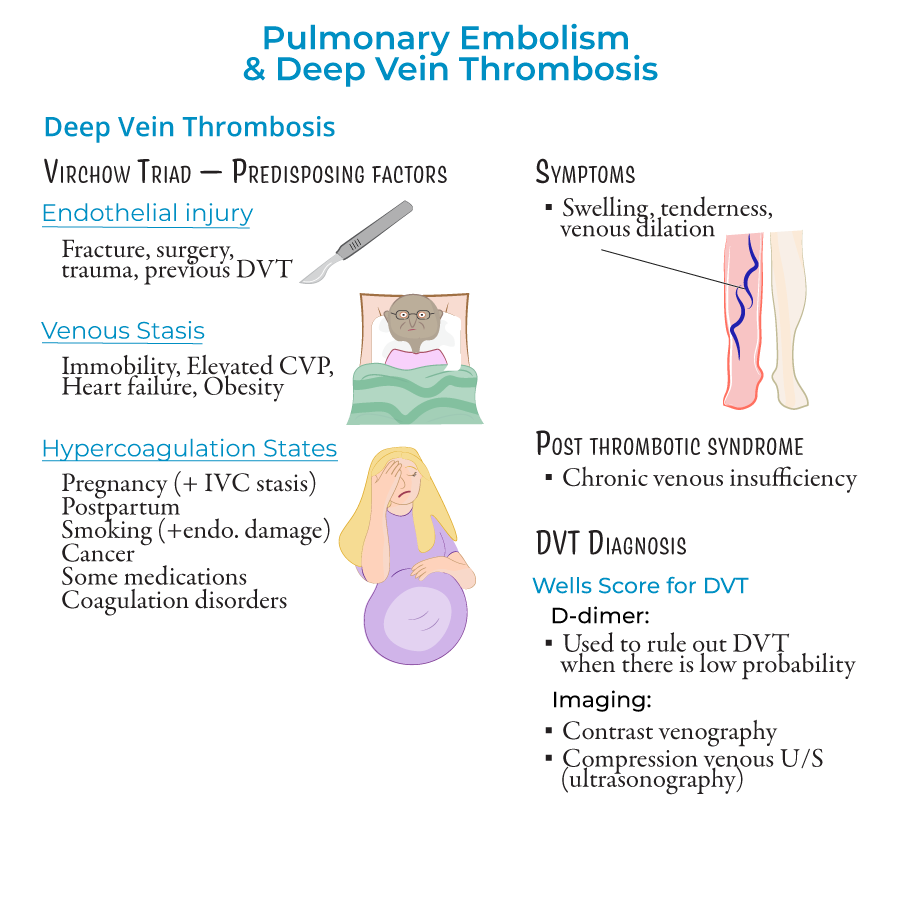
Deep Vein Thrombosis (DVT)
1. Definition: Formation of blood clot in deep veins, most commonly in lower extremities.
2. Primary cause: Leading cause of pulmonary embolism.
3. Clinical features: When symptomatic, presents with unilateral leg swelling, tenderness, and venous dilation.
4. Complications:
- Post-thrombotic syndrome due to venous valve damage
- Pulmonary embolism (most serious complication)
Pulmonary Embolism (PE)
1. Definition: Obstruction of pulmonary arteries, usually by thrombi from deep veins.
2. Nonthrombotic sources: Air, fat, amniotic fluid, bacterial (septic), foreign bodies, and tumors.
3. Classification:
- By risk: Massive (high risk), intermediate (submassive), and low risk
- By location: Saddle emboli (at pulmonary trunk bifurcation), lobar, segmental, or subsegmental
- Ventilation-perfusion mismatch
- Hypoxemia
- Respiratory alkalosis
- Pulmonary hypertension
- Right heart failure
Diagnostic Approach
1. DVT diagnosis:
- Wells Score for DVT (considering swelling, edema, alternative diagnoses)
- D-dimer testing (to rule out low-probability DVT)
- Imaging: Contrast venography or venous ultrasonography with compression
- Wells Score for PE (heart rate, signs/symptoms, alternative diagnoses)
- D-dimer: >500 ng/mL suggests possible PE
- Imaging: CT angiography, ventilation-perfusion scan
- ECG: May show sinus tachycardia, S1Q3T3 pattern (S in lead I, Q and inverted T in lead III)
- Chest X-ray: May show atelectasis, Hampton hump (pulmonary infarction), Westermark sign (oligemic areas), pleural effusion
Treatment Principles
1. Supportive therapy: Oxygen, saline, vasopressors.
2. Anticoagulation:
- Acute: Heparin, enoxaparin, or fondaparinux
- Long-term: Warfarin
- Sequential compression devices (SCDs) to prevent venous stasis
- Prophylactic anticoagulants (low-dose enoxaparin or heparin)
- --
HIGH YIELD
Virchow's Triad Details
1. Endothelial injury:
- Trauma stimulates clotting cascade
- Surgery, especially orthopedic
- Previous DVT damages vessel walls
- Inflammation causes endothelial dysfunction
- Immobility (long flights, bedridden patients)
- Heart failure reduces forward flow
- Compression of veins (e.g., May-Thurner syndrome, pregnancy)
- Obesity increases intra-abdominal pressure
- Pregnancy (also causes IVC compression)
- Malignancy (especially pancreatic, lung)
- Hormonal contraceptives increase clotting factors
- Genetic disorders (Factor V Leiden, Protein C/S deficiency)
Clinical Features & Presentations
1. DVT symptoms: Often unilateral leg swelling, tenderness, venous dilation.
2. PE symptoms: Dyspnea (85%), chest pain (40-75%), tachypnea, tachycardia.
3. Silent presentation: Both DVT and PE can be asymptomatic.
4. Massive PE: Presents with hemodynamic instability (hypotension).
5. Altered mental status: Important clue in elderly patients.
Diagnostic Testing Details
1. D-dimer:
- Fibrin degradation product
- High sensitivity, low specificity
- Negative predictive value in low-probability patients
- <2: Low probability
- 2-6: Moderate probability
- >6: High probability
- Hampton hump: Wedge-shaped pulmonary infarction, usually in lower lobes
- Westermark sign: Focal oligemia (hypoperfusion)
- Saddle embolus: Visible at bifurcation of main pulmonary artery
Pulmonary Infarction
1. Mechanism: Small emboli obstruct blood flow causing tissue ischemia.
2. Location: Most common in lower lobes.
3. Radiographic finding: Wedge-shaped "Hampton Hump" on chest X-ray.
4. Clinical significance: Indicates tissue death from prolonged ischemia.
5. Pathology: Hemorrhagic necrosis of lung parenchyma.
Treatment Considerations
1. Anticoagulation contraindications: Active bleeding, recent surgery, thrombocytopenia.
2. Thrombolysis indications: Massive PE with hemodynamic instability.
3. Inferior vena cava filters: When anticoagulation is contraindicated.
4. Prophylaxis importance: High-risk patients should receive appropriate prophylaxis.
5. Post-thrombotic syndrome: Long-term complication of DVT requiring management.
- --
Beyond the Tutorial
Hemostasis & Coagulation Cascade
1. Intrinsic pathway: Activated by contact with collagen via Factor XII.
2. Extrinsic pathway: Activated by tissue factor (Factor III) exposure.
3. Common pathway: Both pathways converge at Factor X activation.
4. Fibrinolytic system: Plasmin degrades fibrin to produce D-dimers.
5. Natural anticoagulants: Protein C, Protein S, Antithrombin III inhibit clotting.
Detailed Pathophysiology
1. Right ventricular failure: Acute pressure overload causes RV dilation and dysfunction.
2. Pulmonary hypertension: Acute from mechanical obstruction; chronic from repeated emboli.
3. Dead space ventilation: Areas ventilated but not perfused, wasting respiratory effort.
4. Hypoxemic mechanisms: V/Q mismatch, shunting, impaired diffusion.
5. Platelet activation: Contributes to propagation of thrombus.
Additional Risk Factors
1. Inherited thrombophilias: Antithrombin deficiency, protein C/S deficiency, prothrombin gene mutation.
2. Antiphospholipid syndrome: Autoimmune disorder causing hypercoagulability.
3. Heparin-induced thrombocytopenia: Paradoxical thrombosis due to antibodies against heparin-PF4 complex.
4. Malignancy-associated: Especially mucin-producing adenocarcinomas (Trousseau syndrome).
5. Inflammatory bowel disease: Increases thrombotic risk through multiple mechanisms.
Pathologic Features
1. Gross appearance: Red-blue obstructive material in pulmonary arteries.
2. Lines of Zahn: Alternating layers of platelets/fibrin and red cells in organized thrombi.
3. Pulmonary infarcts: Typically wedge-shaped, hemorrhagic, and subpleural.
4. Resolution process: Thrombolysis and recanalization over days to weeks.
5. Chronic changes: Organization and fibrosis of unresolved thrombi.
Advanced Diagnostic Considerations
1. CT pulmonary angiography: Gold standard showing filling defects in pulmonary arteries.
2. Echocardiography: May show right ventricular strain, McConnell's sign (RV free wall akinesis with apical sparing).
3. Elevated troponin: Indicates myocardial injury from RV strain.
4. BNP/NT-proBNP: Elevated in right heart failure.
5. Normal A-a gradient: Rare in PE, making a low A-a gradient useful in excluding PE from differential.
