USMLE/COMLEX 1 - Myocardial Infarctions
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 1 & COMLEX-USA Level 1 from the Myocardial Infarctions: Diagnosis & Treatment tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
 Below is information not explicitly contained within the tutorial but important for USMLE & COMLEX 1.
Below is information not explicitly contained within the tutorial but important for USMLE & COMLEX 1.
- --
VITAL FOR USMLE/COMLEX 1
Definition and Pathophysiology
1. Myocardial infarction is defined as myocardial injury with ischemia.
2. MI results from coronary artery occlusion leading to ischemia and necrosis.
3. STEMI (ST-elevation MI) indicates complete occlusion with transmural infarction.
4. NSTEMI (Non-ST-elevation MI) typically reflects partial occlusion or subendocardial infarction.
5. Cardiac troponin elevation is the gold standard biomarker for diagnosis.
Epidemiology & Risk Factors
1. Declining in high-income countries but rising in middle/low-income countries.
2. Incidence after age 35, from highest to lowest: Black males > Black females > White males > White females.
3. MI occurs approximately 10 years earlier in men than women.
4. Key modifiable risk factors: Dyslipidemia, diabetes mellitus, hypertension, smoking, obesity.
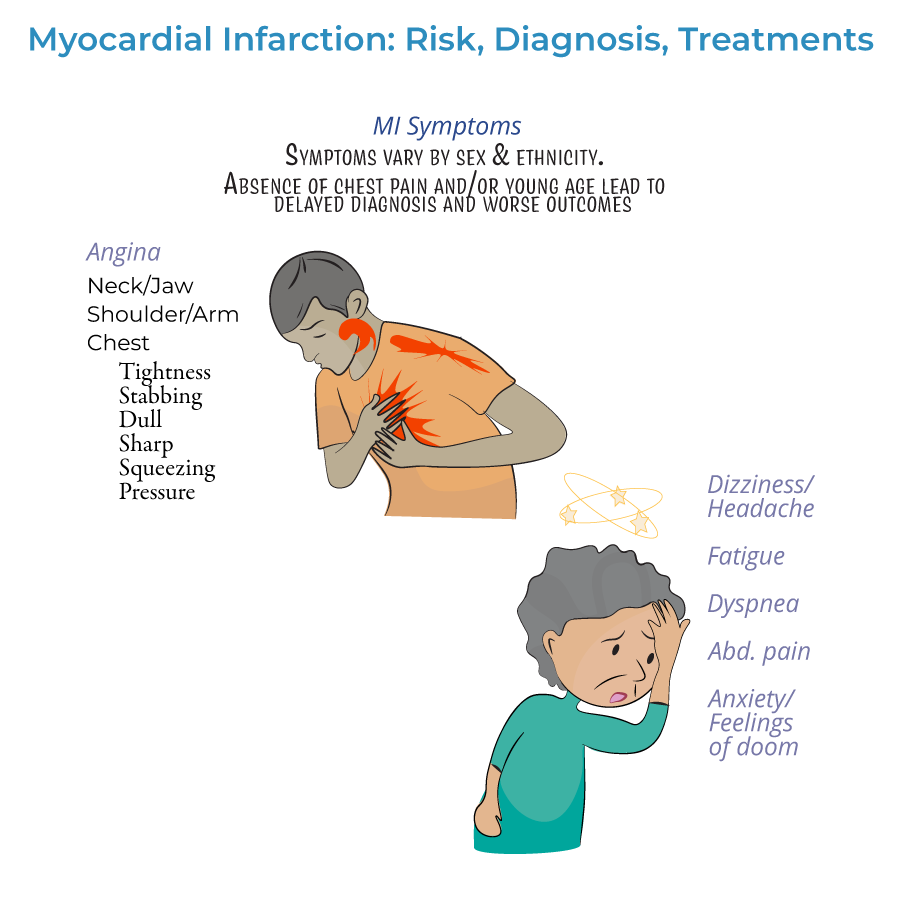
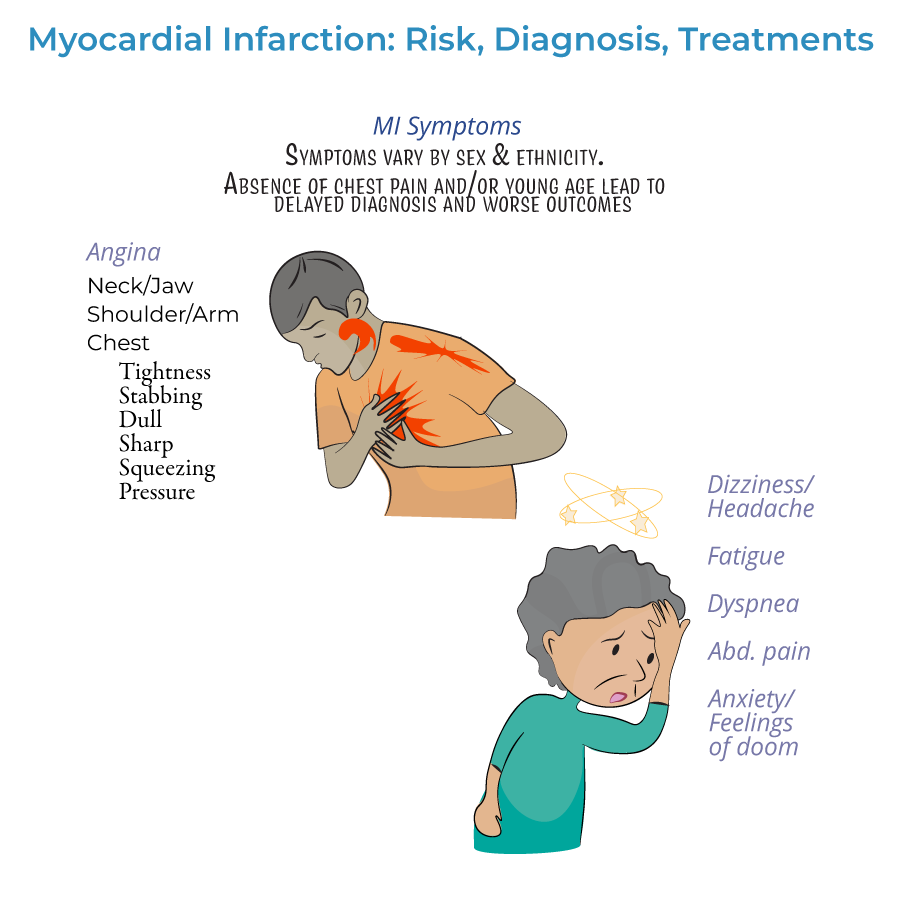
Clinical Presentation
1. Classic symptoms: Chest pain/pressure radiating to left arm, neck, or jaw.
2. Atypical presentations common in women, elderly, and diabetics: fatigue, dyspnea, epigastric pain.
3. Silent MI may occur without noticeable symptoms, especially in diabetics.
4. Associated symptoms: nausea, vomiting, diaphoresis, anxiety, sense of impending doom.
Diagnosis
1. ECG is the first diagnostic tool - distinguishes STEMI vs. NSTEMI.
2. Cardiac biomarkers: Troponin I/T and CK-MB show characteristic rise and fall.
3. Troponin peaks within 24 hours and is more specific than CK-MB.
4. ECG localization correlates with specific coronary artery territories:
- Anterior: Left anterior descending artery (leads V3-V4)
- Inferior: Right coronary artery (leads II, III, aVF)
- Lateral: Left circumflex artery (leads I, aVL, V5-V6)
Treatment Principles
1. Time is myocardium - prompt reperfusion is essential.
2. STEMI treatment: Primary PCI within 90 minutes or fibrinolytics within 30 minutes.
3. Immediate medications: Aspirin, P2Y12 inhibitor, anticoagulation, oxygen (if saturation <90%).
4. Secondary prevention: Beta-blockers, ACE inhibitors/ARBs, statins, lifestyle modification.
- --
HIGH YIELD
ECG Localization and Vessel Correlation
1. Anterior MI (V3-V4): Left anterior descending artery.
2. Anteroseptal MI (V1-V2): Proximal left anterior descending artery.
3. Lateral MI (I, aVL): Left circumflex artery.
4. Inferior MI (II, III, aVF): Right coronary artery (90%), left circumflex (10%).
5. Posterior MI (V7-V9, tall R in V1-V2): Right coronary or left circumflex artery.
6. Right ventricular MI (ST elevation in V4R): Proximal right coronary artery.
Cardiac Biomarkers
1. Troponin I and T: Rise within 3-6 hours, peak at 24 hours, remain elevated for 7-10 days.
2. CK-MB: Rises within 4-6 hours, peaks at 24 hours, normalizes within 48-72 hours.
3. Myoglobin: Earliest marker (1-3 hours) but lacks specificity.
4. Biomarker timing is critical for diagnosis of reinfarction or extension.
Complications of MI
1. Early (hours to days): Arrhythmias, cardiogenic shock, free wall rupture, ventricular septal rupture, papillary muscle rupture.
2. Late (days to weeks): Pericarditis, ventricular aneurysm, mural thrombus, heart failure.
3. Right ventricular infarction presents with elevated JVP, hypotension, and clear lung fields.
4. Dressler syndrome (autoimmune pericarditis) can occur weeks to months after MI.
Acute Treatments
1. Door-to-balloon time <90 minutes for primary PCI in STEMI.
2. Fibrinolytic contraindications: Recent surgery/trauma, prior intracranial hemorrhage, uncontrolled hypertension.
3. Nitrates are contraindicated in right ventricular infarction and with phosphodiesterase inhibitor use.
4. Morphine can be used for pain but may mask symptoms and should be used cautiously.
Cross-Type Concepts
1. Stunned myocardium: Temporarily dysfunctional but viable tissue after reperfusion.
2. Hibernating myocardium: Chronically dysfunctional but viable tissue due to chronic hypoperfusion.
3. ECG progression: Hyperacute T waves → ST elevation → Q waves → T wave inversion → normalization.
4. Reciprocal changes (ST depression) in leads opposite to the infarct site have prognostic significance.
- --
Beyond the Tutorial
Myocardial Infarction Types
1. Type 1: Spontaneous MI related to atherosclerotic plaque rupture.
2. Type 2: Supply-demand mismatch (e.g., severe anemia, hypotension).
3. Type 3: Sudden cardiac death with suspected MI but no biomarker confirmation.
4. Type 4: MI related to PCI or stent thrombosis.
5. Type 5: MI related to CABG.
Arrhythmias Associated with MI Locations
1. Anterior MI: Bundle branch blocks, ventricular tachycardia.
2. Inferior MI: Sinus bradycardia, AV blocks, atrial fibrillation.
3. Right ventricular MI: High-degree AV blocks requiring temporary pacing.
Pharmacological Considerations
1. Morphine may increase mortality in NSTEMI due to delayed antiplatelet absorption.
2. Beta-blockers should be used cautiously in acute phase if hemodynamic instability.
3. ACE inhibitors are beneficial if EF <40% but may worsen outcomes if started too early.
Special Populations
1. Women: More likely to have atypical symptoms and worse outcomes.
2. Elderly: Higher mortality and complication rates, often present with dyspnea rather than chest pain.
3. Diabetics: Higher incidence of silent MI and worse long-term prognosis.
